ORIGINAL RESEARCH article
Revisiting false-positive and imitated dissociative identity disorder.

- Research Centre for Trauma & Dissociation, SWPS University of Social Sciences and Humanities, Katowice, Poland
ICD-10 and DSM-5 do not provide clear diagnosing guidelines for DID, making it difficult to distinguish ‘genuine’ DID from imitated or false-positive cases. This study explores meaning which patients with false-positive or imitated DID attributed to their diagnosis. 85 people who reported elevated levels of dissociative symptoms in SDQ-20 participated in clinical assessment using the Trauma and Dissociation Symptoms Interview, followed by a psychiatric interview. The recordings of six women, whose earlier DID diagnosis was disconfirmed, were transcribed and subjected to interpretative phenomenological analysis. Five main themes were identified: (1) endorsement and identification with the diagnosis. (2) The notion of dissociative parts justifies identity confusion and conflicting ego-states. (3) Gaining knowledge about DID affects the clinical presentation. (4) Fragmented personality becomes an important discussion topic with others. (5) Ruling out DID leads to disappointment or anger. To avoid misdiagnoses, clinicians should receive more systematic training in the assessment of dissociative disorders, enabling them to better understand subtle differences in the quality of symptoms and how dissociative and non-dissociative patients report them. This would lead to a better understanding of how patients with and without a dissociative disorder report core dissociative symptoms. Some guidelines for a differential diagnosis are provided.

Introduction
Multiple Personality Disorder (MPD) was first introduced in DSM-III in 1980 and re-named Dissociative Identity Disorder (DID) in subsequent editions of the diagnostic manual ( American Psychiatric Association, 2013 ). Table 1 shows diagnostic criteria of this disorder in ICD-10, ICD-11, and DSM-5. Some healthcare providers perceive it as fairly uncommon or associated with temporary trends ( Brand et al., 2016 ). Even its description in ICD-10 ( World Health Organization, 1993 ) starts with: “This disorder is rare, and controversy exists about the extent to which it is iatrogenic or culture-specific” (p. 160). Yet, according to the guidelines of the International Society for the Study of Trauma and Dissociation ( International Society for the Study of Trauma and Dissociation, 2011 ), the prevalence of DID in the general population is estimated between 1 and 3%. The review of global studies on DID in clinical settings by Sar (2011) shows the rate from 0.4 to 14%. However, in studies using clinical diagnostic interviews among psychiatric in-patients, and in European studies these numbers were lower ( Friedl et al., 2000 ). The discrepancies apparently depend on the sample, the methodology and diagnostic interviews used by researchers.
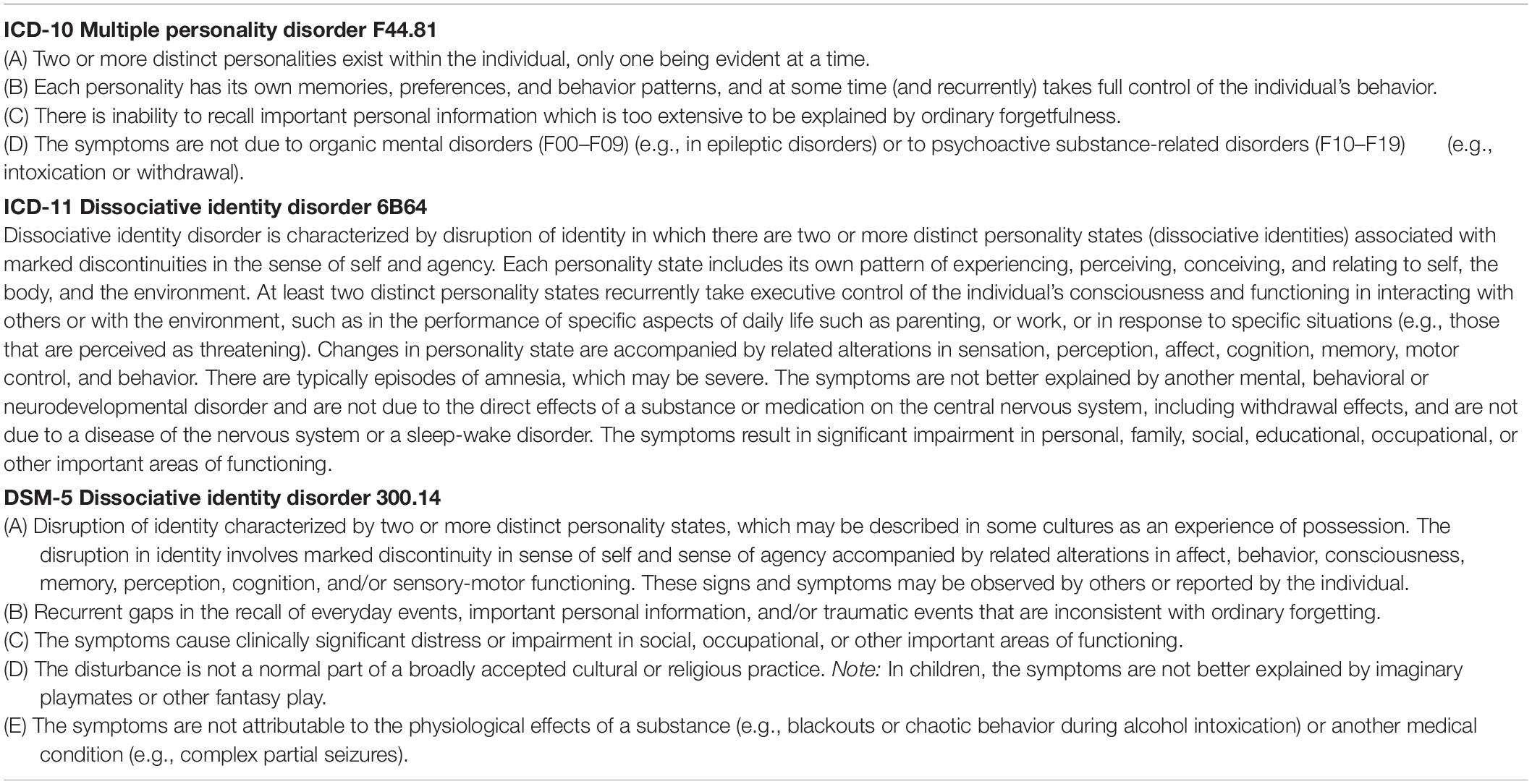
Table 1. Diagnostic criteria for dissociative identity disorder.
Diagnosing complex dissociative disorders (DID or Other Specified Dissociative Disorder, OSDD) is challenging for several reasons. Firstly, patients present a lot of avoidance and rarely report dissociative symptoms spontaneously without direct questioning ( Boon and Draijer, 1993 ; International Society for the Study of Trauma and Dissociation, 2011 ; Dorahy et al., 2014 ). In addition, standard mental state examination does not include these symptoms and healthcare professionals do not receive appropriate training in diagnosing dissociative disorders ( Leonard et al., 2005 ). Secondly, complex dissociative disorders are polysymptomatic, and specialists would rather diagnose these patients with disorders more familiar to them from clinical practice, e.g., anxiety disorders, eating disorders, schizophrenia, or borderline personality disorder ( Boon and Draijer, 1995 ; Dell, 2006 ; Brand et al., 2016 ). For these reasons, complex dissociative disorders are underdiagnosed and often mis-diagnosed. For example, 26.5–40.8% of DID patients would already have been diagnosed and treated for schizophrenia ( Putnam et al., 1986 ; Ross et al., 1989 ). On the other hand, because there is so much information about DID in the media (Hollywood productions, interviews and testimonies published on YouTube, blogs), people who are confused about themselves and try to find an accurate diagnosis for themselves may learn about DID symptoms on the Internet, identify themselves with the disorder, and later (even unintentionally) report core symptoms in a very convincing way ( Draijer and Boon, 1999 ). This presents a risk of making a false positive diagnosis, which is unfavorable for the patient, because using treatment developed for DID with patients without autonomous dissociative parts may be inefficient or even reinforce their pathology.
Authors who wrote about patients inappropriately diagnosed with this disorder used terms such as ‘malingering’ or ‘factitious’ DID ( Coons and Milstein, 1994 ; Thomas, 2001 ). According to Draijer and Boon (1999) , both labels imply that patients intentionally simulate symptoms, either for external gains (financial benefits or justification for one’s actions in court) or for other forms of gratification (e.g., interest from others), while in many cases their motivation is not fully conscious. Getting a DID diagnosis can also provide structure for inner chaos and incomprehensible experiences, and be associated with hope and belief it is real. On the other hand, diagnostic errors often result in inappropriate treatment plans and procedures.
Already in 1995 Boon and Draijer stressed that a growing number of people self-diagnosed themselves based on information from literature and the Internet, and reported symptoms by the book during psychiatric or psychological assessment. Based on their observation of 36 patients in whom DID had been ruled out after applying the structured clinical interview SCID-D, these clinicians identified differences between genuine and imitated DID. They classified their participants into three groups: (1) borderline personality disorder, (2) histrionic personality disorder, or (3) persons with severe dissociative symptoms but not DID. Participants in that study reported symptoms similar to DID patients, including: amnesia (but only for unacceptable behavior), depersonalisation, derealisation, identity confusion, and identity alteration. However, they presented themselves and interacted with the therapist in very different ways. While DID patients are usually reluctant to talk about their symptoms and experience their intrusions as shameful, people who imitated DID were eager to present their problems, sometimes in an exaggerated way, in an attempt to convince the clinician that they suffered from DID ( Boon and Draijer, 1995 ; Draijer and Boon, 1999 ). Similar observations were expressed by Thomas (2001) saying that people with imitated DID can present their history chronologically, using the first person even when they are highly distressed or allegedly presenting an altered personality, and are comfortable with disclosing information about experiences of abuse. They can talk about intrusions of dissociative parts, hearing voices or difficulties controlling emotions, without shame.
Unfortunately, ICD-10, ICD-11, and DSM-5 offer no specific guidelines on how to differentiate patients with personality disorders and dissociative disorders by the manner in which they report symptoms. There are also limited instruments to distinguish between false-positive and false-negative DID. From the clinical perspective, it is also crucial to understand the motives for being diagnosed with DID, and disappointment when this diagnosis is disconfirmed. Accurate assessment can contribute to developing appropriate psychotherapeutic procedures ( Boon and Draijer, 1995 ; Draijer and Boon, 1999 ). Apart from observations already referred to earlier in this article, there are no qualitative analyses of false-positive DID cases in the past 20 years. Most research was quantitative and compared DID patients and simulators in terms of cognitive functions ( Boysen and VanBergen, 2014 ). This interpretative phenomenological analysis is an idiographic study which explores personal experiences and meaning attributed to conflicting emotions and behaviors in six women who had previously been diagnosed with DID and referred to the Research Centre for Trauma and Dissociation for re-evaluation. It explores how they came to believe they have DID and what had led clinicians to assume that these patients could be suffering from this disorder.
Materials and Methods
This study was carried out in Poland in 2018 and 2019. Rich qualitative material collected during in-depth clinical assessments was subjected to the interpretative phenomenological analysis (IPA), a popular methodological framework in psychology for exploring people’s personal experiences and interpretations of phenomena ( Smith and Osborn, 2008 ). IPA was selected to build a deeper understanding of how patients who endorsed and identified with dissociative identity disorder made sense of the diagnosis and what it meant for them to be classified as false-positive cases during reassessment.
Interpretative phenomenological analysis uses phenomenological, hermeneutic, and idiographic principles. It employs ‘double hermeneutics,’ in which participants share their experiences and interpretations, followed by researchers trying to make sense and comment on these interpretations. IPA uses small, homogenous, purposefully selected samples, and data are carefully analyzed case-by-case ( Smith and Osborn, 2008 ; Pietkiewicz and Smith, 2014 ).
This study is part of a larger project examining alterations in consciousness and dissociative symptoms in clinical and non-clinical groups, held at the Research Centre for Trauma & Dissociation, financed by the National Science Centre, and approved by the Ethical Review Board at the SWPS University of Social Sciences & Humanities. Potential candidates enrolled themselves or were registered by healthcare providers via an application integrated with the website www.e-psyche.eu . They filled in demographic information and completed online tests, including: Somatoform Dissociation Questionnaire (SDQ-20, Pietkiewicz et al., 2018 ) and Trauma Experiences Checklist ( Nijenhuis et al., 2002 ). Those with elevated SDQ-20 scores (above 28 points) or those referred for differential diagnosis were consulted and if dissociative symptoms were confirmed, they were invited to participate in an in-depth clinical assessment including a series of interviews, video-recorded and performed at the researcher’s office by the first author who is a psychotherapist and supervisor experienced in the dissociation field. In Poland, there are no gold standards for diagnosing dissociative disorders. The first interview was semi-structured, open-ended and explored the patient’s history, main complaints and motives for participation. It included questions such as: What made you participate in this study? What are your main difficulties or symptoms in daily life? What do you think caused them? Further questions were then asked to explore participants’ experiences and meaning-making. This was followed by the Trauma and Dissociation Symptoms Interview (TADS-I, Boon and Matthess, 2017 ). The TADS-I is a new semi-structured interview intended to identify DSM-5 and ICD-11 dissociative disorders. The TADS-I differs in several ways from other semi-structured interviews for the assessment of dissociative disorders. Firstly, it includes a significant section on somatoform dissociative symptoms. Secondly, it includes a section addressing other trauma-related symptoms for several reasons: (1) to obtain a more comprehensive clinical picture of possible comorbidities, including symptoms of PTSD and complex PTSD, (2) to gain a better insight into the (possible) dissociative organization of the personality: patient’s dissociative parts hold many of these comorbid symptoms and amnesia, voices or depersonalisation experiences are often associated with these symptoms; and (3) to better distinguish between complex dissociative disorders, personality disorders and other Axis I disorders and false positive DID. Finally, the TADS-I also aims to distinguish between symptoms of pathological dissociation indicating a division of the personality and symptoms which are related to a narrowing or a lowering of consciousness, and not to the structural dissociation of the personality. Validation testing of the TADS-I is currently underway. TADS interviews ranging from 2 to 4 h were usually held in sessions of 90 min. Interview recordings were assessed by three healthcare professionals experienced in the dissociation field, who discussed each case and consensually came up with a diagnosis based on ICD-10. An additional mental state examination was performed by the third author who is a psychiatrist, also experienced in the differential diagnosis of dissociative disorders. He collected medical data, double-checked the most important symptoms, communicated the results and discussed treatment indications. Qualitative data collected from six patients out of 85 were selected for this interpretative phenomenological analysis, based on the following criteria for inclusion, which could ensure a homogenous sample expected of IPA studies – (a) female, (b) previously diagnosed or referred to rule in/out DID, (c) endorsement and identification with DID, (d) dissociative disorder disconfirmed in the assessment. Interviews with every participant in this study ranged from 3 h 15 min to 7 h 20 min (mean: 6 h).
Participants
Participants of this IPA were six female patients aged between 22 and 42 years who were selected out of 86 people examined in a larger study exploring dissociation and alterations in consciousness in clinical and non-clinical groups. (Participants in the larger study met criteria of different diagnoses and seven among them had ‘genuine’ DID). These six patients did not meet DID criteria on the TADS-I interview but believed themselves that they qualified for that diagnosis. Four of them had higher education, two were secondary school graduates. All of them registered in the study by themselves hoping to confirm their diagnosis but two (Olga and Katia) were referred by psychiatrists, and the others by psychotherapists. All of them traveled from far away, which showed their strong motivation to participate in the assessment. Four had previously had psychiatric treatment and five had been in psychotherapy due to problems with emotional regulation and relationships. In the cases of Victoria and Dominique, psychotherapy involved working with dissociative parts. None of them recalled any physical or sexual abuse, but three (Dominique, Victoria, and Mary), following therapists’ suggestions, were trying to seek such traumatic memories to justify their diagnosis. They all felt emotionally neglected by carriers in childhood and emotionally abused by significant others. None of them reported symptoms indicating the existence of autonomous dissociative parts. None had symptoms indicating amnesia for daily events, but four declared not remembering single situations associated with conflicting emotions, shame, guilt, or conversations during which they were more focused on internal experiences rather than their interlocutors. None experienced PTSD symptoms (e.g., intrusive traumatic memories and avoidance), autoscopic phenomena (e.g., out-of-body experiences), or clinically significant somatoform symptoms. None had auditory verbal hallucinations but four intensely engaged in daydreaming and experienced imagined conversations as very real. All of them had been seeking information about DID in literature and the Internet. For more information about them see Table 2 . Their names have been changed to protect their confidentiality.
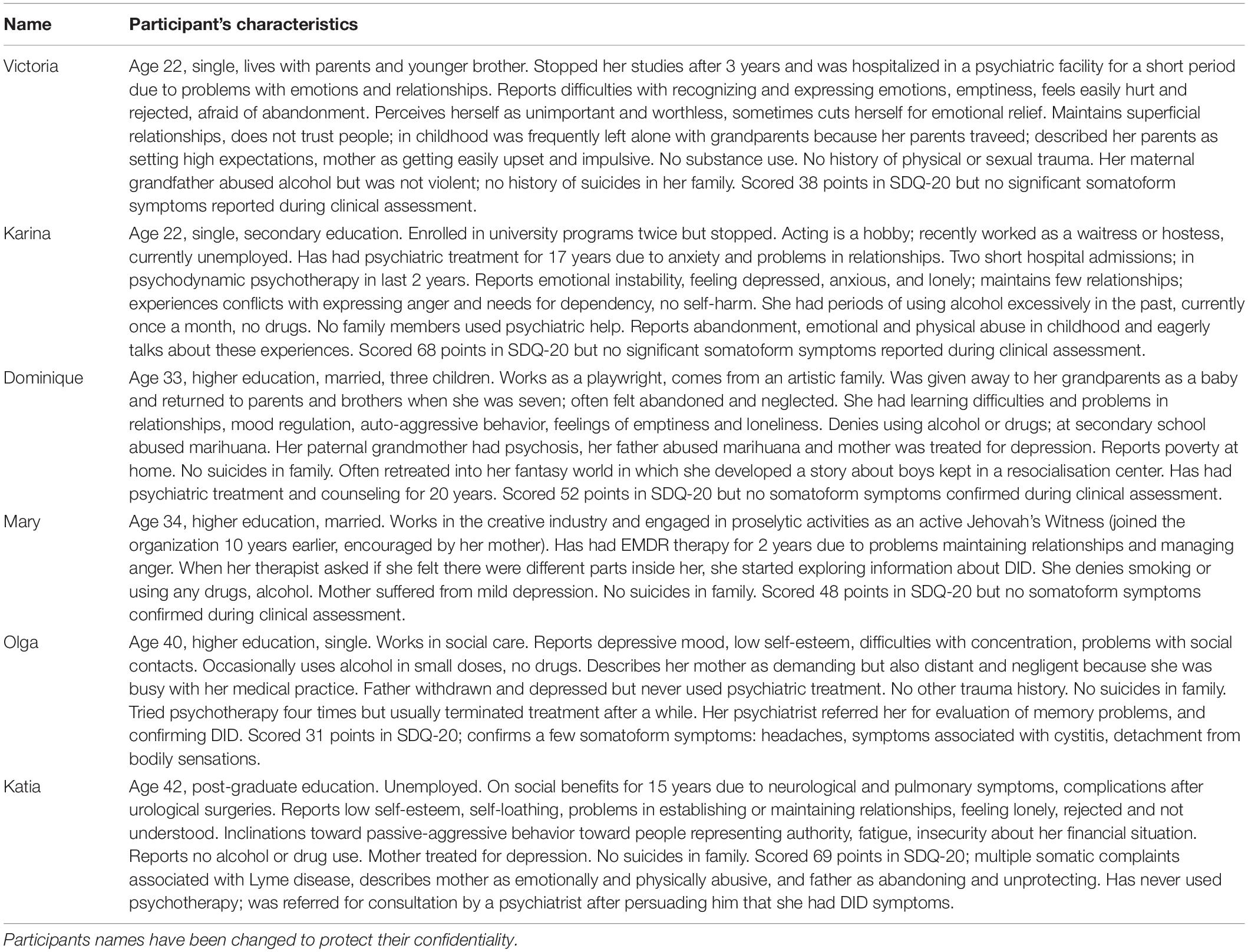
Table 2. Study participants.
The Researchers
The principal investigator (IJP) is a psychotherapist, supervisor, and researcher in the field of community health psychology and clinical psychology. The second co-investigator (RT) is a psychiatrist, psychotherapist, and supervisor. The third co-investigator (SB) is a clinical psychologist, psychotherapist, supervisor, and a consulting expert in forensic psychology, who also developed the TADS-I. They are all mentors and trainers of the European Society for Trauma and Dissociation, with significant expertise in the assessment of post-traumatic conditions. The first co-investigator (AB) has a master’s degree in psychology and is a Ph.D. candidate. She is also a psychotherapist in training. All authors coded and discussed their understanding of data. Their understanding and interpretations of symptoms reported by participants were influenced by their background knowledge and experience in diagnosing and treating patients with personality disorders and dissociative disorders.
Data Analysis
Verbatim transcriptions were made of all video recordings, which were analyzed together with researchers’ notes using qualitative data-analysis software – NVivo11. Consecutive analytical steps recommended for IPA were employed in the study ( Pietkiewicz and Smith, 2014 ). For each interview, researchers watched the recording and carefully read the transcript several times. They individually made notes about body language, facial expressions, the content and language use, and wrote down their interpretative comments using the ‘annotation’ feature in NVivo10. Next, they categorized their notes into emergent themes by allocating descriptive labels (nodes). The team then compared and discussed their coding and interpretations. They analyzed connections between themes in each interview and between cases, and grouped themes according to conceptual similarities into main themes and sub-themes.
Credibility Checks
During each interview, participants were encouraged to give examples illustrating reported symptoms or experiences. Clarification questions were asked to negotiate the meaning participants wanted to convey. At the end of the interview, they were also asked questions to check that their responses were thorough. The researchers discussed each case thoroughly and also compared their interpretative notes to compare their understanding of the content and its meaning (the second hermeneutics).
Participants in this study explained how they concluded they were suffering from DID, developed knowledge about the syndrome and an identity of a DID patient, and how this affected their everyday life and relationships. Five salient themes appeared in all interviews, as listed in Table 3 . Each theme is discussed and illustrated with verbatim excerpts from the interviews, in accordance with IPA principles.
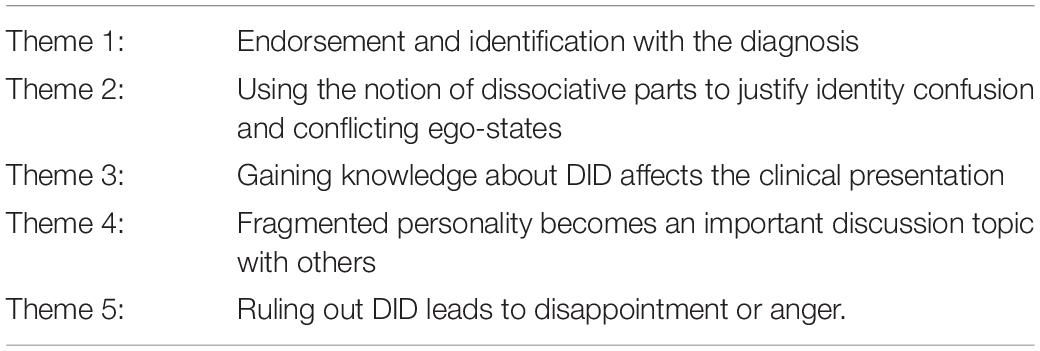
Table 3. Salient themes identified during the interpretative phenomenological analysis.
Theme 1: Endorsement and Identification With the Diagnosis
All six participants hoped to confirm they had DID. They read books and browsed the Internet seeking information about dissociation, and watched YouTube videos presenting people describing multiple personalities. Dominique, Victoria, Mary, and Karina said that a mental health professional suggested this diagnosis to them. Dominique remembers consulting a psychiatrist when she was 15, because she had problems controlling anger at home or in public places. She initially found descriptions of borderline personality captured her experiences well enough, but a psychiatrist refuted the idea and recommended further diagnostics toward a dissociative disorder. However, the girl refused to go to hospital for observation.
During an argument with my mother I felt as if some incredible force took control and I smashed the glass in the cabinet with my hand. It was like being under control of an alien force. I started reading about borderline and I thought I had it. I found a webpage about that and told my mother I should see a psychiatrist. I went for a consultation and told her my story. This lady said: “Child, you don’t have borderline, but multiple personality.” She wanted to keep me in the psychiatric unit but I did not agree to stay for observation. (Dominique).
This led Dominique to research the new diagnosis. Karina also said she was encouraged to seek information about DID, when a doctor suggested she might be suffering with it.
When I was 11, I had problems at school and home. Other children made fun of me. My mom took me to a doctor and he said I had borderline, but later I was diagnosed with an anxiety disorder. That doctor also suggested I had DID and told me that I should read more about this diagnosis. (Karina).
Victoria and Mary shared similar stories about psychotherapists suggesting the existence of dissociative parts, having readily accepted this new category as a good explanation for aggressive impulses or problems with recalling situations evoking guilt or shame. Dominique and Victoria stressed, however, that, apart from feeling emotionally abandoned, they could not trace any significant traumas in their early childhoods, although therapists maintained that such events must be present in dissociative patients.
I have no idea why I have this [DID]. My therapist looked for evidence of childhood trauma, which sounds like the easiest explanation, but I don’t feel I had any horrific memories which I threw out of my consciousness. (Victoria).
Katia and Olga had used psychiatric treatment for anxiety and depression for years. After exploring information about different mental disorders they concluded they had DID. They thought there was a similarity between their personal experiences and those of people publishing testimonials about multiple personalities.
I tried to understand this battle inside, leading me to stagnation. I didn’t know how to describe that but I recently bought a book Healing the fragmented selves of trauma survivors , and everything was explained there. Some of these things I have discovered myself and some were new to me. (Olga).
Subsequently, Katia presented to her doctor a review of literature about DID, trying to persuade him that she had this disorder.
Theme 2: Using the Notion of Dissociative Parts to Justify Identity Confusion and Conflicting Ego-States
Once participants had embraced the idea of having multiple personalities, they seemed to construct inner reality and justify conflicting needs, impulses or behaviors as an expression of dissociative parts. They referred to being uncertain about who they were and having difficulties recognizing personal emotions, needs or interests. Some of them felt it was connected to a negative cognition about themselves as worthless, unimportant, and not deserving to express what they felt or wanted. Victoria said she would rather define herself through the eyes of others:
My therapist asked what I wanted or needed. It turned out that without other people’s expectations or preferences to which I normally adjust, I wouldn’t know who I am or what I want. I usually engage in my friends’ hobbies and do what I think gives them pleasure. Otherwise, I think they will not like me and reject me, because I have nothing to offer. (Victoria).
Since a young age, Dominique tended to immerse herself in a fantasy world, developing elaborated scenarios about people living in a youth center administered by a vicious boss. Different characters in her ‘Story’ represented specific features, interests and plans she had.
Well, there is John who is a teacher and researcher. He teaches mathematics. I have no skills in maths at all. Tim is a philosopher and would like to train philosophers, enroll doctoral studies. He would like me to study philosophy but the rest of the system wants me to be a worrier. Ralf is a caring nurse and would like to become a paramedic. It is difficult to reconcile all these different expectations. Whoever comes up front, then I have these ideas. (Dominique).
Dominique neither had amnesia nor found evidence for leading separate lives and engaging herself in activities associated with her characters. She maintained her job as a playwright, and merely imagined alternative scenarios of her life, expressed by her inner heroes. In other parts of the interview, she referred to them as ‘voices inside,’ but admitted she never heard them acoustically. They were her own vivid thoughts representing different, conflicting opinions or impulses.
Katia said she felt internally fragmented. There were times when she engaged in certain interests, knowledge and skills, but she later changed her goals. Fifteen years ago she gave up her academic career and went on sickness benefit when she became disabled due to medical problems; she experienced this as a great loss, a failure, which affected her sense of identity and purpose.
In recent years I have a growing sense of identity fragmentation. I have problems with defining my identity because it changes. I used to feel more stable in the past. I had these versions of myself which were more dominating, so I had a stronger sense of identity. For example, 20 years ago there was this scientist. I was studying and felt like a scientist, attending conferences. Now I don’t have that and I don’t know who I am. […] I also have changing interests and hobbies because of different personalities. Long ago I liked certain music, played the guitar, sang songs. I don’t do that anymore, I suddenly lost interest in all that. (Katia).
She described changes in her professional and social lives in terms of switches between dissociative parts. Although she maintained the first person narrative (“I was studying,” “I played,” or “I sang”), indicating some sense of continuity, she thought it proved the existence of two or more distinct personalities.
Participants also reported thoughts, temptations, impulses or actions which seemed to evoke conflicting feelings. Attributing them to ‘something inside that is not-me’ could free them from guilt or shame, so they used a metaphor of someone taking over, logging in, or switching. Dominique thought it was inappropriate to express disappointment or anger, but she accepted the thought that her dissociative parts were doing this.
When I’m angry at my therapist, it is not really me but somebody inside who gets angry easily. Greg often switches on in such situations and says: “Tell her this and this”. […] I went to a shop once and discovered that the price on the label was not for a whole package of batteries but a single one. And suddenly Greg switched on and had a row with the cashier. I mean, I did it, but wound up by his anger. This is so weird, I wouldn’t react like that. They just charged incorrectly and I would normally ignore that but Greg said: “I give a shit about their mistakes. I won’t accept that.” What a failure! (Dominique).
Mary said she had parts that expressed anger, sadness, and needs associated with attachment. She observed them and allowed them to step in, when situations required.
There were situations in my life when the teenager must have been active. She protected me. She is ready to fight; I am not like that at all. I hate violence, and that teenager likes using force to protect me. […] My therapist suggested I call her after this interview if I do not feel well. I didn’t accept that but the [inner] girls got upset and told me I needed her help. They made me comply, so I agreed to call her if I do not feel well. It has always been like this. (Mary).
During assessment, no participant provided evidence for the existence of autonomous dissociative parts. It seems that the inner characters described by them personified unintegrated ego-states which used to evoke conflicting feelings.
Theme 3: Exploring Personal Experiences via the Lens of Dissociation
Reading books, websites and watching videos of people who claimed to have DID, encouraged them to compare themselves, talk about and express ‘multiple personalities.’ The participants became familiar with specialist terms and learned about core symptoms mentioned in psychiatric manuals.
I read First person plural which helped me understand what this is all about. The drama of the gifted child and The body keeps the score . More and more girls started to appear. There is a 6-month old baby which showed up only 2 months ago, a sad 11-year old teenager, and a 16-year old who thinks I am a loser. I was a teenager like that. Now she is having problems and becoming withdrawn there are fewer switches, because she knows we need to help the little one first. (Mary).
Olga was also inspired by books. Not only did she find similarities to trauma survivors but she made new discoveries and thought there were other experiences she had been unaware of earlier. Victoria started using techniques which literature recommended for stabilization in dissociative disorders. She said these books helped her understand intense emotions and improve concentration.
This explains everything that happens to me, why I get so angry. I also found anchors helpful. I focus on certain objects, sounds or smells which remind me where I am, instead of drifting away into my thoughts. (Victoria).
It seemed that exploring information about DID encouraged changes in participants’ clinical presentation. At first, they merely struggled with emotional liability or detachment, internal conflicts, and concentration problems. Later, they started reporting intrusions of dissociative parts or using clinical terms (e.g., flashback) for experiences which were not necessarily clinical symptoms. Dominique said that the characters of her story would often ‘log in’ and take control. She demonstrated that during the interview by changing her voice and going into a ‘trance.’ She created her own metaphors, explaining these experiences and comparing them with those described in literature. She stressed that she never had amnesia and remained aware of what was happening during her ‘trance.’
I think it is a form of dissociation on the emotional level. I read a lot… The minds of Billy Milligan or First person plural . For sure, I do not have an alteration of personality. I have co-consciousness. My theory is, we are like a glove, we all stem from one trunk, but we are like separate fingers. (Dominique).
While participants maintained they had flashbacks, they understood them as sudden recollections of past memories but not necessarily related to trauma. Katia said she recently remembered the picture of the house and garden where she played as a child and associated these experiences with moments of joy. Karina also exemplified her flashbacks with ‘intrusions of happy memories’ which belonged to other personalities:
Sometimes I begin to laugh but this is not my laughter, but the laughter of sheer joy. Someone inside me is very happy and wants to talk about happy childhood memories, make jokes. (Karina).
Mary said a child part of her was responsible for flashbacks and making comments about current situations. However, she later denied hearing voices or having any other Schneider’s symptoms.
I can hear her comments, that she does not like something. I can be flooded by emotions and have flashbacks associated with that child. For example, there is a trigger and I can see things that this child has seen. She is showing me what was happening in her life. (Mary).
Participants discussed their dissociative parts, their names and features, exhibiting neither avoidance nor fear or shame. On the contrary, they seemed to draw pleasure by smiling, showing excitement and eagerness to produce more examples of their unusual experiences. At the beginning of the interview, Karina was very enthusiastic and said, “My heart is beating so fast, as if I were in fight-or-flight mode.”
Theme 4: Talking About DID Attracts Attention
Not only were multiple personalities a helpful metaphor for expressing conflicting feelings or needs (already mentioned in Theme 2), but they also became an important topic of conversations with family or friends.
My husband says sometimes: “I would like to talk to the little girl.” He then says that I start behaving differently. I also talk to my therapist using different voices. Sometimes, she addresses them asking questions. If questions are asked directly, they respond, but there are times I do not allow them to speak, because the teenager part can be very mean and attacks people. (Mary).
It may have been easier for Mary to express her needs for dependency and care by ascribing them to a little girl and, because she felt awkward about feeling angry with the therapist, attributing hostile impulses to a teenager could give her a sense of control and reduce guilt. Karina decided to create a video-blog for documenting dissociative parts, and shared her videos with people interested in DID. She said she was surprised to find clips in which she looked dreadful, having her make-up smeared all over the face, because she had no memory of doing that. However, she showed no signs that it bothered her. She discussed the videos with her best friend, a DID fan who had encouraged her to enroll in the study in order to confirm her diagnosis. They were collecting evidence to support the idea that she had a dissociative disorder, which she presented one by one, before being asked about details.
Mark [her friend] reads a lot about DID. He says I sometimes talk in a high voice which is not the way I usually talk. He refers to us as plural. […] In some of these videos I do not move or blink for a minute. I look at some point and there is no expression on my face. I can remember things until this moment, and later I discover myself looking like something from Creepypastas. I am so sorry for people who have to see this… and I found my diary. I have been writing diaries since I was seven. I sometimes have no memory for having written something. I need to find these notes because I would like to write a book about a fantasy world and inner conflicts. (Karina).
Dominique and Katia also wrote journals to record dissociative experiences. Katia hoped to be recognized as an expert-by-experience and develop her career in relation to that. She brought with her a script of a book she hoped to publish 1 day.
Theme 5: Ruling Out DID Leads to Disappointment or Anger
Four participants were openly disappointed that their DID diagnosis was not confirmed. They doubted if their descriptions were accurate enough, or they challenged the interviewer’s understanding of the symptoms. Katia also suggested that she was incapable of providing appropriate answers supporting her diagnosis due to amnesia and personality alterations.
Do you even consider that I might give different answers if you had asked these questions 2 or 5 years ago? I must have erased some examples from my memory and not all experiences belong to me. I know that people can unconsciously modify their narratives and that is why I wanted an objective assessment. […] Nobody believed I was resistant to anesthetics until I was diagnosed with some abnormalities. It was once written in my medical report that I was a hypochondriac. One signature and things become clear to everyone. Sometimes it is better to have the worst diagnosis, but have it. (Katia).
She expected that the diagnosis would legitimize her inability to establish satisfactory relationships, work, and become financially independent. For this reason, she also insisted that the final report produced for her should contain information about how she felt maltreated by family or doctors, and revealed her hopes to claim damages for health injury. Mary and Karina were also upset that the interviewers did not believe they had DID.
Can you try to imagine how hard it is? I am not making things up? You don’t believe me. I am telling you things and you must be thinking, from the adult perspective: “You are making this up.” Nothing pisses me off more than someone who is trying to prove to others that they have just imagined things. They [dissociative parts] feel neglected again, as always! (Mary).
Karina tried to hide her disappointment and claimed she was glad she didn’t have a severe mental illness. However, she thought she would need to build another theory explaining her symptoms. After the interview, she sent more videos trying to prove the assessment results were not accurate.
What about my problems then? I am unable to set boundaries, I have anxiety, I fear that a war might break out. If this is not dissociation, then what? I had tests and they ruled out any neurological problems. I came here and ruled out another possibility. It is some information but I have not heard anything new. (Karina).
Only Victoria seemed relieved that her DID diagnosis was not confirmed. She was happy to discuss how attachment problems or conflicts with expressing emotions and needs affected her social life and career, and receive guidelines for future treatment. She felt liberated from having to uncover childhood traumas that her therapist expected her to have as a dissociative patient.
I was hoping that you would find another explanation for my problems… for what is wrong with me, why I feel so sensitive or spaced out, because it is annoying. I would like to know what is going on. I don’t think I’ve had any severe trauma but everybody wants to talk about trauma all the time. (Victoria).
ICD-10 and DSM-5 provide inadequate criteria for diagnosing DID, basically limited to patients having distinct dissociative identities with their own memories, preferences and behavioral patterns, and episodes of amnesia ( American Psychiatric Association, 2013 ; World Health Organization, 1993 ). Clinicians without experience of DID may therefore expect patients to present disruptions of identity during a consultation and spontaneously report memory problems. However, trauma specialists view DID as a ‘disorder of hiddenness’ because patients often find their dissociative symptoms bizarre and confusing and do not disclose them readily due to their shame and the phobia of inner experiences ( Steele et al., 2005 , 2016 ; Van der Hart et al., 2006 ). Instead, they tend to undermine their significance, hide them and not report them during consultations unless asked about them directly. Dissociative patients can also be unaware of their amnesia and ignore evidence for having done things they cannot remember because realizing that is too upsetting. Contrary to that, this study and the one conducted in 1999 in the Netherlands by Draijer and Boon, show that some people with personality disorders enthusiastically report DID symptoms by the book, and use the notion of multiple personalities to justify problems with emotional regulation, inner conflicts, or to seek attention. As with Dutch patients, Polish participants were preoccupied with their alternate personalities and two tried to present a ‘switch’ between parts. Their presentations were naïve and often mixed with lay information on DID. However, what they reported could be misleading for clinicians inexperienced in the dissociation field or those lacking the appropriate tools to distinguish a genuine dissociative disorder from an imitated one.
Therefore, understanding the subtleties about DID clinical presentation, especially those which are not thoroughly described in psychiatric manuals, is important to come up with a correct diagnosis and treatment plan. Various clinicians stress the importance of understanding the quality of symptoms and the mechanisms behind them in order to distinguish on the phenomenological level between borderline and DID patients ( Boon and Draijer, 1993 ; Laddis et al., 2017 ). Participants in this study reported problems with identity, affect regulation and internal conflicts about expressing their impulses. Some of them also had somatic complaints. These symptoms are common in personality disorders and also in dissociative disorders, which are polysymptomatic by nature. However, the quality of these symptoms and psychological mechanisms behind them may be different. For a differential diagnosis, clinicians need to become familiar with the unique internal dynamics in people who have developed a structural dissociation of personality as a result of trauma. These patients try to cope with everyday life and avoid actively thinking about and discussing traumatic memories, or experiencing symptoms associated with them. Because of that avoidance, they find it challenging to talk about dissociative symptoms with a clinician. Besides experiencing fear of being labeled as insane and sent to hospital, there may be internal conflicts associated with disclosing information. For example, dissociative parts may forbid them to talk about symptoms or past experiences. This conflict can sometimes be indicated by facial expression, involuntary movements, spasms, and also felt by the clinician in his or her countertransference. In other words, it is not only what patients say about their experiences, but how they do this. Therapists’ observations and countertransference may help in assessing the quality of avoidance: How openly or easily do patients report symptoms or adverse life experiences? Is that associated with strong depersonalisation (detachment from feelings and sensations, being absent)? Is there evidence for internal conflicts, shame, fear or feeling blocked when talking about symptoms (often observed in facial expression, tone of voice)? Participants in this study were eager to talk about how others mistreated them and wanted to have that documented on paper. Difficult experiences in the past sometimes triggered intense emotions in them (anger, resentment, and deep sadness) but they did not avoid exploring and communicating these states. On the contrary, they eagerly shared an elaborate narrative of their sorrows and about their inner characters – the multiple personalities they were convinced they had. They became keen on DID and used a variety of resources to familiarize themselves with core symptoms. They also spontaneously reported them, as if they wanted to provide sound evidence about having DID and were ready to defend their diagnosis. Some planned their future based on it (an academic career, writing a book, or a film). During the interviews, it became clear that some perceived having an exotic diagnosis as an opportunity for seeking attention and feeling unique, exhibiting the drama of an ‘unseen child’ (see section “Theme 4”).
Understanding a few of the symptoms identified in this study can be useful for differential diagnosis: intrusions, voices, switches, amnesia, use of language, depersonalisation. How they are presented by patients and interpreted by clinicians is important.
Triggered by external or internal factors (memories or anything associated with trauma) dissociative patients tend to relive traumatic experiences. In other words, they have intrusive memories, emotions or sensorimotor sensations contained by dissociative parts which are stuck in trauma. In addition to avoidance, this is another characteristic PTSD feature observed in the clinical presentation of DID patients ( Van der Hart et al., 2010 ). Interestingly, participants in this study showed no evidence for intrusions (images, emotions or somatosensory experiences directly related to trauma), but rather problems with emotional regulation (illustrated in sections “Themes 1 and 2”). Asked about intrusive images, emotions or thoughts, some gave examples of distressing thoughts attacking self-image and blaming for their behavior. This, however, was related to attachment problems and difficulties with self-soothing. They also revealed a tendency to indulge themselves in these auto-critical thoughts instead of actively avoiding them, which is often a case in dissociative patients. Some intrusions reported by DID patients are somatoform in nature and connected with dissociative parts stuck in trauma time ( Pietkiewicz et al., 2018 ). Although three participants in this study had very high scores in SDQ-20 indicating that they may have a dissociative disorder (scores of 50–60 are common in DID), further interviews revealed that they aggravated their symptoms and, in fact, had low levels of somatoform dissociation. This shows that tests results should be interpreted with caution and clinicians should always ask patients for specific examples of the symptoms they report.
It is common for DID patients to experience auditory hallucinations ( Dorahy et al., 2009 ; Longden et al., 2019 ). The voices usually belong to dissociative parts and comment on actions, express needs, likes and dislikes, and encourage self-mutilation. Subsequently, there may be conflicts between ‘voices,’ and the relationship with them is quite complex. Dorahy et al., 2009 observe that auditory hallucinations are more common in DID than in schizophrenia. In dissociative patients they are more complex and responsive, and already appear in childhood. Specifically, child voices are also to be expected in DID (97% in comparison to 6% in psychosis). None of our participants reported auditory hallucinations although one (Dominique) said she had imaginary friends from childhood. While this could sound like a dissociative experience, exploring their experiences showed she had a tendency to absorb herself in her fantasy world and vividly imagine characters in her story (see section “Theme 2”).
Literature also shows that it is uncommon for avoidant dissociative patients to present autonomous dissociative parts to a therapist before a good relationship has been established and the phobia for inner experiences reduced ( Steele et al., 2005 ). Sudden switches between dissociative personalities may occur only when the patient is triggered and cannot exercise enough control to hide his or her symptoms. Two participants in this study (Dominique and Karina) tried to present ‘alternate personalities’ and they actually announced this would happen, so that the interviewer did not miss them. Later on, they could relate to what happened during the alleged switch (no amnesia), maintaining the first-person perspective (I was saying/doing). Contrary to that, dissociative patients experience much shame and fear of disclosing their internal parts ( Draijer and Boon, 1999 ). If they become aware that switches had occurred, they try to make reasonable explanations for the intrusions of parts and unusual behavior (e.g., I must have been very tired and affected by the new medicine I am taking).
Dell (2006) mentions various indicators of amnesia in patients with DID. However, losing memory for unpleasant experiences may occur in different disorders, usually for behaviors evoking shame or guilt, or for actions under extreme stress ( Laddis et al., 2017 ). All patients in this study had problems with emotional regulation and some said they could not remember what they said or did when they became very upset. With some priming, they could recall and describe events. For this reason, it is recommended to explore evidence for amnesia for pleasant or neutral activities (e.g., doing shopping or cleaning, socializing). According to Laddis et al. (2017) there are different mechanisms underlying memory problems in personality and dissociative disorders.
Use of Language
Participants in this study often used clinical jargon (e.g., flashbacks, switches, and feeling depersonalized) which indicates they had read about dissociative psychopathology or received psycho-education. However, they often had lay understanding of clinical terms. A good example in this study was having ‘flashbacks’ of neutral or pleasant situations which had once been forgotten. Examples of nightmares did not necessarily indicate reliving traumatic events during sleep (as in PTSD) but expressed conflicts and agitation through symbolic, unrealistic, sometimes upsetting dreams. When talking about behavior of other parts and their preferences, they often maintained a first-person perspective. Requesting patients to provide specific examples is thus crucial.
Depersonalisation
Detachment from feelings and emotions, bodily sensations and external reality is often present in various disorders ( Simeon and Abugel, 2006 ). While these phenomena have been commonly associated with dissociation, Holmes et al. (2005) stress the differences between detachment (which can be experienced by both dissociative and non-dissociative patients) and compartmentalisation, associated with the existence of dissociative parts. Allen et al. (1999) also stress that extreme absorptive detachment can interfere with noticing feelings and bodily sensations, and also memory. Some participants in this study tended to enter trance-like states or get absorbed in their inner reality, subsequently getting detached from bodily sensations. They also described their feeling of emptiness in terms of detachment from feelings. Nevertheless, none of them disclosed evidence for having distinct dissociative parts. Some of their statements might have been misleading; for example, when they attributed anger attacks to other parts, not-me (see: Dominique in section “Theme 2”). One might suspect it could be evidence for autonomous dissociative parts. However, these participants seem to have had unintegrated, unaccepted self-states and used the concept of DID to make meaning of their internal conflicts. In their narrative they maintained the first-person narrative. None of them provided sound evidence for extreme forms of depersonalisation, such as not feeling the body altogether or out-of-body experiences.
There can be many reasons why people develop symptoms which resemble those typical of DID. Suggestions about a dissociative disorder made by healthcare providers can help people justify and explain inner conflicts or interpersonal problems. In this study several clinicians had suggested a dissociative disorder or DID to the patient. Literature on multiple personalities and therapy focused on them, and using expressions such as ‘parts’, ‘dissociating’, ‘switches,’ can also encourage demonstrating such symptoms. There are also secondary gains explained in this study, such as receiving attention and care. Draijer and Boon (1999) observe that people with borderline features justified shameful behavior and avoided responsibility by attributing their actions to ‘alter personalities.’ Such people can declare amnesia for their outbursts of anger, or hitting partners. Others explained their identity confusion and extreme emptiness using the DID model. All their participants reported emotional neglect and felt unseen in their childhood, so they adopted a new DID-patient identity to fill up inner emptiness ( Draijer and Boon, 1999 ). Just like the participants in this study, they were angry when that diagnosis was disconfirmed during the assessment, as if the clinician had taken away something precious from them. This shows that communicating the results should be done with understanding, empathy and care. Patients and clinicians need to understand and discuss reasons for developing a DID-patient identity, its advantages and pitfalls.
In countries where clinicians are less familiar with the dissociative pathology, there may be a greater risk for both false-negative and false-positive DID diagnoses. The latter is caused by the growing popularity of that disorder in media and social networks. People who try to make meaning of their emotional conflicts, attachment problems and difficulties in establishing satisfactory relationships, may find the DID concept attractive. It is important that clinicians who rule out or disconfirm DID, also provide patients with friendly feedback that encourages using treatment for their actual problems. Nevertheless, this may still evoke strong reactions in patients whose feelings and needs have been neglected, rejected or invalidated by significant others. Disconfirming DID may be experienced by them as an attack, taking something away from them, or an indication that they lie.
Limitations and Further Directions
Among the 85 people who participated in a thorough diagnostic assessment, there were six false-positive DID cases, and this study focused on their personal experiences and meaning attributed to the diagnosis. Because IPA studies are highly idiographic, they are by nature limited to a small number of participants. There were two important limitations in this research. Firstly, information about the level of psychoform symptoms has not been given, because the validation of the Polish instrument used for that purpose is not complete. Secondly, TADS-I used for collecting clinical data about trauma-related symptoms and dissociation has not been validated, either. Because there are no gold standards in Poland for diagnosing dissociative disorders, video-recordings of diagnostic interviews were carefully analyzed and discussed by all authors to agree upon the diagnosis. Taking this into consideration, further qualitative and quantitative research is recommended to formulate and validate more specific diagnostic criteria for DID and guidelines for the differential diagnosis.
Clinicians need to understand the complexity of DID symptoms and psychological mechanisms responsible for them in order to differentiate between genuine and imitated post-traumatic conditions. There are several features identified in this study which may indicate false-positive or imitated DID shown in Table 4 , which should be taken into consideration during diagnostic assessment. In Poland, as in many countries, this requires more systematic training in diagnosis for psychiatrists and clinical psychologists in order to prevent under- and over-diagnosis of dissociative disorders, DID in particular. It is not uncommon that patients exaggerate on self-report questionnaires when they are invested in certain symptoms. In this study, all participants had scores above the cut-off score of 28 on the SDQ-20, a measure to assess somatoform dissociation, which suggested it was probable they had a dissociative disorder. However, during a clinical diagnostic interview they did not report a cluster of somatoform or psychoform dissociative symptoms and did not meet criteria for any dissociative disorder diagnosis. Clinicians also need to go beyond the face value of a patient’s responses, ask for specific examples, and notice one’s own countertransference. Draijer and Boon (1999) observed that DID patients were often experienced by clinicians as very fragile, and exploring symptoms with people with personality disorders (who try to aggravate them and control the interview) can evoke tiredness or even irritability. It is important that clinicians understand their own responses and use them in the diagnostic process.
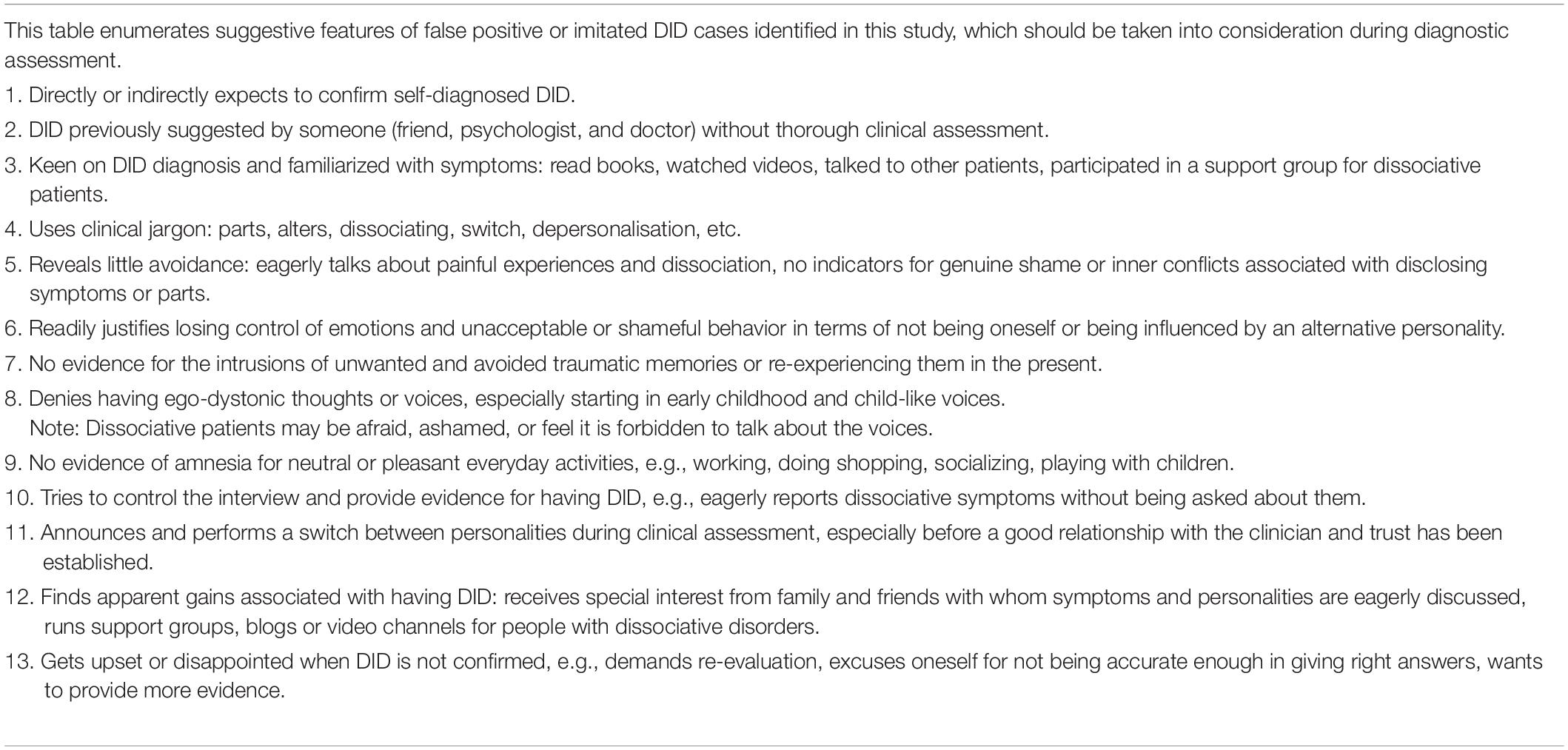
Table 4. Red flags for identifying false-positive or imitated DID.
While psycho-education is considered a crucial element in the initial treatment of dissociative disorders ( Van der Hart et al., 2006 ; Howell, 2011 ; Steele et al., 2016 ), patients whose diagnosis has not been confirmed by a thorough diagnostic assessment should not be encouraged to develop knowledge about DID symptomatology, because this may affect their clinical presentation and how they make meaning of their problems. Subsequently, this may lead to a wrong diagnosis and treatment, which can become iatrogenic.
Data Availability Statement
The datasets generated for this study are not readily available because data contain highly sensitive clinical material, including medical data which cannot be shared according to local regulations. Requests to access the datasets should be directed to IP, [email protected] .
Ethics Statement
The studies involving human participants were reviewed and approved by Ethical Review Board at the SWPS University of Social Sciences and Humanities. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
IP collected qualitative data, performed the analysis, and prepared the manuscript. AB-N transcribed and analyzed the interviews and helped in literature review and manuscript preparation. RT performed psychiatric assessment and helped in data analysis and manuscript preparation. SB helped in data analysis and manuscript preparation. All authors contributed to the article and approved the submitted version.
Grant number 2016/22/E/HS6/00306 was obtained for the study “Interpretative phenomenological analysis of depersonalization and derealization in clinical and non-clinical groups.”
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Allen, J. G., Console, D. A., and Lewis, L. (1999). Dissociative detachment and memory impairment: reversible amnesia or encoding failure? Compre. Psychiatry 40, 160–171. doi: 10.1016/S0010-440X(99)90121-9
CrossRef Full Text | Google Scholar
American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5) , Fifth Edn. Arlington, VA: American Psychiatric Publishing.
Google Scholar
Boon, S., and Draijer, N. (1993). The differentiation of patients with MPD or DDNOS from patients with a cluster B personality disorder. Dissociation 6, 126–135.
Boon, S., and Matthess, H. (2017). Trauma and Dissociation Symptoms Interview (TADS-I), version 1.9.
Boon, S. A., and Draijer, P. J. (1995). Screening en Diagnostiek van Dissociatieve Stoornissen. Lisse: Swets & Zeitlinger.
Boysen, G. A., and VanBergen, A. (2014). Simulation of multiple personalities: a review of research comparing diagnosed and simulated dissociative identity disorder. Clin. Psychol. Rev. 34, 14–28. doi: 10.1016/j.cpr.2013.10.008
PubMed Abstract | CrossRef Full Text | Google Scholar
Brand, B. L., Webermann, A. R., and Frankel, A. S. (2016). Assessment of complex dissociative disorder patients and simulated dissociation in forensic contexts. Int. J. Law Psychiatry 49, 197–204. doi: 10.1016/j.ijlp.2016.10.006
Coons, P. M., and Milstein, V. (1994). Factitious or malingered multiple personality disorder: eleven cases. Dissociation 7, 81–85.
Dell, P. F. (2006). A new model of dissociative identity disorder. Psychiatr. Clin. 29, 1–26. doi: 10.1016/j.psc.2005.10.013
Dorahy, M. J., Brand, B. L., Şar, V., Krüger, C., Stavropoulos, P., Martínez-Taboas, A., et al. (2014). Dissociative identity disorder: an empirical overview. Aust. N. Z. J. Psychiatry 48, 402–417. doi: 10.1177/0004867414527523
Dorahy, M. J., Shannon, C., Seagar, L., Corr, M., Stewart, K., Hanna, D., et al. (2009). Auditory hallucinations in dissociative identity disorder and schizophrenia with and without a childhood trauma history: similarities and differences. J. Nerv. Ment. Dis. 197, 892–898. doi: 10.1097/NMD.0b013e3181c299ea
Draijer, N., and Boon, S. (1999). The imitation of dissociative identity disorder: patients at risk, therapists at risk. J. Psychiatry Law 27, 423–458. doi: 10.1177/009318539902700304
Friedl, M., Draijer, N., and De Jonge, P. (2000). Prevalence of dissociative disorders in psychiatric in−patients: the impact of study characteristics. Acta Psychiatr. Scand. 102, 423–428. doi: 10.1034/j.1600-0447.2000.102006423.x
Holmes, E. A., Brown, R. J., Mansell, W., Fearon, R. P., Hunter, E. C., Frasquilho, F., et al. (2005). Are there two qualitatively distinct forms of dissociation? a review and some clinical implications. Clin. Psychol. Rev. 25, 1–23.
Howell, E. F. (2011). Understanding and Treating Dissociative Identity Disorder: A Relational Approach. New York, NY: Routledge.
International Society for the Study of Trauma and Dissociation (2011). Guidelines for treating dissociative identity disorder in adults, third revision. J. Trauma Dissociation 12, 115–187. doi: 10.1080/15299732.2011.537247
Laddis, A., Dell, P. F., and Korzekwa, M. (2017). Comparing the symptoms and mechanisms of “dissociation” in dissociative identity disorder and borderline personality disorder. J. Trauma Dissociation 18, 139–173.
Leonard, D., Brann, S., and Tiller, J. (2005). Dissociative disorders: pathways to diagnosis, clinician attitudes and their impact. Aust. N. Z, J. Psychiatry 39, 940–946. doi: 10.1080/j.1440-1614.2005.01700.x
Longden, E., Moskowitz, A., Dorahy, M. J., and Perona-Garcelán, S. (2019). Auditory Verbal Hallucinations: Prevalence, Phenomenology, and the Dissociation Hypothesis Psychosis, Trauma and Dissociation: Evolving Perspectives on Severe Psychopathology . (Hoboken, NJ: John Wiley & Sons Ltd.), 207–222.
Nijenhuis, E., van der Hart, O., and Kruger, K. (2002). The psychometric characteristics of the traumatic experiences checklist (TEC): first findings among psychiatric outpatients. Clin. Psychol. Psychother. 9, 200–210. doi: 10.1002/cpp.332
Pietkiewicz, I. J., Hełka, A., and Tomalski, R. (2018). Validity and reliability of the Polish online and pen-and-paper versions of the somatoform dissociation questionnaires (SDQ-20 and PSDQ-5). Eur. J. Trauma Dissociation 3, 23–31. doi: 10.1016/j.ejtd.2018.05.002
Pietkiewicz, I. J., and Smith, J. A. (2014). A practical guide to using interpretative phenomenological analysis in qualitative research psychology. Psychol. J. 20, 7–14. doi: 10.14691/CPPJ.20.1.7
Putnam, F. W., Guroff, J. J., Silberman, E. K., Barban, L., and Post, R. M. (1986). The clinical phenomenology of multiple personality disorder: review of 100 recent cases. J. Clin. Psychiatry 47, 285–293.
Ross, C. A., Norton, G. R., and Wozney, K. (1989). Multiple personality disorder: an analysis of 236 cases. Can. J. Psychiatry 34, 413–418. doi: 10.1177/070674378903400509
Sar, V. (2011). Epidemiology of dissociative disorders: an overview. Epidemiol. Res. Int. 2011, 404538. doi: 10.1155/2011/404538
Simeon, D., and Abugel, J. (2006). Feeling Unreal. Depersonalization Disorder and the Loss of the Self. New York, NY: Oxford University Press.
Smith, J. A., and Osborn, M. (2008). “Interpretative phenomenological analysis,” in Qualitative Psychology: A Practical Guide to Research Methods , ed. J. Smith (London: Sage), 53–80.
Steele, K., Boon, S., and Van der Hart, O. (2016). Treating Trauma-Related Dissociation. A Practical, Integrative Approach. New York, NY: W. W. Norton & Company.
Steele, K., Van Der Hart, O., and Nijenhuis, E. R. (2005). Phase-oriented treatment of structural dissociation in complex traumatization: overcoming trauma-related phobias. J. Trauma Dissociation 6, 11–53.
Thomas, A. (2001). Factitious and malingered dissociative identity disorder: clinical features observed in 18 cases. J. Trauma Dissociation 2, 59–77. doi: 10.1300/J229v02n04_04
Van der Hart, O., Nijenhuis, E., and Steele, K. (2006). The Haunted Self: Structural Dissociation and the Treatment of Chronic Traumatization. London: W.W. Norton & Co.
Van der Hart, O., Nijenhuis, E. R., and Solomon, R. (2010). Dissociation of the personality in complex trauma-related disorders and EMDR: theoretical considerations. J. EMDR Pract. Res. 4, 76–92. doi: 10.1891/1933-3196.4.2.76
World Health Organization (1993). The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization.
Keywords : dissociative identity disorder (DID), false-positive cases, personality disorder, dissociation, differential diagnosis
Citation: Pietkiewicz IJ, Bańbura-Nowak A, Tomalski R and Boon S (2021) Revisiting False-Positive and Imitated Dissociative Identity Disorder. Front. Psychol. 12:637929. doi: 10.3389/fpsyg.2021.637929
Received: 04 December 2020; Accepted: 14 April 2021; Published: 06 May 2021.
Reviewed by:
Copyright © 2021 Pietkiewicz, Bańbura-Nowak, Tomalski and Boon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Igor Jacob Pietkiewicz, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Research article
- Open access
- Published: 07 September 2020
Living with personality disorder and seeking mental health treatment: patients and family members reflect on their experiences
- Karlen R. Barr 1 ,
- Mahlie Jewell 2 ,
- Michelle L. Townsend 1 &
- Brin F. S. Grenyer 1
Borderline Personality Disorder and Emotion Dysregulation volume 7 , Article number: 21 ( 2020 ) Cite this article
15k Accesses
13 Citations
37 Altmetric
Metrics details
Despite effective treatments for personality disorders being developed, consumers and carers often report negative experiences of mental health services, including challenges accessing these treatments.
This qualitative study used separate focus groups to compare the unique perspectives of consumer and carers, and to investigate how to improve services for individuals with personality disorders. Reflexive thematic analysis was used to analyze the data.
Both consumers and carers ( N = 15) discussed the value of providing appropriate information to consumers when they are diagnosed with personality disorder. Consumers and carers described the importance of creating a safe environment for consumers when they present to the emergency department. Both groups discussed experiencing positive and negative treatment from mental health professionals, and suggested that professionals should be trained to understand personality disorder. Limited accessibility and quality of services, and offering peer support to consumers were also described by consumers and carers. Consumers and carers also had perspectives which were unique to their group. Consumers identified the importance of psychological treatment, having a strong therapeutic relationship with a mental health professional, and the benefit of long term psychotherapy with the same professional. Broadening the scope of psychotherapies including creative, animal-assisted, and physical therapies was recommended by consumers. Carers described the importance of assessing for personality disorder and intervening early. Involvement in the assessment, diagnosis, and intervention process was important to carers. The desire to be recognized and supported by mental health professionals was discussed by carers.
Conclusions
This research contributes to the concern that consumers with personality disorder and their carers experience stigma and low quality care within mental health services. In line with these findings, we recommend guidelines for health professionals who work with consumers with personality disorder.
Personality disorders are severe mental disorders characterized by disturbances in affect, identity, and relationships [ 1 ]. Approximately 7.8% of the population has a personality disorder [ 2 ], and people with personality disorders represent about 20% of emergency department and 25% of inpatient mental health admissions [ 3 ]. In mental health and primary care settings, borderline personality disorder (BPD) is the most common personality disorder [ 4 ]. Effective treatments for personality disorder exist, including dialectical behavior therapy (DBT) and psychodynamic therapies [ 5 ]. However, consumers with personality disorder often are not offered or are unable to access evidence-based therapies and thus have negative experiences when receiving mental health services [ 6 ]. In addition, carers supporting consumers with personality disorder often experience high levels of stress, grief, and mental health problems [ 7 , 8 ], and they can experience difficulties accessing appropriate services for themselves and the consumers they support [ 9 ]. Considering the perspectives of consumers and carers is recommended to improve mental health services [ 10 ], and is supported by government [ 11 , 12 ] and mental health professionals [ 13 , 14 ].
Experiences of mental health services have been studied from the perspectives of consumers with various mental illnesses and their carers. Consumers describe the importance of mental health professionals discussing diagnoses with consumers and carers, and providing hope and information regarding diagnosis [ 15 ]. Regarding treatment planning, consumers want to be involved in their treatment decisions [ 16 ], although they are often excluded from participating in decision making [ 17 ]. Further, consumers describe not being prepared for hospital discharge, not being involved in the decision to discharge, and not receiving adequate support following discharge [ 18 ]. Carers supporting consumers with a range of mental health problems express that they have little involvement in mental health services and little access to information on mental health services [ 16 ]. Many carers believe they should have access to information about consumers, and report that confidentiality prevents them from receiving information about the consumer they support. Carers describe wanting respectful treatment for themselves and consumers, and better communication from mental health professionals, including education about specific disorders [ 19 ]. Other barriers described by carers include poor communication between services, limited service accessibility, and receiving little information about consumer treatment plans [ 20 ]. Carers also experience inconsistent assistance from mental health professionals in response to consumer mental health crises [ 21 , 22 ].
Multiple studies have investigated the experiences of consumers with personality disorder regarding mental health services. Consumers with personality disorder often do not receive an explanation of their diagnosis [ 23 ], or experience stigmatizing language and insufficient evidence-based information about their diagnosis [ 6 ]. Consumers have also described negative responses from health professionals in the emergency department [ 24 ]. Other negative experiences include poor communication from professionals, and inappropriate treatment, such as not having concerns taken seriously [ 6 ]. Increasing psychological and emotional support is recommended by consumers with personality disorder [ 6 ], including being supported by health professionals who help them understand their feelings [ 23 ].
Perspectives of mental health services from carers supporting consumers with personality disorder have also been investigated. Carers often experience relationship difficulties with the consumers they support, and do not know where to find help [ 9 ]. The majority of carers want support for themselves but find carer support services are unavailable or difficult to access [ 9 , 25 ]. Carers can also experience difficulty supporting consumers to find mental health professionals and consistent services to provide support to consumers with personality disorder [ 9 ]. In addition, many carers describe not receiving an explanation of the consumer’s diagnosis and not being appropriately involved in treatment decisions [ 25 ]. Carers identified wanting more information about personality disorder and how to respond to crises, and express that they are often expected to make treatment decisions without having sufficient knowledge [ 26 ].
A systematic review of 38 studies examined the perspectives of consumers and carers regarding mental health services for individuals with BPD [ 27 ]. Across the studies, consumers described receiving limited information about the assessment process and BPD diagnosis, negative responses from mental health professionals in the emergency department or inpatient setting, limited information options for therapeutic interventions, and poor communication regarding the availability of services. Studies exploring the carer perspective found that carers wanted their supporting role and their difficulties to be recognized by mental health professionals, be provided more information regarding BPD diagnosis and treatment options, and information about how to effectively respond to the consumer they support. While consumers and carers shared some consistent views, differences in opinion were observed, such as carers focusing on the lack of support they received from professionals. Comparing the consumer and carer experiences was limited because only five studies were found regarding the carer perspective, and only one study included the perspectives of consumers and carers. Therefore, more information is required regarding similarities and differences of consumer and carer views. In addition, few of the included research studies were co-produced with consumers or carers, even though this is known to lead to questions and findings closer to what people with lived experience require [ 28 ].
Problems continue to be present in personality disorder services and programs and require input from consumers and carers regarding possible improvements. It is important to increase knowledge regarding the views of consumers and carers who support someone with personality disorder, to compare views of consumers and carers regarding services for individuals with personality disorder, and to co-produce research on consumer and carer perspectives. The purpose of this study was to bring together all these needs and gaps in the literature: to explore and compare the perspectives of consumers and carers regarding personality disorder services using a co-design approach aimed to inform the development of better services.
Participants
Participants were recruited using a flyer advertisement that was sent to consumer and carer support and advocacy groups, and services which support individuals with personality disorder. Participants were invited to participate if they were either a consumer with a lived experience of personality disorder or a carer or family member supporting someone with a personality disorder. The views of 15 individuals were obtained, a sample large enough for data saturation within a qualitative approach. Table 1 outlines the demographic characteristics of the participants.
Participants provided informed written consent prior to study participation, following study approval from the Institutional Review Board. Two focus group discussions occurred simultaneously; one with consumers and one with carers, as requested by the participants. Both focus groups were co-facilitated by 2 researchers with experience in personality disorders and group facilitation. The consumer focus group was co-facilitated by the consumer researcher. In addition, 1 mental health professional was present in each group to provide assistance to participants if they became distressed. Focus group questions were based on a guide that was co-designed by the authors. Some questions required participants to provide written answers or creative responses. Questions differed slightly for consumer and carer participants. Open-ended questions were followed with relevant follow-up questions as required. Questions explored the quality of care experienced at different services, including mental health services and emergency services, and how the practice of health professionals could improve. Questions included, “What have you found most helpful about the services you have been involved in?”, “Is there anything you wish clinicians and service leaders better understood about individuals living with personality disorder?” and “How can health professionals best support families and carers of individuals who have been recently diagnosed with personality disorder?” The discussions were audio recorded and transcribed. Focus group discussions occurred over a 90-min period. A $50 voucher was provided to participants as compensation for their time.
Data analysis
The data were analyzed using reflexive thematic analysis, which conceptualizes themes as patterns based in meaning [ 29 ]. First, the transcripts were read and re-read and brief notes were made to obtain familiarization with the data. Next, participant statements were coded into nodes through the software NVivo 11. Nodes were created using an inductive orientation to gather statements with similar meanings. Themes were constructed based on the nodes, and were revised as needed to reflect the lived experience of participants. One researcher independently coded the data, which was informed by regular discussions with the research team. The consumer researcher was part of the research team throughout all phases and provided active input into the themes developed. Inter-rater reliability was obtained by all team members arriving at a consensus for the coding. In addition, an independent researcher coded a portion of data to allow us another view on agreement - with Cohen’s kappa coefficient for inter-rater reliability being κ = 0.75, which indicates a relatively high level of agreement [ 30 ].
Consumer perspectives
In this section, the views that were gathered from the consumer focus group are presented.
Theme 1: challenges and successes finding a mental health professional who understands personality disorder
Consumers described how medical and psychiatric registrars often do not have the experience and knowledge base to provide treatment or information to people with personality disorders. Difficulties in finding a mental health professional who has training in and understands personality disorders were described by several participants. “In my long hard, long lived history as a consumer, with an illness, I have been referred and searched high and low for private psychologists who would have knowledge of this particular ill – normality, this illness, and you know, there’s very few out there who are familiar enough with it.” Consumers described various instances when mental health professionals used stigmatizing language, which had a major negative influence on their well-being. “[After multiple stigmatizing comments] I felt so completely let down and failed by the public system. Like my life didn’t matter, like I didn’t matter.”
Several consumers described positive experiences with mental health professionals who specialize in treating personality disorders. Consumers explained the importance of finding a mental health professional that they can connect with, who complements their specific needs. A trial and error process of finding a suitable mental health professional was described , “They’re not always going to be – the right one is not always going to be the first one you get. There’s a lot of trial and error.” Participants valued mental health professionals who were clear about how long they could work with them, admitted to making mistakes, kept them accountable to their goals, and persevered in contacting consumers. “I didn’t turn up three times and she kept calling me. And she kept saying to me, ‘If you won’t come see me, let me send you to someone else.’”
The importance of mental health professionals being specifically trained to work with people with personality disorders was discussed. “They (mental health professionals) should all be, you know, trained to work with people who have BPD. They should understand it.” Communicating with consumer advocates was recommended for mental health professionals to improve their understanding of personality disorders. Consumers discussed how they wanted mental health professionals to understand that people with personality disorders can recover.
Theme 2: the need to improve the assessment and diagnosis process
While some participants reported that they did not respond well to the diagnosis initially, others readily embraced the diagnosis. “I liked my diagnosis. I was, like, yes. I know what it is.” Consumers frequently described being given a diagnosis of personality disorder without any explanation or further information about symptoms, or how being provided with this information would help. One participant described receiving a diagnosis following a quick assessment, without receiving an explanation. “I spoke to her (the psychologist) for, maybe, 60 to 90 minutes, and then she diagnosed me with borderline personality disorder… no one gave me any, sort of, information or anything. I was just stuck with this diagnosis and I knew nothing about it.” Consumers described the potential helpfulness of receiving appropriate treatment options when a diagnosis is given, including referral to specialist clinicians. Factsheets that provide information about personality disorders, including symptoms and treatment options, were suggested to be given to consumers at diagnosis. “I’d like a fact sheet that you could – you know. An actual, just, you – you know, this is your diagnosis, these are the symptoms you have with it, here is the available treatment options, here is what happens through with these treatment options.” Consumers described the importance of health professionals assessing for co-occurring mental health or physical health issues.
Theme 3: the need to improve communication between mental health professionals to ensure continuity of care
Consumers described how improved communication between mental health professionals regarding diagnosis, treatment, and hospital discharge is needed . “Then they referred me to the dietician who never came, and that was it, and then they just discharged me.” Participants described disappointment when mental health professionals did not respond to recommendations made by a consumer’s private psychologist, particularly when consumers are experiencing a crisis. “In spite of my psychologist writing a detailed letter with all of my symptoms, the fact that she’s known me for so long, and that she’s sufficiently worried about my safety at this point in time, they were still willing to try and send me back home.” Professionals listening to the advice of a consumer’s psychologist can help consumers feel cared for and help them trust professionals and the mental health system. “She (my psychologist) tried to visit me a couple of times in locked wards and was not allowed in, um, and – and, um, would have been really helpful if she could have just spoken to them and said, ‘Hey, here’s what works for [the person I support],’ but they wouldn’t listen to her.” In addition, it was recommended that professionals share their resources with one another, such as fact sheets, so that consumers can receive the information they require.
The importance of continuity of care was discussed by many participants. “He (psychiatry registrar) says to me, ‘What are you here for?’ And I say, ‘Well, did you read the notes from my last appointment here?’ He said, ‘No. Tell me all about yourself.’” The capacity of a mental health professional to see a consumer for more than a few months may relieve a consumer from the difficulty of repeatedly sharing their past experiences. When a referral to another mental health professional occurs, it may be helpful to provide information on the consumer to assist continuity of care, if consent from consumers is provided. “There hadn’t been any change over from the previous therapist, so we had to start all over again and tell the story for the umpteenth time.” When referring a consumer to another service, professionals could provide some crisis skills training to help consumers while they are in between services. Following up with information that is communicated to consumers was also described as important. “I had a lot of problems with their continuity of service, in, ‘We’ll call you tomorrow,’ and then three days later you get a call back.”
Theme 4: increasing feelings of safety when consumers are experiencing a crisis
Consumers described how first responders often communicated effectively with them and helped them to feel safe and comfortable. “I feel more safe having police and ambos come to my house than I would have an acute care worker come to my house.” However, inappropriate verbal and physical interactions from first responders were also discussed. Consumers described how identifying with the LGBTIQA+ community can result in negative or poor treatment from some first responders.
Some consumers described how acute care units and emergency departments did not provide a safe environment. Consumers described receiving negative judgments from mental health professionals during crises, including being ignored, shamed, denied services or being told that they are “not trying hard enough.” Simple changes to service environments such as allowing curtains to be drawn or receiving positive communication from mental health professionals were described to increase comfort. “They allow you to have the curtains on, so you can calm yourself down.”
Limitations of inpatient wards and emergency departments were described, such as being locked up and alone. Therefore, alternative safe places were suggested for consumers to go to when experiencing distress, such as cafes, respite homes, or rehabilitation centres. “I can’t be alone because I’m not safe enough to be alone, but I don’t need the acute care centres. I just don’t even need to be talking to someone, but I just need to not be alone.”
Theme 5: providing expanded treatment options and increasing service accessibility
Consumers described various ways that treatments and services could be improved. Some consumers discussed the power of art therapy and creative therapies, animal-assisted therapy, nature therapy, and physical therapy. “I found a sexual assault nurse who actually got balloons and filled them with, um, like, paint, and just gave me, like, darts, basketball shooters, the room was just splattered everywhere. It was so colourful that it was a distraction… I find sometimes just having a psychologist isn’t good enough, you need that art therapy; you need the physical therapy.” Several consumers described how peer support could aid them, including providing support groups and safe places where people with lived experience can connect. Consumers also described the helpfulness of 24-h phone lines. One consumer described the usefulness of e-therapy. “He (my psychologist) was prepared to do some sessions remotely by video-conference. You know, so, we were just about to go into the UK at the time, and then it – I didn’t have to break my therapy.” One consumer discussed the benefit of support being provided to carers. “The support group that my mum has been going to… before she’d often just get upset or angry or - whereas now she just seems to be a lot better at knowing what to do without making it worse, kind of thing. So, it’s good.”
Consumers discussed the limited availability of mental health services for personality disorders. Some barriers to accessing mental health services included homelessness, location, and finances . “I wish clinicians understood how cost-prohibitive consistent treatment is for low-income patients.” Non-government organizations were acknowledged by some participants as providing better care compared to government organizations.
Carer perspectives
In this section, five themes from discussions in the carer focus group are presented.
Theme 1: the importance of carer involvement in early assessment and intervention
Carers described how they wanted to be involved during assessment, diagnosis and intervention. Receiving a diagnosis for the person they support was described as taking a lengthy amount of time. “ My biggest issue was getting the diagnosis. Yeah. That took 10 years. Yeah. And the hardest part was that how quick they seem to have – have wanted to keep sending her home.” Frustration was expressed by carers about how mental health professionals often mislabelled a consumer’s difficulties as anxiety, depression, or ‘normal’ behaviours, before later giving a diagnosis of personality disorder. Carers described working hard to find a mental health professional who would provide an assessment or diagnosis for the person they support, particularly during adolescence. “It took yeah, begging and pleading and we are not taking her home until we spoke to a psychiatrist, to tell them our side, and then we got a diagnosis.” After diagnosis, carers emphasized the importance of mental health professionals explaining a personality disorder diagnosis to consumers and carers. The importance of early diagnosis and assessment was highlighted by many carers, such as when a person first experiences a crisis. “ They hit their absolute lowest before there’s a click or a diagnosis into what’s going on, in comparison to trying to seek help for many years, when you can already see many traits .”
Carers discussed the importance of communicating their perspective of the person they support to inform decisions made by mental health professionals, such as diagnosis. Involving carers as soon as possible was recommended, such as during the consumer’s first crisis. Several participants suggested involving carers in treatment helps them to understand what the person they support is learning and experiencing. Confidentiality was described as a barrier to carers being involved in assessment and treatment. “There is no communication, because of this confidentiality. And I think that could be the worst enemy, basically, standing in the way of the family therapy.”
Theme 2: improving responses and follow-up when consumers present in crisis
Mixed feedback was received from carers in relation to the responses from police and ambulance responders. Some negative interactions were described, including physical force by police rather than a dialogue approach. “In one case, the police came and basically… he was thrown on to the floor, you know, with policemen with the guns. It was so traumatic, instead of first having a dialogue approach.” However, many carers described compassionate treatment from police and ambulance responders towards consumers and carers, which was sometimes experienced as comparably better than treatment provided by other mental health professionals during crises. “The first responders are much more caring for carers, family members and explaining what they’re doing, and in their compassionate treatment.”
Carers discussed how consumers can experience difficulties at the emergency department when there are physical health assessments and long wait times for mental health problems. Several carers discussed how separating mental health problems and physical health problems in the emergency department may result in better care. Providing a safe place within the emergency department “that people can go to in a crisis to calm down and self-soothe” was also recommended.
Carers described how consumers were often sent home from the emergency department without appropriate support. “We went to emergency and were sent home with nothing in our first instant… [the person I support] was just sent home to me, with no explanation of anything .” Following discharge from emergency departments or inpatient services, carers recommended that mental health professionals inform consumers and carers about the treatment that was provided and treatment options for the future. Carers proposed that communication between mental health professionals and carers about a consumer’s hospital discharge can help protect the safety of consumers and others. Several carers described not receiving information from mental health professionals unless it was requested by the carer. “Even when [the person I support] was sent home from hospital two times, she was never sent home with anything… Not unless you ask for it.”
Theme 3: increasing mental health professionals’ understanding of personality disorders and improving communication
Carers described the harms of mental health professionals using inappropriate and stigmatizing language when communicating with consumers and carers. The use of recovery-oriented, strengths-based language was desired by carers, such as expressing an understanding of the difficult experiences faced by carers and consumers. Mental health professionals who provided explanations about mental health problems which can be understood by consumers and carers were valued. “I think if they actually remember that this is the first time someone’s hearing it, they actually may be forthcoming with more information.”
Many carers discussed improving training and awareness of personality disorders for health professionals. “If the training is proper – with the GPs, with the doctors, psychiatrists, psychologists, nurses, we have the system right. It’s a matter of just the right education.” Carers described how mental health professionals need to be aware of support that is available and to explain treatment options. Carers also wanted guidance from mental health professionals on how they can best support consumers. “We (carers) need to know what we can do to help them. We want to understand how they feel and why they act/behave the way they do. Please help us to ensure they get the best care and the treatment they need to recover.”
Carers discussed the value of mental health professionals communicating with one another, including providing referral information. When mental health professionals liaise, it can provide a more holistic picture of a person’s difficulties, including physical and psychological symptoms. “[The person I support] has a lot of physical symptoms that I think are a result of her mental state. But I’m not sure. So, they sent her off for all these tests… but there’s no – no one’s like, pulling it all together. The GPs should be, but they don’t.”
Theme 4: improving accessibility and quality of services for consumers
Several carers described limited availability and quality of services within the mental health system, including the public and private healthcare system. “She’s had stays in private hospitals as well. And to be honest, not a lot better. I mean, it’s much nicer place. But I don’t know that the level of care is much better, really, considering how much you pay for it.” The small amount of psychological sessions provided by the public healthcare system was described by carers as insufficient. The proximity of services was also described negatively, including consumers having long commutes to receive treatment. Long wait times to receive treatment were also discussed. “She was on four waitlists in the city at private clinics. One down here in this region. Couldn’t get her in. Christmas Eve, they rang and said, ‘Oh, we’ve got a bed in the city.’ So October, November, December, she was on 24-hour watch. Because I couldn’t get her in anywhere.”
Carers also recommended personalizing therapy for specific consumers, including offering support in nature. Several carers described the helpfulness of DBT. “She (the person I support) ended up being put through a DBT group… that has by far been one of the best things for our entire family.” Carers described how offering employment assistance and peer support groups for consumers may be beneficial.
Theme 5: improving support for carers
Carers described feeling overwhelmed and stressed by caring for a person with personality disorder and suggested carer respite as a valuable form of support. One carer described feeling hopeless after multiple attempts to find a treatment that would work for the person they support. Financial and work difficulties due to time commitments supporting someone with personality disorder were also described. “The Government needs to know is the financial strain on families… with needing weekly psychologist, regular psychiatrist, not being able to get to work, because you get called home all the time.”
Carers discussed the importance of mental health professionals understanding the difficulties experienced by carers. Carers described receiving little support for themselves from mental health professionals. Mental health professionals asking a carer ‘how are you?’ was described as a positive first step. “I had one registered nurse, who was special… who actually asked me how I was. And that was probably year six of the journey. And until then, not a soul had ever asked me how I was.” Other options for providing support to carers were discussed, including a 24-h phone line, peer support groups, counselling for carers, and promoting self-care. Providing educational resources to carers was recommended, such as having brochures in hospital waiting rooms, offering educational groups, and providing links to online information. Several carers recommended increasing public awareness and understanding of personality disorders through education, which may help others in the general community understand the experiences of consumers and carers.
A comparison of the consumer and carer themes can be found in Table 2 . Both consumers and carers described disturbing stigma and prejudice, but also receiving some exemplar care from some professionals. Broadening support options for both consumers and carers was a priority.
This study explored and compared experiences of personality disorder services from the perspectives of consumers and carers. Consumers and carers described a number of negative and positive experiences with mental health services and provided recommendations on how services could improve.
Both consumers and carers discussed the importance of receiving appropriate information when a person is diagnosed with personality disorder, which is consistent with previous research [ 6 , 23 , 31 , 32 ]. Taking a collaborative stance in working with consumers during the assessment and diagnosis process was identified as a way to reduce stigmatization and empower consumers to engage in treatment [ 33 ]. Safety when in crisis was a major concern, both interpersonally (e.g. through promoting compassionate communication) and physically (e.g. avoiding rough handling by authorities, having safe rooms within emergency settings). Consumers also described creating safe places separate from the emergency department, such as voluntary residential or drop-in programs. Previous research indicates that residential programs may be a beneficial alternative to the emergency department for consumers with BPD [ 34 ]. Investigating the carer perspective of alternative safe places and respite options could also be important.
Both positive and negative experiences with mental health professionals and first responders were described by consumers and carers. The literature suggests that stigmatization and discrimination of personality disorder in mental health services continues to be prominent [ 35 ], although professional attitudes toward personality disorder have improved over time [ 36 ]. During crises, consumers and carers expressed receiving better treatment from first responders, compared to mental health professionals, which may mean that mental health professionals have more stigma of personality disorder compared to first responders [ 37 ]. Both groups suggested improving mental health professionals’ knowledge and understanding regarding personality disorders. Research has shown that training can improve mental health professionals’ understanding and attitudes [ 38 , 39 ]. Increasing the accessibility and awareness of training may be required. Providing training to first responders and increasing public awareness of personality disorder may also help reduce stigma and discrimination [ 35 ].
Consumers and carers described the potential benefit of offering peer support to consumers. Peer support can help consumers with various mental health problems by providing shared experiences which offer validation and hope [ 40 , 41 ]. Increasing the number of peer workers and peer support groups for consumers with personality disorder may be valuable. In addition, both carers and consumers described difficulty accessing personality disorder services. Increasing availability of services and making services more affordable may benefit consumers and carers.
From the consumer perspective, importance was given to the therapeutic relationship with mental health professionals, including finding a clinician they can connect with who specializes in personality disorder. This finding is unsurprising given that a strong therapeutic alliance can facilitate recovery [ 42 ]. Consumers described how mental health professionals, such as medical registrars, often did not have sufficient knowledge and experience to support them, and they requested people with experience who had specialized knowledge of personality disorders. Ensuring registrars who work with consumers with personality disorder have appropriate knowledge prior to in-person interactions and are supported by a specialist mental health professional may be helpful. Regarding referrals, health professionals should increase their awareness of personality disorder treatments available in their area, and offer consumers a range of possible mental health professionals that can support them.
Consumers also discussed the importance of continuity of care, including being able to work long term with a mental health professional. Therefore, it is important for mental health professionals to clarify how long they can work with consumers and to provide appropriate support when a consumer is transitioning from one professional to another. In addition, mental health professionals should communicate with one another to ensure they have all necessary information to support a consumer with personality disorder. Collaboration amongst mental health professionals involved in a consumer’s treatment is associated with improved consumer outcomes [ 43 ]. Further, consumers described the importance of private psychologists being able to communicate with other professionals involved in their care during a crisis. With a consumer’s consent, emergency department and inpatient services should collaborate with a consumer’s primary mental health professional, such as a private psychologist.
Expanded therapy options, such as art and animal-assisted therapy, were also recommended by consumers. Previous research has shown that art therapy can help increase well-being and decrease symptoms in consumers with a personality disorder [ 44 ]. Increasing accessibility and affordability of creative therapies and other approaches is recommended to improve referrals and options for consumers.
For carers, importance was placed on early assessment and intervention, which is supported by evidence and treatment guidelines [ 10 , 45 ]. However, consumers did not discuss early intervention, although they have previously described delays in receiving a diagnosis [ 42 ]. Carers also focussed on being involved in the assessment and treatment of the consumers they support, although consumers did not mention this. While carer involvement in assessment and intervention is important to carers and may help them support consumers [ 46 ], the perspective of consumers should be considered because not all consumers endorse family or friend involvement in their care [ 47 , 48 ]. In addition, carers focussed on improving support for carers, including having mental health professionals checking in on carers. However, consumers can have negative experiences of mental health professionals providing support to their carers [ 47 ]. Therefore, professionals may need to find a balance when providing support to consumers and carers. For example, a professional might provide carers with referral information to a psychological education or carer peer support group after consulting with the consumer and clearly explaining the reason for providing support to carers. Alternatively, carers may seek their own supports through mental health professionals and support groups. Table 3 provides a summary guideline of recommendations for health professionals arising from this research.
Limitations and future research
Although data saturation occurred in the analysis of qualitative interviews, the small sample size used in the study may be a limitation as other views may not have been represented [ 49 ]. We did not investigate further the treatment history, specific diagnoses of the consumers, amount of carer engagement with services, or cultural background of participants, meaning it was difficult to estimate to what extent our sample were representative of the broader consumer and carer population. Statements spontaneously reported by consumers and carers did reflect in detail findings from previous studies supporting that our sample was comparative to others in the literature. Further, the sample was predominately female, and the perspectives of male consumers and carers were limited, and it would be important to increase their participation in future research. Consumers and carers were not always asked the same questions, making it difficult to compare their experiences in some topic areas. The groups were ran as semi-structured focus groups and the facilitators followed a guide, but were all responsive to the participants in the focus group and what they wanted to focus on. For example, consumers were not asked about carer involvement in assessment and treatment. Despite the limitations, the findings provide important information to improve services for individuals living with personality disorder and their carers. Future research could explore safe environments for consumers experiencing crisis, and expanded treatment options for personality disorders, including art therapy and peer support. In addition, there is a need to broaden our understanding of the variety and nature of consumer views of having carers involved in their assessment and treatment.
The current study explored and compared mental health service experiences from the perspectives of consumers with personality disorder and carers. The findings add to the ongoing concern about the stigma, prejudice and poor provision of services for people with personality disorder, despite some examples of high quality work being delivered. In addition, the findings highlight similarities and differences in consumer and carer perspectives. Based on the findings, a number of guidelines are provided to inform the practice of health professionals who support consumers with personality disorder.
Availability of data and materials
Data from the current study will not be made available, as participants did not consent for their transcripts to be publicly released. Extracts of participant responses have been made available within the manuscript.
Abbreviations
Borderline personality disorder
Dialectical behavior therapy
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Washington, D.C: American Psychiatric Association; 2013.
Google Scholar
Winsper C, Bilgin A, Thompson A, Marwaha S, Chanen AM, Singh SP, et al. The prevalence of personality disorders in the community: a global systematic review and meta-analysis. Br J Psychiatry. 2019;216:1–10.
Lewis KL, Fanaian M, Kotze B, Grenyer BFS. Mental health presentations to acute psychiatric services: 3-year study of prevalence and readmission risk for personality disorders compared with psychotic, affective, substance or other disorders. BJPsych Open. 2019;5:1–7.
Korzekwa MI, Dell PF, Links PS, Thabane L, Webb SP. Estimating the prevalence of borderline personality disorder in psychiatric outpatients using a two-phase procedure. Compr Psychiatry. 2008;49(4):380–6.
PubMed Google Scholar
Cristea IA, Gentili C, Cotet CD, Palomba D, Barbui C, Cuijpers P. Efficacy of psychotherapies for borderline personality disorder: a systematic review and meta-analysis. JAMA Psychiatry. 2017;74:319–28.
Morris C, Smith I, Alwin N. Is contact with adult mental health services helpful for individuals with a diagnosable BPD? A study of service users views in the UK. J Ment Health. 2014;23(5):251–5.
Bailey RC, Grenyer BFS. Supporting a person with personality disorder: a study of carer burden and well-being. J Personal Disord. 2014;28(6):796–809.
Bailey RC, Grenyer BFS. The relationship between expressed emotion and wellbeing for families and carers of a relative with borderline personality disorder. Personal Ment Health. 2015;9(1):21–32.
Dunne E, Rogers B. “It’s us that have to deal with it seven days a week”: Carers and borderline personality disorder. Community Ment Health J. 2013;49(6):643–8.
Grenyer BFS, Ng FY, Townsend ML, Rao S. Personality disorder: a mental health priority area. Aust N Z J Psychiatry. 2017;51(9):872–5.
Commonwealth of Australia. National standards for mental health services. 2010.
Mental Health Commission of Canada. Changing directions changing lives: The mental health strategy for Canada. 2012.
Jørgensen K, Rendtorff JD. Patient participation in mental health care - perspectives of healthcare professionals: an integrative review. Scand J Caring Sci. 2018;32(2):490–501.
Bee P, Brooks H, Fraser C, Lovell K. Professional perspectives on service user and carer involvement in mental health care planning: a qualitative study. Int J Nurs Stud. 2015;52(12):1834–45.
PubMed PubMed Central Google Scholar
Milton AC, Mullan BA. A qualitative exploration of service users’ information needs and preferences when receiving a serious mental health diagnosis. Community Ment Health J. 2015;51(4):459–66.
Lammers J, Happell B. Mental health reforms and their impact on consumer and carer participation: a perspective from Victoria. Australia Issues Ment Health Nurs. 2004;25(3):261–76.
Stomski NJ, Morrison P. Participation in mental healthcare: a qualitative meta-synthesis. Int J Ment Heal Syst. 2017;11(1):67.
Redding A, Maguire N, Johnson G, Maguire T. What is the lived experience of being discharged from a psychiatric inpatient stay? Community Ment Health J. 2017;53(5):568–77.
Goodwin V, Happell B. Consumer and carer participation in mental health care: the carer’s perspective: part 1 - the importance of respect and collaboration. Issues Ment Health Nurs. 2007;28(6):607–23.
Goodwin V, Happell B. Consumer and carer participation in mental health care: the carer’s perspective: part 2—barriers to effective and genuine participation. Issues Ment Health Nurs. 2007;28(6):625–38.
Brennan A, Warren N, Peterson V, Hollander Y, Boscarato K, Lee S. Collaboration in crisis: Carer perspectives on police and mental health professional’s responses to mental health crises. Int J Ment Health Nurs. 2016;25(5):452–61.
Olasoji M, Maude P, McCauley K. Not sick enough: experiences of carers of people with mental illness negotiating care for their relatives with mental health services. J Psychiatr Ment Health Nurs. 2017;24(6):403–11.
CAS PubMed Google Scholar
Lawn S, McMahon J. Experiences of care by Australians with a diagnosis of borderline personality disorder. J Psychiatr Ment Health Nurs. 2015;22(7):510–21.
CAS PubMed PubMed Central Google Scholar
Vandyk A, Bentz A, Bissonette S, Cater C. Why go to the emergency department? Perspectives from persons with borderline personality disorder. Int J Ment Health Nurs. 2019;28(3):757–65.
Lawn S, McMahon J. Experiences of family carers of people diagnosed with borderline personality disorder. J Psychiatr Ment Health Nurs. 2015;22(4):234–43.
Acres K, Loughhead M, Procter N. Carer perspectives of people diagnosed with borderline personality disorder: a scoping review of emergency care responses. Australas Emerg Care. 2019;22(1):34–41.
Lamont E, Dickens GL. Mental health services, care provision, and professional support for people diagnosed with borderline personality disorder: systematic review of service-user, family, and carer perspectives. J Ment Health. 2019:1–15.
Gillard S, Turner K, Neffgen M, Griggs I, Demetriou A. Doing research together: bringing down barriers through the ‘coproduction’ of personality disorder research. Ment Health Rev J. 2010;15(4):29–35.
Braun V, Clarke V, Hayfield N, Terry G. Thematic analysis. In: Liamputtong P, editor. Handbook of research methods in health social sciences. Singapore: Springer Singapore; 2019. p. 843–60.
Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37:360–3.
Buteau E, Dawkins K, Hoffman P. In their own words: improving services and hopefulness for families dealing with BPD. Soc Work Ment Health. 2008;6(1–2):203–14.
Horn N, Johnstone L, Brooke S. Some service user perspectives on the diagnosis of borderline personality disorder. J Ment Health. 2007;16(2):255–69.
Hackmann C, Wilson J, Perkins A, Zeilig H. Collaborative diagnosis between clinician and patient: why to do it and what to consider. BJPsych Adv. 2019;25(4):214–22.
Mortimer-Jones S, Morrison P, Munib A, Paolucci F, Neale S, Hellewell A, et al. Staff and client perspectives of the open Borders programme for people with borderline personality disorder. Int J Ment Health Nurs. 2019;28(4):971–9.
Sheehan L, Nieweglowski K, Corrigan P. The stigma of personality disorders. Curr Psychiatry Rep. 2016;18(1):1–7.
Day NJS, Hunt A, Cortis-Jones L, Grenyer BFS. Clinician attitudes towards borderline personality disorder: a 15-year comparison: attitudes toward borderline personality disorder. Personal Ment Health. 2018;12(4):309–20.
Bonnington O, Rose D. Exploring stigmatisation among people diagnosed with either bipolar disorder or borderline personality disorder: a critical realist analysis. Soc Sci Med. 2014;123:7–17.
Lamph G, Sampson M, Smith D, Williamson G, Guyers M. Can an interactive e-learning training package improve the understanding of personality disorder within mental health professionals? J Ment Health Train Educ Pract. 2018;13(2):124–34.
Welstead HJ, Patrick J, Russ TC, Cooney G, Mulvenna CM, Maclean C, et al. Mentalising skills in generic mental healthcare settings: can we make our day-to-day interactions more therapeutic? BJPsych Bull. 2018;42(3):102–8.
Gillard S, Gibson SL, Holley J, Lucock M. Developing a change model for peer worker interventions in mental health services: a qualitative research study. Epidemiol Psychiatr Sci. 2015;24(05):435–45.
Pallaveshi L, Balachandra K, Subramanian P, Rudnick A. Peer-led and professional-led group interventions for people with co-occurring disorders: a qualitative study. Community Ment Health J. 2014;50(4):388–94.
Ng FYY, Townsend ML, Miller CE, Jewell M, Grenyer BFS. The lived experience of recovery in borderline personality disorder: a qualitative study. Borderline Personal Disord Emot Dysregulation. 2019;6(1):1–9.
Tippin GK, Maranzan KA, Mountain MA. Client outcomes associated with interprofessional care in a community mental health outpatient program. Can J Commun Ment Health. 2016;35(3):83–96.
Haeyen S, van Hooren S, van der Veld WM, Hutschemaekers G. Promoting mental health versus reducing mental illness in art therapy with patients with personality disorders: a quantitative study. Arts Psychother. 2018;58:11–6.
Chanen AM, Thompson KN. Early intervention for personality disorder. Curr Opin Psychol. 2018;21:132–5.
Fitzpatrick S, Wagner AC, Monson CM. Optimizing borderline personality disorder treatment by incorporating significant others: a review and synthesis. Personal Disord Theory Res Treat. 2019;10(4):1–12.
CAS Google Scholar
Wonders L, Honey A, Hancock N. Family inclusion in mental health service planning and delivery: consumers’ perspectives. Community Ment Health J. 2019;55(2):318–30.
Landeweer E, Molewijk B, Hem MH, Pedersen R. Worlds apart? A scoping review addressing different stakeholder perspectives on barriers to family involvement in the care for persons with severe mental illness. BMC Health Serv Res. 2017;17(1):1–10.
Guest G, Bunce A, Johnson L. How many interviews are enough?: an experiment with data saturation and variability. Field Methods. 2006;18(1):59–82.
Download references
Acknowledgements
Charlotte van Schie for inter-rater reliability, and consumers and carers who participated in this study.
NSW Mental Health Commission Lived Experience Framework Implementation Grant, and NSW Ministry of Health support to the Project Air Strategy for Personality Disorders. The funders had no role in the design, recruitment, collection, interpretation, or writing of the study.
Author information
Authors and affiliations.
School of Psychology and Illawarra Health and Medical Research Institute, University of Wollongong, Wollongong, NSW, 2522, Australia
Karlen R. Barr, Michelle L. Townsend & Brin F. S. Grenyer
Project Air Strategy Consumer and Carer Advisory Committee, Wollongong, NSW, Australia
Mahlie Jewell
You can also search for this author in PubMed Google Scholar
Contributions
KRB - study design, participant recruitment, data collection, data analysis, and writing- original draft. MJ and MLT- study design, participant recruitment, data collection, data analysis, and writing- review and editing. BFSG - study design, data collection, and writing- review and editing. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Brin F. S. Grenyer .
Ethics declarations
Ethics approval and consent to participate.
Prior to the start of the study, this study received ethics approval from the University of Wollongong Social Sciences Human Research Ethics Committee (2015/430). All participants were informed of the aims and risks of the study and provided informed consent.

Consent for publication
Not applicable.
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Barr, K.R., Jewell, M., Townsend, M.L. et al. Living with personality disorder and seeking mental health treatment: patients and family members reflect on their experiences. bord personal disord emot dysregul 7 , 21 (2020). https://doi.org/10.1186/s40479-020-00136-4
Download citation
Received : 31 May 2020
Accepted : 11 August 2020
Published : 07 September 2020
DOI : https://doi.org/10.1186/s40479-020-00136-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Personality disorder
- Lived experience
- Qualitative
- Mental health services
Borderline Personality Disorder and Emotion Dysregulation
ISSN: 2051-6673
- General enquiries: [email protected]
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
Personality disorder
- Related content
- Peer review
- Orestis Kanter Bax , consultant psychiatrist in medical psychotherapy 1 2 ,
- Dimitrios Chartonas , consultant psychiatrist 2 3 ,
- Jennie Parker , independent lived experience researcher , KUF development lead 2 5 ,
- Spyridon Symniakou , GP partner 6 ,
- Tennyson Lee , consultant psychiatrist in medical psychotherapy , psychoanalyst , honorary senior lecturer 2 4 7 6 8
- 1 Basildon Complex Needs Psychotherapy and Personality Disorder Service, Essex Partnership University NHS Foundation Trust, UK
- 2 Centre for Understanding Personality (CUSP), London
- 3 Camden and Islington Personality Disorder Service, Camden and Islington NHS Foundation Trust
- 4 Deancross Personality Disorder Service, East London NHS Foundation Trust
- 5 Berkshire Healthcare NHS Foundation Trust
- 6 Blithdale Health Centre, Clinical Director East End Health Network
- 7 Institute of Psychoanalysis, British Psychoanalytical Society
- 8 Wolfson Institute, Queen Mary University of London
- Correspondence to O Kanter Bax orestis.kanter-bax{at}nhs.net
What you need to know
Personality disorders are a set of complex emotional difficulties. They are common, often unrecognised, and are associated with mental and physical health comorbidities and reduced life expectancy
Personality disorders are perceived as stigmatising diagnoses. Alternative terms have been proposed. New classification systems help in moving away from rigid use of categorical diagnoses
Assessment and management in primary care require a non-judgmental approach that builds trust through attentiveness, validation, openness, and consistency
Holistic care for people with personality disorders can be improved with reflective practice structures, staff training, collaboration, and team working
Sources and selection criteria
We searched Pubmed, Medline, Embase, the Cochrane Library, CINAHL, PsycINFO, AMED, British Nursing Index, HMIC, and Health Business Elite using the term “personality disorder”. Findings from randomised controlled trials (RCTs), systematic reviews, and meta-analyses were ranked as high in quality (see table 1 ) and we also used our own reference archives, books, and expert contacts to supplement the structured search.
Personality disorders describe a set of long standing complex emotional difficulties, which are common, highly stigmatised, and potentially disabling. They are frequently under-recognised and may run a long course when people lack access to appropriate treatment. Recent developments in evidence, guidelines, and policy have placed an emphasis on public awareness, de-stigmatisation, training professionals in generalist settings, improving access to specialist care, and improving physical health outcomes. 1 2 This article provides an overview of the latest information on the assessment and management of personality disorders in primary care, with an emphasis on borderline personality disorder (also referred to as emotionally unstable personality disorder).
What are personality disorders?
Personality disorders are pervasive and enduring, affecting the emotional, cognitive, and behavioural functioning of a person, expressed in relation to their self (eg, identity, self-evaluation, affect regulation, direction) and others (eg, intimacy, boundaries, sense of security in relationships). People with personality disorders may face difficulties with social functioning at work, with family, and with social life and leisure, and such difficulties may represent a significant deviation from what is expected for the individual’s developmental stage and culture. 3 No consensus exists on a single definition, research in the field is growing rapidly, and controversy surrounds the validity of existing conceptual frameworks. 4 Some people with lived experience and some clinicians question use of the term “personality disorder” altogether, and advocate for its replacement (for example, the term “complex emotional needs” has been proposed). 5
Negative attitudes and biases are still held about people who receive a diagnosis of personality disorder both in the general public 6 7 and among clinicians. 8 Longstanding misconceptions exist about the nature and “untreatability” of personality disorders, but evidence is growing for the efficacy of treatments for borderline personality disorder ( table 1 ) and emerging treatments for antisocial and narcissistic personality difficulties. 12 16
Evidence based treatment for borderline personality disorder 9 10 11
- View inline
What underlies personality disorders?
As with other mental health conditions, genetic and environmental factors contribute to the development of personality disorders. The genetic link is still not well understood 17 18 and evidence on heritability is limited. 19 Genetic factors are thought to interact with the environment to lead to neurobiological changes. 20 Epigenetic effects of the environment on gene expression are also increasingly recognised. 21 Antenatal adversities (eg, increased stress in utero) 22 and adverse childhood experiences, 23 including physical, emotional, and sexual abuse, neglect, and parental mental illness, are associated with an increased risk of a diagnosis of personality disorder in adulthood. 24 In particular, a meta-analysis found that individuals with borderline personality disorder are 13.91 times more likely to report childhood adversity than non-clinical controls and 3.15 times more likely than other people with other psychiatric conditions. 25
Several theoretical models exist that can be clinically useful. Attachment theory provides a model for the understanding of how early disruptions in the infant-caregiver relationship may influence regulation of affect and development of the self. 26 Psychoanalytical object relations theory explains how early internal self and other (object) representations and “patterns” of relating are repeated in adulthood. 27 Adapted cognitive behavioural theory focuses on the effects of conditioning (eg, through invalidating environments) on emotional, cognitive, and behavioural patterns that develop in adulthood. Understanding the complex multi-causal pathways leading to a personality disorder diagnosis can reduce stigma. 28
How common are personality disorders, and who is affected?
Relatively little epidemiological research has been conducted in personality disorders, but estimates of prevalence suggest as many as one in 10 people in the general population has a personality disorder. 29 30 A 2000 study of 303 consecutive primary care attenders estimated that one in four met the criteria for a diagnosis. 31 Estimates of the prevalence in secondary mental healthcare are variable because of heterogeneity of samples, but two literature reviews reported that up to 52% of psychiatric outpatients and up to 70% of patients in inpatient and forensic settings met the criteria for personality disorders, 32 and 12% of patients in outpatient psychiatric clinics and 22% of patients in inpatient psychiatric clinics for borderline personality disorder. 33
Antisocial personality disorder is consistently more common in men than women. 34 There is possible measure or clinician bias in diagnosis of borderline personality disorder in lesbian, gay, and bisexual patients 35 and risk of symptom mislabelling in minority groups, differences in healthcare seeking behaviour between men and women, and mental health risks and barriers for LGBTQ+ populations. 36 Correlation exists between a diagnosis of personality disorder and low socioeconomic status, urbanicity, lower educational attainment, occupational difficulties, and marital discord. 34 Sparse evidence is available on ethnic variations. 37 Clinicians may find it helpful to expand their understanding of the impact of racial trauma 38 and barriers to accessing healthcare for people in black, Asian, and ethnic minority populations.
Prevalence in older populations is about 10%. 39 An underlying and undiagnosed personality disorder may become evident for the first time in older age if disruptions occur in a previously stable life (eg, new onset illness, loss of partner), which lead to decompensation. Differential diagnoses when making a new diagnosis of personality disorder in older people are important (eg, late onset or relapse of other mental or physical illness, including dementia, malignancy, or substance misuse). Evidence suggests a decline in diagnosis of borderline personality disorder with progression of age, indicating a natural improving course in this group. 40 41
How are personality disorders classified?
In ICD-11, 42 released by the World Health Organization in 2018, the clinician is invited to: a) identify the presence of a core problem in functioning of self and interpersonal relating; b) its level of severity (mild, moderate, severe); and c) its main traits : negative affectivity, detachment, dissociality, disinhibition, anankastia (ie, obsessive-compulsive traits), and whether a borderline pattern exists. This classification marked a radical shift away from the categorical classification adopted in ICD-10, DSM-IV, and DSM-5 ( table 2 ), 43 and it allows primary care clinicians to adopt a more pragmatic approach to recognising personality disorder: to look for a core problem, its functional impact and severity, and how this might present in the patient’s relationships and during clinical appointments. 44
Classification systems
DSM-5, which otherwise preserves the categorical approach of DSM-IV, attempts a “hybrid” approach between the categorical and dimensional models, by including an “alternative model” ( table 2 ).
For non-specialist clinicians, awareness of categorical dimensions might be useful, but finer differentiation may be left to the specialist.
How to approach suspected personality disorder
Establishing a specific working framework for the assessment and management of personality disorder can help to prevent exclusion, provide a safe and containing environment, and instil hope. General principles include an open, empathic, and non-judgmental attitude, attentive listening, active and genuine interest, and validation of the patient’s experience. Use a trauma informed approach, which recognises the high prevalence and complex impact of traumatic experiences in personality disorders. 45 46
Box 1 lists some helpful indicators for suspecting personality disorder. Clinicians may be able to incorporate these in their clinical encounters and use them to communicate their patient’s stories and needs to colleagues, while recognising that this list is not exhaustive.
Indicators for personality disorder in non-specialist settings
Strong indicators.
Negative affectivity and affective dysregulation (rapid mood changes, low mood, anxiety, anger, detachment)
Impulse dysregulation (risk taking behaviours, sexual promiscuity, alcohol and substance misuse)
Interpersonal problems: a) In “outside” life (eg, turbulent relationships, violence, dependence, avoidance, isolation); b) In the clinical encounter (eg, increased use of resources, recurrent crises, feeling stuck). In particular, turbulence and volatile relationships tend to be characteristic of borderline personality disorder difficulties
Strong emotional reactions in the clinician during the clinical encounter. Unusual departures from established clinical practice (eg, prescribing out of the ordinary, allocation of clinical time, working outside expertise)
Poor responses to evidence based treatments for other mental health conditions (anxiety, depression, post-traumatic stress disorder)
Additional indicators to look for
Cognitive-perceptual symptoms (rigid or bizarre ideas, antagonism, lack of trust, unusual dissociative or quasi-psychotic symptoms)
Evidence of self-injurious behaviours (scars, marks on skin), significant history of deliberate self-harm and suicidal behaviours
Medically unexplained symptoms 47 48
Parents of children presenting with evidence of deficits in the home environment (eg, neglect, abuse, social adversity, or trauma)
Early adversity and history of trauma (but do not adopt a mechanistic approach, assuming or excluding a diagnosis based on the presence or absence of adversity and trauma)
Childhood diagnosis of emotional disorder, disrupted behaviours, or conduct disorder
Longer initial appointments may be necessary and, where possible, having consistency rather than multiple involved clinicians. Allow time to build trust, tolerate any initial confusion, be open about the service limitations, and adopt an understanding and curious attitude if the person’s requests and demands seem excessive. Strong emotional reactions to patients (positive or negative), observation of unexpected dynamics at play in the doctor-patient interaction or within the team, or deviations from well established practices, may alert the clinician to unconscious repetitions of “patterns” of relating that may complicate the clinical encounter. 49 50
Anxiety, depression, sequelae of a recent trauma or life crisis, or requests relating to an existing diagnosis may in fact be indicators of a personality disorder. Aim to look beyond the apparent presenting symptom and try to understand the individual’s circumstances and their point of view. Simply put, it is essential to get to know a patient and their story. When you formulate their difficulties, try to cover the areas of: 1) sense of self; 2) interpersonal relating; 3) educational and vocational attainment; 4) risk assessment (self-harm and suicide, aggression and violence, risks to dependants and children, risk from others including domestic abuse); 5) hopes and expectations of clinical care. Involve families or carers when appropriate and, with the patient’s consent, seek information from other involved agencies.
Screening tools in primary care are of limited use, but the standardised assessment of personality scale is concise and may help in identifying a personality disorder. 51 Standardised tools can otherwise be used as indicated for mental health screening purposes. 52 Urine drug testing, neuro-imaging, and blood testing may be appropriate in specific cases to exclude other pathologies (eg, in addiction, older adults, and the perinatal period).
Management in primary care
Caring for people with personality disorders in primary care requires a person centred approach that promotes open dialogue and reduces stigma. The goal is not to provide a cure, or “fix” some underlying fault, but to engage in a curious and compassionate way with the person experiencing distress in their attempt to understand and manage their painful experience, even when their wishes and expectations may initially seem unclear or confusing ( box 2 ).
Patient and clinician perspectives on managing personality disorder in primary care
We asked two people to share their experiences of personality disorder. One is a practising GP in the NHS, the other a patient with experience of primary care services during their journey with personality disorder.
It takes a lot to recognise the need for additional support, and once this decision has been made, it can be the start of a very long and emotionally exhausting journey. For most, this starts with a visit to the GP, with the expectation of understanding and perhaps even some answers—medical or other. Someone who can listen without judgment, take the time to get to know us, and show compassion are just a few qualities that can save further distress or misunderstandings on either side. We may not know what we need, or how even to communicate (or comprehend) our thoughts and feelings in a 10 minute appointment. Prior experiences of rejection, abandonment, or attachment difficulties can make it really hard to put our trust in others, including healthcare professionals. Added to this, hidden past or current traumas hinder openness; building a trusting relationship is therefore key to progressing our journey.
We learn to view the world as an unsafe place, where we will not be believed, and that we are not worthy of care. Looking and sounding “OK,” we can come across as malingering—not a term I would choose, but one that fits my interpretation of the invalidating response received at times. All of these are experiences from my own journey over the past 25 years. On reflection, I did expect answers but didn’t really know the question. Part of this journey was through a maze of diagnoses and unhelpful treatments, both medical and psychological. Being referred to services that declined me due to my stigmatising diagnosis, falling between private sector care and the NHS, and repeated assessments or referrals became exhausting and frustrating. The one constant in this journey was my GP practice, perhaps the only place that cannot turn me away and hopefully does not judge based on a mental health label (which I might not even agree with). While I can now see that the remit of a GP is very broad, having someone in the practice that has the skills, time, and compassion to listen and support us in thinking what may be helpful can be invaluable and even life changing.
The question of how we, as a primary care team, can work with people experiencing relational and personality difficulties becomes an almost daily one. In a wider context, primary care unfortunately is becoming increasingly transactional and reactionary, a box ticking exercise, where the complexity of human interaction, continuity as a therapeutic ingredient, and empathy are being replaced by a conveyor belt-like service with e-consultations or orders, and expectations of next day-type delivery by exhausted and burnt out workers. Our commissioners are increasingly relying on numerical indicators to monitor the quantity and quality of our work.
One of the biggest difficulties my team and I face when interacting with a patient with personality disorder is the sense of isolation. Every interaction, especially with someone in need, can be challenging, more so if one has difficulties relating to a person. Lack of trust, breakdown of communication, complexity of presentation, suicidal risk, threatening or dismissive attitude, inconsistencies, lack of a descriptive or explanatory framework can all become barriers to effective clinical practice because they act as magnifying lenses to the difficulties all of us—clinical and non-clinical staff—may experience, and because of the complexity of human nature. This is when I feel most inadequate, full of stress, defensive, persecuted, confused, and hopeless, and this is an experience I share with my team members. But with a reflective space and effective communication between my team and colleagues and the wider mental health and care ecosystem, we can achieve miracles.
Structured management starts with working collaboratively with the person to produce a formulation and understanding of the nature of their difficulties. Consistency, clear communication, and clear boundaries are key. A “contract” between the patient and clinician that will guide their work together from the outset may be helpful 49 to provide clarity about the role and limitations of primary care, establishing clinician and patient responsibilities and modelling realistic expectations. 53
Box 3 outlines management principles, strategies, and techniques that can be used by generalist clinicians and teams.
Management principles, strategies, and techniques
General principles: open, empathic, and non-judgmental attitude; attentive listening; active and genuine interest; validation of the patient’s experience; positive regard that promotes hope; readiness to acknowledge own limitations and mistakes
Acknowledge the patient’s feelings and be aware of your own emotional responses
Be mindful of trauma and its impact on the patient’s life and help-seeking behaviours, and actively aim to avoid re-traumatisation
Be clear and transparent about procedures
Use person centred, co-produced, and mutually agreed treatment plans or “contracts”: negotiated agreements on how the patient and clinician will work with one another to frame the relationship, set goals, establish clear roles and expectations, and manage deviations from what has been agreed
Consider and discuss the use of emotion regulation, distress tolerance, and grounding techniques (muscle relaxation, breathing skills, self-soothing using one’s senses, silence, mindfulness and meditation, yoga postures, exercise)
• Use techniques aimed at improving mentalising during consultations (mentalising refers to the process by which we make sense of ourselves and others, in terms of subjective states and processes (thoughts, feelings, intentions) and impaired mentalising is a core feature of borderline personality disorder 53 )
Share an interview structure plan with the patient, slowing down a chaotic interview and “rewinding” to previously unresolved discussions
Identify and name the underlying emotion: this can help reduce the patient’s levels of anxiety and emotional arousal (anger, elation, sadness/despair, fear) during a consultation
Validate and reflect on the patient experience
Describe your own reflections on the discussion
Invite the patient to reflect from the third position: “What would you tell a friend in this situation?”
Use medications thoughtfully when necessary, and strive to rationalise unnecessary prescribing and polypharmacy; avoid prescribing or changing medications during crises
Encourage lifestyle changes and discuss sleep routines before considering the use of sleeping tablets
Be mindful of mental health comorbidities and treat accordingly, or seek specialist input when required (eg, mood and anxiety disorders, post-traumatic stress disorder, eating disorders, autism spectrum disorder, 54 attention deficit/hyperactivity disorder, intellectual disability 55 56 )
Address problematic alcohol and substances use
Be mindful of increased physical health morbidity, and consider physical health needs
Discuss social needs and encourage structured meaningful activity and social connectedness. Involvement of a primary care mental health practitioner, a social prescriber and peer coach, social care, and third sector organisations may be helpful when indicated
A shared sense of purpose and a culture of cooperation
Team cohesion and mutual support
Formalised regular supervision and reflective practice
Readiness to engage with difficult clinical situations and consider judgment or bias when identified in either colleagues or patients
A culture of reflection and adherence to agreed plans and strategies
Safety management
Establish clear pathways for safety and crisis management
Differentiate and identify an acute escalation in chronic risk and avoid complacency
Have shared safety management plans that are comprehensive and accessible
Encourage strategies to minimise harm in patients who self-harm
Adapting services to meet patients’ needs
Consider what adjustments in service delivery and staff training might improve patient care ( box 4 ). For some patients a long term and trusting relationship with a reliable GP who is genuinely interested may become key in their path to living a more fulfilling life. Chronic difficulties in clinical relationships can develop, however; unhelpful or entangled situations may arise, and this is not rare. Specialist advice or consultation 57 58 may help to resolve this, and reflection can lead to valuable learning from experience for the clinician. Avoid working in isolation, and consider ways to promote reflective spaces and staff wellbeing, to prevent burnout. 59
What can I put in place in my service?
Need specific services and adjustments.
Provide structure and consistency (allocate a named clinician)
Offer scheduled, regular appointments—do not adopt a reactive, crisis management practice
Consider longer appointments (20-30 minutes)
Consider planned telephone contacts with a named doctor
Have reliable and transparent crisis management plans and pathways
Offer bespoke training for first line clinical and reception staff
Put in place regular reflective practice groups across disciplines
Organise peer support, supervision, and clinical practice based meetings with mental health team specialists and/or a local psychiatrist
Establish reliable pathways of communication with local mental health specialists
Offer a tailored-to-need service to resolve complaints and conflict
Integrate a trauma informed approach into policies, procedures, and practices
Shared care, or blended primary and secondary team working, requires reliable communication pathways between all involved agencies. With permission from the patient, make transparent to involved services any treatment “contract” that has been agreed. Openly acknowledge, discuss, and reflect on any deviations from mutual agreements.
Managing safety
Non-suicidal self-injury (self-harm) is common in people with borderline personality disorder (65-80% of cases). 60 The risk of suicide is many times greater than in the general population, 33 with estimates suggesting that up to 10% of people with borderline personality disorder will die by suicide. 61 Plans for safety and crisis management are clinically indicated and actively researched. 62 People who have a personality disorder and are in crisis should access specific local protocols and pathways tailored to their needs. Document up-to-date assessments of the level of risk to self and others, and any safeguarding issues concerning the patient or dependants. Specialist or emergency psychiatry is appropriate for serious and escalating risk patterns.
Medications
Many people with a personality disorder take several drugs, despite an absence of evidence to support the use of any specific medication for the conditions. 63 64 Guidelines from the National Institute for Health and Care Excellence recommend treatment of comorbidities where present as indicated. 65 Recent research highlights the complex interpersonal dynamics that may influence prescribing, especially in patients with personality disorder. 66 67 Reactive prescribing without clear direction, especially during crises, may become a problem. When prescribing, either for physical or mental health, discuss in advance (and in a clear manner) goals, duration of treatment, target symptoms, and potential side effects. Seek informed consent, psychoeducation, and reflection on expectations. 68 69 Consider psychological aspects of resistance to treatment, poor adherence, and medication misuse, and be curious about the meaning of taking and prescribing medication. 70 71 72 If you prescribe without a clear clinical rationale, consider whether this is driven by your emotional reactions in your encounter with the patient. It may be practical to treat symptoms such as insomnia with short courses of medications. We advise specialist input if considering antipsychotic or mood stabilising medications.
When to refer and what to expect
Availability of specialist treatment may vary by region. Involvement of community psychiatry and/or specialist services for personality disorder is indicated for: a) diagnostic clarification; b) assessment of readiness for and choice of specialist treatment; c) case consultation regarding management difficulty and increased risk. Referral to non-specialist talking therapies services—in England through Improving Access to Psychological Therapies (IAPT)—may be appropriate for personality disorder of mild severity and when a full diagnosis is not met. These services may also be appropriate for cases in which focused psychological treatment of a comorbid mental health condition is indicated, if relevant training and resources are available in local provision, but IAPT services may not meet the patients’ needs otherwise. 73
The presence of a diagnosis does not in itself indicate psychological readiness for a specialist treatment programme. The specialist assessment can be demanding, and treatment is not always available or appropriate. In the UK, available specialist programmes are lengthy and require commitment, so that timing and competing priorities need to be considered in advance. Unstable living conditions, uncontrolled alcohol or substance misuse, severe eating disorder, serious risk of harm to self or others, and vulnerability to harm from others may need to be tackled first, with relevant specialist input if necessary (eg, addiction or eating disorder services, adult social services). Canvass patient views, preferences, and goals, based on any previous experience of psychological therapies, at an early stage. 74
Several evidence based treatments, mainly for borderline personality disorder, are available in secondary and tertiary care in the NHS ( table 1 ). No single modality stands out in terms of efficacy, 75 and sometimes multiple treatment attempts may be needed. Brief treatments (such as cognitive behavioural therapy) might not be helpful, and the choice and sequencing of treatments requires specialist involvement. 76
Contact other agencies (eg, probation services, social services, social support agencies for housing, occupation, and activities), as necessary, for support.
Education into practice
What training opportunities could be made available to staff to support their interactions with people who have a personality disorder?
Can you identify one specific barrier that people with a personality disorder may face when trying to access your service?
Useful resources (mainly UK based)
For clinicians.
National Institute for Health and Care Excellence. Personality disorders: borderline and antisocial: https://www.nice.org.uk/guidance/qs88 Updated June 2015.
World Health Organization, ICD-10 Classifications of mental and behavioural disorder: Clinical descriptions and diagnostic guidelines, World Health Organization, 1992: https://icd.who.int/browse10/2016/en
·World Health Organization, ICD-11 Classifications of mental and behavioural disorder: Clinical descriptions and diagnostic guidelines, World Health Organization, 2018: https://icd.who.int/browse11/l-m/en
Balint Society: https://balint.co.uk . Balint group membership provides a space to think about those encounters which leave professionals drained, puzzled, or stuck
Standardised Assessment of Personality—Abbreviated Scale (SAPAS): https://www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/standardised-assessment-of-personality-abbreviated-scale-sapas-preliminary-validation-of-a-brief-screen-for-personality-disorder/26FB730F35F54B952381AA9C662FF8C2
The Knowledge and Understanding Framework (KUF) national training programme: https://www.westlondon.nhs.uk/our-services/adult/mental-health-services/cassel-hospital/consultation-and-training-services and The National KUF Hub https://twitter.com/nationalkufhub
“Six levels of validation” interpersonal effectiveness skills resource: https://dbtselfhelp.com/dbt-skills-list/interpersonal-effectiveness/validation/
Safer care for patients with personality disorder. National confidential inquiry into suicide and homicide by people with mental illness, University of Manchester. 2018: https://documents.manchester.ac.uk/display.aspx?DocID=37564 Related educational videos “Safer care for patients given a diagnosis of personality disorder: a learning resource”: https://sites.manchester.ac.uk/ncish/resources/safer-care-for-patients-given-a-diagnosis-of-personality-disorder-a-learning-resource/
NHS England and NHS Improvement and the National Collaborating Centre for Mental Health, The Community Mental Health Framework for Adults and Older Adults, September 2019: https://www.england.nhs.uk/wp-content/uploads/2019/09/community-mental-health-framework-for-adults-and-older-adults.pdf
Office for Health Improvement & Disparities Guidance: Working definition of trauma-informed practice and resources: https://www.gov.uk/government/publications/working-definition-of-trauma-informed-practice/working-definition-of-trauma-informed-practice
For patients, families, and carers
For immediate help.
NHS 111 (option 2) can help if you have an urgent medical problem and you’re not sure what to do. Visit https://111.nhs.uk (for people aged 5 and over only) or call 111 (available 24 hours a day, 7 days a week)
With life threatening emergencies, call 999 or go to the nearest emergency department
The Samaritans are there to listen 24 hours a day. Call on 08457 90 90 90 or visit the website at https://www.samaritans.org .
SANEline is a national out-of-hours mental health helpline offering specialist emotional support, guidance, and information to anyone affected by mental illness, including family, friends, and carers. Available every day from 4.30 pm to 10.30 pm on 0300 304 7000: https://www.sane.org.uk/what_we_do/support/helpline
Most areas have a mental health crisis team available 24 hours a day; their contact details should be available via the local council or social services, or they can be contacted via hospital emergency departments.
Text SHOUT: a 24/7 UK based volunteer led text service for anyone in crisis. Developed by the Mental Health Innovations charity: https://www.giveusashout.org/
Other resources
MIND. Personality Disorders leaflet: https://www.mind.org.uk/information-support/types-of-mental-health-problems/personality-disorders/about-personality-disorders/
The National Education Alliance for Borderline Personality Disorder: https://www.borderlinepersonalitydisorder.com/consumer-recovery-resources/ A resource for families and people in recovery, education and training for professionals. (USA)
·The National Service user Network (NSUN) weekly bulletin offers a summary of involvement opportunities as well as policy updates: https://www.nsun.org.uk/
Mindfulness meditation—online resources that some may find helpful: https://www.freemindfulness.org/
Cognitive behavioural therapy based self-help resources and worksheets: https://www.getselfhelp.co.uk/
Dialectical behaviour therapy based self-help resources and worksheets: https://dbtselfhelp.com/
National self-harm network: https://www.nshn.co.uk/
Lifesigns: a user-led organisation working around self-injury: https://www.lifesigns.org.uk/
Rachel Reiland, Get Me Out Of Here: My recovery from borderline personality disorder, Hazelden Publishing, 2002.
Self-injury support: https://www.selfinjurysupport.org.uk/
Multimedia resources
Borderliner Notes: The BORDERLINE film interview Archive: https://www.youtube.com/borderlinernotes
Early Years Parenting Unit at the Anna Freud National Centre for Children and Families, Video Series: EYPU—What is “personality disorder”? https://www.youtube.com/watch?v=38EBpzJDodg What is meant by “good mentalisation”? https://www.youtube.com/watch?v=R5kFPpAMDF0
BBC, Radio I & IXtra Stories. Living with BPD: https://www.bbc.co.uk/programmes/p0700vh4/
BBC Radio 4. Narcissism: https://www.bbc.co.uk/programmes/p06y2j6v
Personality Disorder—subtitles. A film produced by the RCPsych Public Engagement Committee and Damn Fine Media: https://www.youtube.com/watch?v=OnwVTrZcn5s/
Adverse Childhood Experiences (ACEs), Public Health Network Cymru. A short film produced for Public Health Wales and Blackburn with Darwen Local Authority: https://www.youtube.com/watch?v=YiMjTzCnbNQ
RethinkBPD: In conversation: Talks on borderline personality disorder and recovery: https://rethinkbpd.org/
Ending exclusion: research and care for people with complex emotional needs #MHQT: A recording of panel discussion around NIHR mental health policy research unit activities: https://youtu.be/aQoQh66D6N4
Public Health Wales, Adverse Childhood Experience (ACE) and Adult Mental Well-Being Wales infograph. 2016: http://www.wales.nhs.uk/sitesplus/documents/888/embargoed%20final%20-%20ace%20%26%20mental%20well-being%20infograph%20e.pdf
Selected readings
Gask L, Evans M, Kessler D. Personality disorder. BMJ 2013;347:f5276
Schrift M, Personality disorders. BMJ Best Practice. 2019
RCPsych Position statement, services for people diagnosable with personality disorders. 2020
NIMHE Personality disorder: no longer a diagnosis of exclusion—policy implementation guidance for the development of services for people with personality disorder. 2003
NIMHE Breaking the cycle of rejection. The Personality Disorders Capabilities Framework. 2003
Bolton W, Lovell K, Morgan L, Wood H, Meeting the challenge, making a difference. Working effectively to support people with personality disorder in the Community. Project report, Department of Health, London. 2014. http://repository.tavistockandportman.ac.uk/864/1/Heather_Wood_-_MeetingTheChallenge.pdf
Mind, Centre for Mental Health, Royal College of Nursing, The British Association of Social Workers, Royal College of General Practitioners, The British Psychological Society, Anna Freud National Centre for Children and Families, Barnet, Enfield, and Haringey Mental Health NHS Trust. Shining lights in dark corners of people’s lives, The consensus statement for people with complex mental health difficulties who are diagnosed with a personality disorder. 2018: https://www.mind.org.uk/media/21163353/consensus-statement-final.pdf
How patients were involved in the creation of this article
JP, a co-author on this paper, has lived experience of personality disorder. Her insights were essential in giving it its final form. An anonymised patient perspective statement has also been included with consent from the author.
Contributors: OKB is the lead author and guarantor of the content of the paper. OKB designed the initial outline and OKB, DC, JP, SS and TL all contributed equally thereafter to writing the final version.
Competing interests: The BMJ has judged that there are no disqualifying financial ties to commercial companies. The authors declare the following other interests: none.
Further details of The BMJ policy on financial interests are here: https://www.bmj.com/about-bmj/resources-authors/forms-policies-and-checklists/declaration-competing-interests
Provenance and peer review : commissioned; externally peer reviewed.
- Hoffman P ,
- Global Alliance for Prevention and Early Intervention for Borderline Personality Disorder
- American Psychiatric Association
- ↵ Livesley J. Handbook of personality disorders. Second Edition: Theory, research and treatment. Guilford Publications, 2018.
- Sheridan Rains L ,
- Sheehan L ,
- Nieweglowski K ,
- Chartonas D ,
- Kyratsous M ,
- Dracass S ,
- Stoffers JM ,
- Choi-Kain LW ,
- Masland SR ,
- Jenkins JA ,
- Bateman A ,
- O’Connell J ,
- Lorenzini N ,
- Gardner T ,
- Simsek-Duran F ,
- McCormick B ,
- Attwood G ,
- Miloseska K ,
- Diamond D ,
- Yeomans F ,
- Martín-Blanco A ,
- Moffitt TE ,
- Reichborn-Kjennerud T
- Gescher DM ,
- Hillemacher T ,
- Frieling H ,
- Brannigan R ,
- Tanskanen A ,
- Huttunen MO ,
- Battle CL ,
- Johnson DM ,
- Palmier-Claus J ,
- Branitsky A ,
- Mansell W ,
- Warwick H ,
- Johnson BN ,
- Clouthier TL ,
- Caligor E ,
- Hörz-Sagstetter S ,
- Volkert J ,
- Gablonski TC ,
- Torgersen S ,
- Kringlen E ,
- Jenkins R ,
- Blizard R ,
- Beckwith H ,
- Ellison WD ,
- Rosenstein LK ,
- Morgan TA ,
- Zimmerman M
- Roberts A ,
- Rodriguez-Seijas C ,
- Semlyen J ,
- McGilloway A ,
- Nicolas G ,
- Abrams RC ,
- Horowitz SV
- Álvarez-Tomás I ,
- Guilera G ,
- Zanarini MC ,
- Frankenburg FR ,
- ↵ World Health Organization. International statistical classification of diseases and related health problems (11th Revision). 2018. https://icd.who.int/browse11/l-m/en
- van der Kolk BA
- Stubley J ,
- ↵ Royal College of General Practitioners and the Royal College of Psychiatrists, CR152, The management of patients with physical and psychological problems in primary care: a practical guide, Report of a joint working group of the, January ref incomplete??? 2009.
- Hatcher S ,
- Walters P ,
- Thornicroft G ,
- ↵ Schrift M, Personality disorders. BMJ Best Practice. 2019.
- Bateman AW ,
- Lovejoy C ,
- Cassidy S ,
- Allison C ,
- Baron-Cohen S
- Carrington A ,
- Herbert A ,
- British Medical Association, Caring for the Mental Health of the Medical Workforce
- Cornelius J ,
- Borschmann R ,
- Barrett B ,
- Hellier JM ,
- Crawford MJ ,
- Bhatti SF ,
- Stoffers-Winterling JM ,
- Storebø OJ ,
- Pereira Ribeiro J ,
- ↵ National Institute for Health and Care Excellence. Personality disorders: borderline and antisocial. https://www.nice.org.uk/guidance/qs88 2015.
- Martean L ,
- Konstantinidou H
- ↵ Francois D, Roth SD, Klingman D. The efficacy of pharmacotherapy for borderline personality disorder: a review of the available randomized controlled trials. Psychiatric Ann 2015;45:431-7.
- Gabbard G ,
- Weinberg E ,
- Konstantinidou H ,
- Rogalski D ,
- Goddard E ,
- Wingrove J ,
- Roughley M ,
- Maguire A ,
- Cristea IA ,
- Gentili C ,
- Palomba D ,
- Albert EB ,
- Gunderson JG
June 18, 2018
Could Multiple Personality Disorder Explain Life, the Universe and Everything?
A new paper argues the condition now known as “dissociative identity disorder” might help us understand the fundamental nature of reality
By Bernardo Kastrup , Adam Crabtree & Edward F. Kelly
This article was published in Scientific American’s former blog network and reflects the views of the author, not necessarily those of Scientific American
In 2015, doctors in Germany reported the extraordinary case of a woman who suffered from what has traditionally been called “multiple personality disorder” and today is known as “dissociative identity disorder” (DID). The woman exhibited a variety of dissociated personalities (“alters”), some of which claimed to be blind. Using EEGs, the doctors were able to ascertain that the brain activity normally associated with sight wasn’t present while a blind alter was in control of the woman’s body, even though her eyes were open. Remarkably, when a sighted alter assumed control, the usual brain activity returned.
This was a compelling demonstration of the literally blinding power of extreme forms of dissociation, a condition in which the psyche gives rise to multiple, operationally separate centers of consciousness, each with its own private inner life.
Modern neuroimaging techniques have demonstrated that DID is real: in a 2014 study , doctors performed functional brain scans on both DID patients and actors simulating DID. The scans of the actual patients displayed clear differences when compared to those of the actors, showing that dissociation has an identifiable neural activity fingerprint. In other words, there is something rather particular that dissociative processes look like in the brain.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
There is also compelling clinical data showing that different alters can be concurrently conscious and see themselves as distinct identities. One of us has written an extensive treatment of evidence for this distinctness of identity and the complex forms of interactive memory that accompany it, particularly in those extreme cases of DID that are usually referred to as multiple personality disorder.
The history of this condition dates back to the early 19th century, with a flurry of cases in the 1880s through the 1920s, and again from the 1960s to the late 1990s. The massive literature on the subject confirms the consistent and uncompromising sense of separateness experienced by the alter personalities. It also displays compelling evidence that the human psyche is constantly active in producing personal units of perception and action that might be needed to deal with the challenges of life.
Although we may be at a loss to explain precisely how this creative process occurs (because it unfolds almost totally beyond the reach of self-reflective introspection) the clinical evidence nevertheless forces us to acknowledge something is happening that has important implications for our views about what is and is not possible in nature.
Now, a newly published paper by one of us posits that dissociation can offer a solution to a critical problem in our current understanding of the nature of reality. This requires some background, so bear with us.
According to the mainstream metaphysical view of physicalism , reality is fundamentally constituted by physical stuff outside and independent of mind. Mental states, in turn, should be explainable in terms of the parameters of physical processes in the brain.
A key problem of physicalism, however, is its inability to make sense of how our subjective experience of qualities—what it is like to feel the warmth of fire, the redness of an apple, the bitterness of disappointment and so on—could arise from mere arrangements of physical stuff.
Physical entities such as subatomic particles possess abstract relational properties, such as mass, spin, momentum and charge. But there is nothing about these properties, or in the way particles are arranged in a brain, in terms of which one could deduce what the warmth of fire, the redness of an apple or the bitterness of disappointment feel like. This is known as the hard problem of consciousness .
To circumvent this problem, some philosophers have proposed an alternative: that experience is inherent to every fundamental physical entity in nature. Under this view, called “ constitutive panpsychism ,” matter already has experience from the get-go, not just when it arranges itself in the form of brains. Even subatomic particles possess some very simple form of consciousness. Our own human consciousness is then (allegedly) constituted by a combination of the subjective inner lives of the countless physical particles that make up our nervous system.
However, constitutive panpsychism has a critical problem of its own: there is arguably no coherent, non-magical way in which lower-level subjective points of view—such as those of subatomic particles or neurons in the brain, if they have these points of view—could combine to form higher-level subjective points of view, such as yours and ours. This is called the combination problem and it appears just as insoluble as the hard problem of consciousness.
The obvious way around the combination problem is to posit that, although consciousness is indeed fundamental in nature, it isn’t fragmented like matter. The idea is to extend consciousness to the entire fabric of spacetime, as opposed to limiting it to the boundaries of individual subatomic particles. This view—called “ cosmopsychism” in modern philosophy, although our preferred formulation of it boils down to what has classically been called “ idealism ”—is that there is only one, universal, consciousness. The physical universe as a whole is the extrinsic appearance of universal inner life, just as a living brain and body are the extrinsic appearance of a person’s inner life.
You don’t need to be a philosopher to realize the obvious problem with this idea: people have private, separate fields of experience. We can’t normally read your thoughts and, presumably, neither can you read ours. Moreover, we are not normally aware of what’s going on across the universe and, presumably, neither are you. So, for idealism to be tenable, one must explain—at least in principle—how one universal consciousness gives rise to multiple, private but concurrently conscious centers of cognition, each with a distinct personality and sense of identity.
And here is where dissociation comes in. We know empirically from DID that consciousness can give rise to many operationally distinct centers of concurrent experience, each with its own personality and sense of identity. Therefore, if something analogous to DID happens at a universal level, the one universal consciousness could, as a result, give rise to many alters with private inner lives like yours and ours. As such, we may all be alters—dissociated personalities—of universal consciousness.
Moreover, as we’ve seen earlier, there is something dissociative processes look like in the brain of a patient with DID. So, if some form of universal-level DID happens, the alters of universal consciousness must also have an extrinsic appearance. We posit that this appearance is life itself : metabolizing organisms are simply what universal-level dissociative processes look like.
Idealism is a tantalizing view of the nature of reality, in that it elegantly circumvents two arguably insoluble problems: the hard problem of consciousness and the combination problem. Insofar as dissociation offers a path to explaining how, under idealism, one universal consciousness can become many individual minds, we may now have at our disposal an unprecedentedly coherent and empirically grounded way of making sense of life, the universe and everything.
Recent research on multiple personality disorder
Affiliation.
- 1 Unit on Dissociative Disorders, National Institute of Mental Health, Bethesda, Maryland.
- PMID: 1946019
The last decade has seen the emergence of solid research on MPD and the dissociative disorders, particularly in the area of diagnosis and clinical phenomenology. A number of other areas have been opened up or advanced considerably. The most notable of these include child and adolescent dissociative disorders; investigation of dissociative memory disturbances; studies of differential alter personality psychophysiology and switching; cross-cultural comparisons of MPD, possession, and dissociative states; and the contribution of pathologic dissociation to the symptomatology of other psychiatric disorders. Yet to be attempted, however, are prospective clinical trials and treatment outcome studies. In addition to clinical and theoretical insights, recent research provides strong evidence for the validity of the diagnosis of MPD. The repeated replication of a core clinical phenomenology demonstrates a construct validity equal to or superior to that demonstrated for most DSM-III/IIIR disorders. The ability of several independently developed instruments to blindly discriminate MPD patients from nondissociative disorder patients with high rates of accuracy supports both the construct and discriminant validity of the diagnosis; and as the astute clinical observations of the last century continue to be confirmed, MPD manifests an historical validity absent in most modern era diagnoses. In the future, arguments about the "reality" of MPD cannot confine themselves merely to attacking one aspect of the disorder but rather must confront the broad range of evidence supporting the validity and reliability of the diagnosis. The future belongs to multicenter studies, although intensive single-case and personal-case series will continue to make important contributions in some areas. The essential elements necessary to begin prospective multicenter studies are rapidly coming together. Already one multicenter structured interview study of clinical phenomenology has been completed and other studies are underway or near publication. As these collaborative research networks mature, even more ambitious studies will be attempted. Adequate funding remains the principal obstacle and must be creatively addressed in this era of budgetary shortfalls, particularly as several research networks cross international boundaries. Exceptionally gratifying is the burgeoning interest of large numbers of psychiatric residents and psychology graduate students in the dissociative disorders. Thanks to a decade of hard work, the next generation of clinicians and researchers will know a great deal more about these patients than the last.
Publication types
- Dissociative Disorders / diagnosis
- Dissociative Disorders / psychology*
- Dissociative Disorders / therapy
- Dissociative Identity Disorder / diagnosis
- Dissociative Identity Disorder / psychology*
- Dissociative Identity Disorder / therapy
- Mental Recall
- Personality Development
- Psychiatric Status Rating Scales
Multiple Personality Disorder: Fact or Fiction? Alexandria K. Cherry Rochester Institute of Technology
Multiple Personality Disorder, or MPD, is one of the most talked about and publicized disorders known and is the center of much debate and criticism. What is currently known about MPD has become common place over the past 20 years. The past two decades have shown an increase in the number of cases of MPD but there are many professionals that are skeptical about whether it even exists. It was found that the longer a clinician has been out of school, the more skeptical of MPD they become. This paper reviews what MPD is, relates it to Dissociative Identity Disorder (DID), and reviews the criticisms of the disorder. The conclusion that is reached is that DID exists and is related to MPD. There are slight differences between the two but in no way should that imply both are equally accepted. This paper also explores the reasons for the high rates of clinical skepticism.
Interest in Multiple Personality Disorder (MPD) started in Europe during the late 1800's. It has gained attention at times, like the "Eve" and "Sybil" cases, and then fallen into the background again (Pica, 1999). There are many reasons for this and many criticisms of those reasons as well. Still the theories of this disorder have survived through much criticism and tweaking. The first part of this paper explores what MPD is. Then the subject of Dissociative Disorders and Dissociative Identity Disorder, or DID, are each discussed. The next topic that is discussed is how Multiple Personality Disorder and Dissociative Identity Disorder relate and differ. Finally, the idea of Multiple Personality Disorder, being a skewed misconception created by society, and the need for a more accepted term (DID) is emphasized. This really goes back to reasons for why the popularity and recognition of Multiple Personality Disorder is ever changing. A mixture of MPD being a "popular" disorder and the unclear classification of the disorder are the major reasons for the criticism (Lilienfeld et al., 1999). These reasons are found to be justified and supported. The result is that Dissociative Identity Disorder is an excellent substitute and reclassification for what was known as MPD. Multiple Personality Disorder A basic knowledge of how Multiple Personality Disorder is described is needed to continue. MPD is hypothesized to be caused by severe childhood trauma that creates a mental split or "dissociation" as a defense against that trauma (Spanos, 1994). The different personalities that occur are called alters. These different parts develop separately and in adulthood help the sufferer deal with stress by expressing resentment or help calm the main personality. Each patient possesses two or more selves and each identity has it's own mood, memories, behaviors, and experiences. The disease theory of Multiple Personality Disorder is that unhappiness in adulthood stems from trauma in childhood (Gleaves, Hernandez, & Warner, 1999) and the trauma is so severe that the individual creates multiple identities to cope with it (Spanos, 1994). The severe trauma is thought to be a result of physical or sexual abuse in childhood. Likewise, most modern patients are women who have been diagnosed with other disorders before being diagnosed with MPD. This is because the intense trauma caused by abuse may create other disorders as well. Because it is associated with other disorders, it was not long before MPD appeared in the Diagnostic and Statistical Manual of Mental Disorders. It first appeared in the 3rd edition (DSM-III); however the name was changed to Dissociative Identity Disorder in the DSM-IV (Dunn, 1992). Dissociative Disorders and Dissociative Identity Disorder Unlike Multiple Personality Disorder, which is more like a disease, where a person has it or does not have it, most professionals feel that dissociation ranges from a "normal" state, daydreaming, to more pathological forms (Waller, Putnam, & Carlson, 1996). So it's not hard to conclude that Dissociative Disorders are rather rare but dissociative experiences are very common (Kihlstrom, Glisky, & Angiulo, 1994). The next step is to explore the most common personality traits that are related to dissociation. These are hypnotizability, absorption, fantasy proneness, and some aspects of openness to experience (Spiegel, & Cardeña 1991). These can be risk factors for dissociative problems. A clinician named Janet, in 1889, who worked with hysterics at the Salpertriere, felt that dissociation is a response to stress but some people are predisposed to the disorders (Kihlstrom, Glisky, & Angiulo, 1994). Janet also coined the term dissociation which was used to describe the split in consciousness that resulted when patients were exposed to traumatic events (Pica, 1999). From his theories it was found that there are distinguishable types of Dissociative phenomena. Dissociative Disorders are groups of syndromes that at the core alter the sufferer's consciousness, affecting memory and identity, which also follow Janet's work (Kihlstrom et al., 1994). Janet also theorized about when vulnerability was at its highest. The developmental window of vulnerability is 18 months to 8 years old (Pica, 1999). This is important because it helps to predict how many alters may appear. There is a significant negative correlation between the age of appearance of an alter personality and the number of personalities. This can bring up other arguments, which are not covered in this paper, regarding Freudian explanations. Measurement It is easier to understand a disorder if one knows how it is measured. Scales like the Dissociative Experiences Scale (DES) measure how dissociated a patient is (Waller, Putnam, & Carlson, 1996). There are also other measures that will not be covered here (e.g., Watson, 2003). The DES was created in the mid-1980s by Carlson and Putnam to address two deficits in the current body of knowledge: (a) a need for a test to detect dissociative disorders and (b) the need to quantify dissociation for research studies. This scale is the most widely used for this purpose. The DES measures are related to: amnesia, depersonalization/derealization, and absorption. Amnesia is evidence that an individual has engaged in complex behavior that they have no memory of or the experience of "snapping out of it" in the middle of an activity and having little or no idea how they got there. Depersonalization or derealization is out of body experiences and other extreme forms of amnesia. Absorption is losing contact with current surroundings. Another measure that is sometimes used is Hypnotic Susceptibility. This may be due to the fact that historically Multiple Personality Disorder has been viewed as an artifact of hypnosis and related to fantasy, suggestibility, and hysteria (Cormier & Thelen, 1998). Fantasy proneness, absorptions and imaginative involvement are other diatheses, for reasons stated already. A person with a high degree level of imagination or someone who has vivid dreams may score high on these types of tests. The real difference between these individuals and a person with Dissociative Identity Disorder is that the dreams of someone without the disorder is the reality of the afflicted. The Next Step Multiple Personality Disorder is among the most historic of disorders dating back to ancient forms of shamanism and demonic possession (Pica, 1999). The idea of multiple identities is present in many cultures but there are distinct differences (Spanos, 1994). For example, shamanism and demonic possession are respected and practiced events in some cultures. There are also similarities between cultures. The major similarity is that these individuals are more influenced by hypnosis and more able to enter a dream state because of their ability to dissociate. Even with some similarities, it suggests that MPD is not cross-cultural. This also raises one of the major criticisms of MPD. The criticism is that Multiple Personality Disorder is a form of manipulation and both the client and clinician can be at fault. Some professionals feel that MPD is a tactic, of the client, to manipulate others into felling sorry for them or for them to get what they want. Therapists can also help to mold the patient into acting like they have MPD if they really have some other disorder (Spanos, 1994). Mental health professionals express concern that MPD is created through hypnosis, demand, suggestion or shaping by the therapist (Cormier & Thelen, 1998). The other general feeling is that MPD is really borderline personality disorder or schizophrenia. This raises the question as to whether most cases of Multiple Personality Disorder are really another condition altogether. MPD is diagnosed with less accuracy than schizophrenia and the two are confused with each other frequently (Hayes & Mitchell, 1994). Could this be because one is frequently mistaken for the other, or because professionals in the field are skeptical about MPD? A survey administered by Hayes and Mitchell seems to point in the later direction. 24% of most professionals are skeptical of MPD. Skepticism is defined as the inclination to doubt. Even though doubt is sometimes good, in excess, it could be detrimental. They found that skepticism and knowledge of MPD are inversely related. The correlation was mild and there was a low response rate to the questionnaire. So it would probably be beneficial to explore this situation more, before any conclusions on diagnosing MPD are made. Nevertheless, many professionals still feel that Multiple Personality Disorder should not be a diagnostic entity (Cormier & Thelen, 1998) even though some feel that there have been numerous, nationwide, consistent clinical reports done supporting it (Gleaves, Hernandez, & Warner, 2003). Since the first argument of skepticism has been ruled out, an analysis of the construction of MPD must be made. In Spanos' 1994 exploration on the subject he concluded that MPD is socially constructed where the characteristics of the disorder change over time to meet the changing expectations. The support for this argument is the changes between cultures, from above, and the changes over time. Since the 19th century the number of identities has gone from 2 or 3 to greater than 20, sometimes reaching 100. Also today animal alters are acceptable for an identity. The last big one is that when MPD was first recognized convulsions was one of the major symptoms but now it is not. The conclusion of Spanos' argument is that the expectations of people with the identities and the reaction of the audience are different across time and cultures. To recap, the major arguments against Multiple Personality Disorder are that it is a form of manipulation, from either the client for clinician, it should really be diagnosed as something else, and that it has been socially constructed. Reclassification as Dissociative Identity Disorder would help to relieve these criticisms. In the pervious section it is clear that the disorder has a strong classification bases, and is clearly defined. This will make it harder for people to feign the disorder, easier to diagnose correctly, and remove any doubt of its being socially constructed. Conclusion This paper has shown what Multiple Personality Disorder and Dissociative Identity Disorder are, how they are different and explored the major criticisms of MPD. Multiple Personality Disorder occurs when a child is abused at a young age and their personality splits into several alters to help them deal with the stress. It is very unclear what the necessary traits that a person needs in order to classify as MPD. Dissociative Identity Disorder is more representative of how professionals feel the disorder is. It is a response to stress, not necessarily child abuse, in which the patient reverts into a dreamlike state where more than one identity may appear. The patient is generally unaware of these other personalities and may not remember at all what has occurred during their laps in time. It is very apparent in the end why the name and classification needed to be changed. There are subtle differences between Multiple Personality Disorder and Dissociative Identity Disorder that help to correct the misconceptions surrounding MPD. Since this disorder is so widely publicized and criticized it is hard to keep a distinct definition to it. The major criticisms are that since Multiple Personality Disorder has been a popular one as early as the 1800's, there has been ample time for the classification of the disorder to be distorted. The other criticism is that since the disorder is under the public eye there are several clinicians and clients who try to feign the disorder. Because of this, there are many professionals who are skeptical about diagnosing MPD. The last criticism is that MPD is really something else. There have been instances where MPD should have been diagnosed as schizophrenia or borderline personality disorder and vise versa. The reclassification to Dissociative Identity Disorder seems to help reduce all of the problems that have arisen. Hopefully this classification will not alter with time and therefore keep criticism of it to a minimum.
Peer Commentary Multiple Personality Disorder and Dissociative Identity Disorder Are One and the Same Marissa D. Clopper Rochester Institute of Technology In "Multiple Personality Disorder: Fact or Fiction?" by Alexandria K. Cherry, valid criticisms are made against Multiple Personality Disorder, currently known as Dissociative Identity Disorder. I agree with Cherry that there is a long history of confusion and controversy about this so-called existing disorder. Iatrogenesis, where the therapist unintentionally shapes or causes the disorder, continues to be considered problematic in diagnosing MPD/DID. In addition, demand characteristics, hypnotizability, suggestibility, and being easily dissociable are disputes that further complicate the distinction of MPD/DID as a sole disorder (Raulin, Lilienfeld, & Katkin, 2003). Cherry implied that MPD is in a way different from DID and that by replacing the label of MPD with DID, criticisms are resolved and this disorder is clearly reclassified. However, I have to disagree with this perspective in that the change of labels resolves criticisms and clearly reclassifies the disorder. First of all, MPD and DID are just different labels that define the one and same disorder. It is not necessarily true that MPD is explicitly for those who have experienced abuse in childhood and that DID is for other forms of trauma--aside from child abuse. Both labels include all factors that potentially contribute to the development of MPD/DID along with predisposing characteristics aforementioned. Also, the main symptoms--dissociation, amnesia, multiple identities, derealization, and depersonalization--are present for both labels. Again, MPD and DID are two labels that describe the same syndrome. Nevertheless, it is possible that the renaming of MPD as DID owes to dissociation as the main symptom that leads to the formation of multiple identities. That might make the overall syndrome more comprehensible than the label of MPD in itself, which doesn't primarily affirm dissociation as the main symptom. Nevertheless, controversies remain regardless of which label is used. Experts are having difficulties in describing the exact symptoms of the disorder and diagnosing an individual with DID. A part of the problem that makes this whole issue confusing is comorbidity. True enough, there are disorders that may overlap that further complicate the distinction of DID as a separate entity. Despite comorbidity, DID has distinct symptoms that separate this disorder from borderline personality disorder and schizophrenia. Borderline personality disorder includes instability of relationships, emotions, and self-image; fears of abandonment; aggressiveness; proneness to self-harm; and strong emotions (Larsen & Buss, 2005). Nowhere does it state dissociation as one of the symptoms. Therefore, borderline is a separate disorder from DID, but may overlap. As for schizophrenia, the differential diagnosis is where "voices" are perceived to be heard. In schizophrenia, voices are perceived to come from the outside of the mind, while in DID, voices are perceived to be heard internally in the mind. By keeping to this very distinction, DID is capable of being identified exclusively. The famous case of Kenneth Bianchi indicates that the continuous redefining and specific steps in making a proper diagnosis of DID have improved. Bianchi was seen to be feigning DID because his alters did not continue consistently over time, did not act under hypnosis the way normal individuals would, and did not have behavioral changes that were witnessed by people who knew him well (Putman, Zahn, & Post, 1990). Malingering and factitious disorders and physical conditions are considered and if they exist, a diagnosis of DID is ruled out. Apparently, with more research, DID is capable of emerging as a clear and sole disorder as maintained by considering potential factors that contribute to the disorder, steps in making a proper diagnosis, and cases, such as Bianchi, that have appeared in history. DID may be continually redefined as we explore new evidence in the future. This scenario is similar to encountering a new disease that we don't formally recognize until at a point that it becomes obvious. For instance, AIDS was not known to be caused by a virus as there were various symptoms such as Kaposi's sarcoma that were thought to exist on its own, but a pattern began to emerge in the homosexual population as well as those who were exposed through using drugs (sharing dirty needles), received blood transfusions, and the like. Through research, this disease was finally recognized to be caused by a virus (HIV); thus, labeled AIDS. Overall, controversies and redefinition will continue until the disorder becomes distinctly clear; but until then, MPD and DID represent the same disorder, regardless of the labels.
Peer Commentary Dissociative Identity Disorder: With Whom Am I Speaking? Travis W. Silverman Rochester Institute of Technology In the study of Multiple Personality Disorder, a most intriguing aspect of the disorder is the number of personalities a patient experiences, as well as how those unique personalities interact within the single body. This aspect of the disorder was mentioned in the paper by Alexandria K. Cherry, "Multiple Personality Disorder: Fact or Fiction?" Due to its interesting and changing nature from patient to patient, the area of interaction and expression personalities within the patient warrants further discussion. The topic brings many questions to mind. Is there a dominant personality, and if so which is it? How many personalities reside in the patient? How does each of the personalities interact? Are they aware of each other? To better understand these questions, knowledge of what is at the base of the disorder is most helpful. Most people (those without DID) have one group containing their cognitive faculties, including recognition of the self, memory, intent, sensation, and consciousness. This grouping within the person allows for one singular sense of continuous identity, and thus a single personality. This singular identity is not present in patients with DID; instead of having one singular identity, they experience many strands of the self where there is a breakdown of the cognitive faculties. In multiple personality or dissociative identity patients, several distinct states of mind or personalities reside in one body. There is a varying range of how many personalities may be present, ranging from 2 personalities to over 20 personalities within one shared body. Each of these personalities has its own sense of self and has its own habits of thought, emotions, and memory. These identities may or may not be aware of each other. In some cases the identities are aware of each other; this is referred to as "co-consciousness"--while one personality is in control, the others are in the background, in the back of the mind, aware of what the current personality is doing and seeing what the current personality sees (Brown, 2001). A good way to think of this is as though looking at a picture or movie and being both the observer and observed. This leads to the way in which memory is experience by each of the personalities individually. When a memory is stored, it is claimed by the personality that was in control of the body at the time of the event; the other personalities would not refer to that event/memory as happening to themselves but instead to another personality. The awareness of other personalities and the system of memory claiming allows the multiple personalities to be unaware of the gaps in time allowing co-existence without question (Carter, 2003). In some cases the other personalities may not be aware of each other or may work against each other in both body and mind. In other words, one personality may seek to undo what another has done. The lack of memory may create gaps in the memory, causing the personalities to feel as though they did not exist for the period of time when they were not in control. A final aspect of the interaction of personalities is the factor of responsibility for actions. If one of the personalities is in control and commits a crime, how is the body to be held responsible? How are punishment and responsibility to be placed? The answers to these questions are more case-based than across-the-board answers. The awareness of the other personalities of the act as well as capabilities or dominance must be considered because due to the shift in personality there may also be a shift in beliefs including right from wrong (Kennett & Matthews, 2002). One personality may be more malevolent than the others. One way to tell if the personalities are aware of each other in deciding responsibility is to see how they refer to each other. Do they refer to each other as him or her, or are they unaware of the person they are being asked about (Brown, 2001). It is clear that more than one aspect of Dissociative Identity Disorder needs to be considered when concluding how the personalities interact. They may very well be aware of each other and have a system that allows for relatively viable sharing of the body. Other cases, however, may pose more trouble wherein the personalities are unaware of each other and may show even malicious behaviors while not in control. An in-depth look at each case would provide the most accurate results as to how the personalities interact.
Peer Commentary The Therapist's Role in Multiple Personality Disorder Charles M. Spuckler Rochester Institute of Technology In "Multiple Personality Disorder: Fact or Fiction?" Cherry stated that the patient can appear to have Multiple Personality Disorder in order to gain attention. The therapist could also induce Multiple Personality Disorder in the patient while neglecting other disorders. There have been many reports of therapists who made the Multiple Personality Disorder appear in a patient or made it worse. Such cases help to question the existence of Multiple Personality Disorder, given that it appears to be a reaction to the way a therapists treats it. The therapist can, however, use treatments for Multiple Personality Disorder that will help the patient recover when other techniques will not work. Multiple Personality Disorder may exist, but it is affected greatly by the actions of the therapist. One case study helps to emphasize the role of the therapist inducing Multiple Personality Disorder. The patient in this study had some symptoms that would suggest Multiple Personality Disorder. These symptoms included amnesia. The therapist who treated the patient heard this symptom and attempted to call out a multiple personality in the patient. This was done through hypnosis and calling the name of the other personality, which was given by the therapist. The patient developed the additional personality because of the therapist's actions. The therapist's eagerness to observe Multiple Personality Disorder caused it to surface, and the therapist ignored completely the problems that the patient actually had. Treating the patient's actual problems could have prevented any dissociative disorder (Chitalkar & Pande, 1996). Hypnotism is a common way of creating Multiple Personality Disorders. According to therapists who use it, hypnotism provides a method for allowing different personalities to appear. It has been shown, however, that patients treated by hypnotism are more likely to have certain symptoms and personalities. Hypnotized patients are also more likely to report abuse, which fits most therapists' vision of the cause of Multiple Personality Disorder (Rowell & Gee, 1999). Both of the above reports show that it is possible for therapists to greatly affect the patient. The patients in the studies may have had some symptoms similar to Multiple Personality Disorder, but their behavior appeared to have been affected by the therapists. The therapists had an idea of how Multiple Personality Order functions and got the patient to act in a manner that agreed with their beliefs. This may weaken the case for Multiple Personality Disorder existing, because the therapist controls to a large extent the patient's actions. It should also be noted that the most common cause of Multiple Personality Disorder is childhood abuse. An abused child will dissociate the painful memories and repress feeling of trauma. Often these memories of childhood abuse are only revealed through a recovery process with a therapist. Such recovered memories are often false and come from the therapists urging that abuse had taken place. Patients may feel that they need to conform to the therapist's opinions. Again, this shows that the therapist is changing the way the patient thinks in order to fit the most likely path of Multiple Personality Disorder. The therapist can worsen Multiple Personality Disorder but also must recognize that it exists how it can be treated. It has been reported that therapists who do not believe in Multiple Personality Disorder will seek to get the patient to repress all signs of it. This treatment may reduce outward signs of the disorder, but the disorder remains and could actually become worse due to the treatment. The major goal of many treatments for Multiple Personality Disorder is to work through the underlying issue thought to have caused the disorder (Kluft, 1999). The therapist is in a difficult position when dealing with patients with Multiple Personality Disorder. Therapists must not encourage the preexisting disorder to agrees with their own ideas about the disorder, but therapists also must not ignore the disorder completely. Therapists could be better educated about Multiple Personality Disorder and how likely it is for a patient to change his or her behavior to meet the expectations of the therapist.
Peer Commentary Heads I Win, Tails You Lose: Are Multiple Personality and Dissociative Identity Disorder Really Different? Erin M. Wells Rochester Institute of Technology Multiple Personality Disorder (MPD) seems to be a very popular and heated topic of debate. It is interesting to think about what it would be like to have different people emerge from one's self and not even recollect what happened while the alter was present. Another possible source of intrigue that may have aided in the popularity of MPD may be its relatedness to demonic episodes and the seeming ability to "just get away from it all," as I'm sure many have wanted to do. The existence of Multiple Personality Disorder as an actual diagnosable and treatable disorder was the topic of Alex Cherry's paper, and I am wondering if it is actually "fiction" or if the criticizers are claiming its nonexistence just because they can't support or explain the symptoms either way. It is really interesting that Dissociative Identity Disorder (DID) seems much more professionally accepted, enough to be published as a mental disorder. DID even has scales of measure that make it diagnosable, and my question is what really is the difference between a person with MPD and one diagnosed with DID? It seems like a very gray area, where somehow professionals have accepted one and hotly contest the other. Both disorders are thought to be caused by severe trauma and both have symptoms of alterations in consciousness, memory, and identity. Many sources even refer to them as the same disorder simply with a different name. Perhaps it is my severe lack of knowledge in the subject matter, but does it all not seem like semantics? Is DID not getting as much criticism as MPD because with the term "multiple personality" in the title, the disorder seems more outlandish and far-fetched? It just seems disconnected that MPD is contested as being an actual disorder whereas DID appears to be the same thing with a little more political correctness and qualitative support. I do not contest the skepticism that clinicians can be very suggestive about the manifestation of a client's mental disorder or state. It seems very likely that a highly suggestive person can be manipulated to believe that something happened to them and that the need to deal with it, especially if the client is under some form of hypnosis. Also, the social popularity and media images of the disorder do seem to play a role in the numbers of occurrences and the manner in which the alters diverge. Does the social element of the disorder mean that it's simply made up and should not even be diagnosed? Could it be that individuals that tend to get dissociative disorders like DID are already susceptible to suggestion and the world around them? Perhaps the changing nature of MPD or DID is due to social changes and how they affect the individual with the disorder. Might it be that the reason the number of alters has risen dramatically since the 19th century be due to a more open nature of society itself and the greater acceptance of psychological disorders in general? I do not doubt that there are individuals out there who are truly feigning the disorder or have incorrectly been diagnosed, but maybe some of the criticism can be relieved from MPD or DID if the manifestations of the disorder are allowed to ebb and flow with the attitudes of society. It would be interesting to study the prevalence and ways in which dissociative disorder exhibits cross-culturally. This paper stated that MPD was suggested as not being cross-cultural, and it would be relevant to note if those not being treated professionally for dissociative disorders had different intensities of the MPD versus those receiving therapy. I guess the real question is whether Multiple Personality Disorder and Dissociative Identity Disorder are really just different names for the same thing? This is a really hard area to study, because the disorders are relatively uncharacterized and are mostly objective in the diagnosis. Moreover, because society and its effects on any individual are not going away, its influence on suggestive disorders like these must be taken into account. Normal personality is somewhat influenced by environment, so naturally multiple identities within one person (whether internal or external) are also going to be impressed upon by the world around them.
Author Response Fictions of Dissociative Identity Disorder Alexandria K. Cherry Rochester Institute of Technology There have always been many misconceptions regarding the differences between Multiple Personality Disorder (MPD) and Dissociative Identity Disorder (DID). This does not discount the critics of my paper, "Multiple Personality Disorder: Fact or Fiction?" Several arguments criticized the arguments in my paper. These are all without strong foundations and therefore cannot hold up. The first commentary, "Multiple Personality Disorder and Dissociative Identity Disorder Are One and the Same," by Clopper mades its mistake in the second paragraph. Clopper stated that she did not agree with the conclusion that reclassifying MPD as DID is good and then contradicts this statement in the next sentence by saying she felt that it solves many problems to reclassify the disorder. This argument does not hold up if it makes sense at all. "Dissociative Identity Disorder: With Whom Am I Speaking?" by Silverman , presented a very interesting twist on the topic discussed in my paper. "The Therapist's Role in Multiple Personality Disorder," by Spuckler , also provided an interesting spin on the topic; he explored the many roles the therapist plays in the disorder. The last commentary, "Heads I Win, Tails You Lose: Are Multiple Personality and Dissociative Identity Disorder Really Different?" provided a very interesting, for lack of a better word, complaint. Though Wells admited to having little knowledge in the topic, she emphasized what many people, professionals and non-professionals alike, have been wondering. There are subtle changes, and the reclassification is important if for only the reason that MPD became distorted over time.
References Brown, M. T. (2001). Multiple personality and personal identity. Philosophical Psychology, 14, 435-448. Carter, R. (2003). Fractured minds. New Scientist, 179, 36-40. Chitalkar, Y., & Pande, N. (1996). Collusion and entanglement in the therapy of a patient with multiple personalities. American Journal of Psychotherapy, 50, 243-252. Cormier, J. F., & Thelen M. H. (1998). Professional skepticism of multiple personality disorder. Professional Psychology: Research and Practice, 29, 163-167. Dunn, G. E. (1992). Multiple personality disorder: A new challenge for psychology. Professional Psychology: Research and Practice, 23, 18-23. Gleaves, D. H., Hernandez, E., & Warner, M. S. (1999). Corroborating premorbid dissociative symptomatology in dissociative identity disorder. Professional Psychology: Research and Practice, 30, 341-345. Gleaves, D. H., Hernandez, E., & Warner, M. S. (2003). The etiology of dissociative identity disorder: Reply to Gee, Allen, and Powell (2003). Professional Psychology: Research and Practice, 34, 116-118. Hayes, J. A., & Mitchell, J. C. (1994). Mental health professionals' skepticism about multiple personality disorder. Professional Psychology: Research and Practice, 25, 410-415. Kennett, J., & Matthews, S. (2002). Identity, control and responsibility: The case of Dissociative Identity Disorder. Philosophical Psychology, 15, 509-527. Kihlstrom, J. F., Glisky, M. L., & Angiulo, M. J. (1994). Dissociative tendencies and dissociative disorders. Journal of Abnormal Psychology, 103, 117-124. Kluft, R. P. (1999). An overview of the psychotherapy of dissociative identity disorder. American Journal of Psychotherapy, 53, 289-320. Larsen, R. J., & Buss, D. M. (2005). Personality psychology: Domains of knowledge about human nature (2nd ed.). Boston: McGraw-Hill. Lilienfeld, S. O., Lynn, S. J., Kirsch, I., Chaves, J. F., Sarbin, T. R., Ganaway, G. K., & Powell, R. A. (1999). Dissociative identity disorder and the sociocognitive model: Recalling the lessons of the past. Psychological Bulletin, 125, 507-523. Pica, M. (1999). The evolution of alter personality states in dissociative identity disorder. Psychotherapy: Theory, Research, Practice, Training, 36, 404-415. Putman, F. W., Zahn, T. P., & Post, R. M. (1990). Differential autonomic nervous system activity in multiple personality disorder. Psychiatry Research, 31, 251-260. Raulin, M. L., Lilienfeld, S. O., & Katkin, E. S. (2003). Abnormal psychology. Boston: Allyn & Bacon. Rowell, R. A., & Gee, T. L. (1999). The effects of hypnosis on dissociative identity disorder: A reexamination of the evidence. Canadian Journal of Psychiatry, 44, 914-917. Spanos, N. P. (1994). Multiple identity enactments and multiple personality disorder: A sociocognitive perspective. Psychological Bulletin, 116, 143-165. Spiegel, D., & Cardeña, E. (1991). Disintegrated experience: The dissociative disorders revisited. Journal of Abnormal Psychology, 100, 366-378. Waller, N. G., Putnam, F. W., Carlson, E. B. (1996). Types of dissociation and dissociative types: A taxometric analysis of dissociative experiences. Psychological Methods, 1, 300-321. Watson, D. (2003). Investigating the construct validity of the dissociative taxon: Stability analyses of normal and pathological dissociation. Journal of Abnormal Psychology, 112, 298-305.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.11(2); 2023 Apr
- PMC10183298

Partial dissociative identity disorder and gender incongruence: a case report
Roland hasler.
Department of Psychiatry, Faculty of Medicine, University of Geneva, Geneva 1201, Switzerland
TRE Unit, Division of Psychiatric Specialities, Department of Psychiatry, University Hospital of Geneva, Geneva 1201, Switzerland
Jérôme Pache
Sexual Medicine and Sexology Unit, Division of Psychiatric Specialities, Department of Psychiatry, University Hospital of Geneva, Geneva 1201, Switzerland
John Köhl
Lorenzo soldati, introduction.
Gender incongruence (GI) is characterized by a marked and persistent incongruence between an individual’s experienced gender and assigned sex, which often leads to a desire to “transition” and a demand for medical treatments. Dissociative identity disorder and partial dissociative identity disorder (PDID) are poorly known mental disorders whose clinical presentation can be confused with GI.
To provide a case report of a patient with PDID and GI who required treatment for GI.
A case report and follow-up were described.
The case report describes a person suffering from PDID and GI and asked for hormonal treatment for GI. In view of the complexity of the case, it was decided to start a follow-up to investigate the gender experience of the different personalities. After 4 months of follow-up, the symptomatology changed, and the patient waived treatment for GI and continued psychotherapeutic treatment for PDID.
Our case report shows the complexity of providing treatment for patient with PDID and GI.
Gender incongruence (GI) is characterized by a marked and persistent incongruence between an individual’s experienced gender and the assigned sex. This often leads to a desire to “transition” to live and be accepted as a person of the experienced gender through gender-affirming hormonal treatment, gender-affirming surgery, or other health care services to make the individual’s body align—as much as desired and to the extent possible—with the experienced gender. 1 GI prevalence is estimated at 0.02% to 0.1%. 2 The goal of gender-affirming hormonal treatment is to induce changes in secondary sexual characteristics, generally by using estrogen with an androgen-lowering medication or testosterone. Gender-affirming surgery refers to different procedures designed to align a person’s body with one’s gender identity, such as vaginoplasty, phalloplasty breast surgery, and facial surgery. These treatments decrease GI and improve quality of life. 2
The World Professional Association for Transgender Health’s standards of care indicate that before one starts gender-affirming medical and/or surgical treatment (GAMST), mental health conditions that may explain the apparent GI must be identified and excluded. 2 Some authors emphasize the importance of considering dissociative disorders when making a differential diagnosis of GI, particularly dissociative identity disorder (DID). 3
DID is characterized by disruption of identity in which there are ≥2 distinct personality states associated with marked discontinuities in the sense of self and agency. Each personality state includes its own pattern of experiencing, perceiving, conceiving, and relating to self, the body, and the environment. At least 2 distinct personality states recurrently take executive control of the individual’s consciousness and functioning in interacting with others or with the environment. There are typically episodes of amnesia. 4 Unlike DID, in partial DID (PDID), there are no episodes of amnesia, and generally 1 personality state is dominant and normally functions in daily life but is intruded on by ≥1 nondominant personality states. The nondominant personality states do not recurrently take executive control of the individual’s consciousness and functioning, but there may be occasional and limited episodes in which a distinct personality state assumes executive control. 4 DID prevalence is estimated to be 1% to 3%, and there are no prevalence estimations for PDID. 5 Psychotherapy is the treatment of choice for these syndromes. 5
Our case report describes the assessment and management of a patient with PDID and GI who asked for GAMST. The goal of this article is to inform clinicians working with patients who ask for GAMST of the possible existence of a rare case of DID or PDID and to inform them of the complexity of providing treatment for these patients.
Case report
A 25-year-old healthy single man referred himself to the Sexology Unit for GI with a request for feminizing hormone therapy (FHT). The patient provided written informed consent. He described suffering for 5 months from an identity disturbance characterized by several distinct personalities, with different gender identities (3 males and 4 females) without memory gaps. He explained that 1 of the female personalities, 1 month after discovering his dissociative disorder, could not tolerate the male body, in which she felt incongruent with her female gender identity and wished to undertake FHT to feminize it.
The Dissociative Experience Scale 6 showed a score of 43.21 in December 2021. At the end of the assessment, 2 concurrent diagnoses were retained: PDID and GI. The diagnosis of PDID was retained since the patient described symptoms consistent with DID. However, the diagnosis of DID could not be retained because of the absence of memory gaps. The diagnosis of GI was retained since 1 of the female personalities described symptoms typical of GI.
In view of the complexity of the case, it was decided to start a 6-month psychotherapeutic treatment. In the beginning, treatment focused on offering support and giving information about the effects and potential side effects of GAMST. This was followed by an exploration and a clarification of the experience that the different personalities had of the male body and how they imagined their body experience after the GAMST. Finally, there was an exploration of the function of the personality-splitting mechanism and the possibility that forgotten traumatic events had generated it.
At about 4 months of treatment, the different personalities seemed to have agreed on the project of feminizing the body. Even the male personalities had come to the conclusion that FHT would have brought an overall well-being to all personalities. The therapist also considered proposing FHT following the 6 months of treatment.
But after 4 months of psychotherapy, the patient began to have a vague memory of having been sexually abused as a child. This awareness, despite being vague, had a major impact on the symptomatology and led to a decrease in the intensity of the dissociative symptoms. In July 2022, the Dissociative Experience Scale score was 34.28. In addition, the GI disappeared. The patient gave up his project for FHT, realizing that the feminization of the body could not bring him well-being, as the male personalities would have experienced this negatively. Moreover, he was no longer willing to accept the health risks of FHT and the social difficulties that he might have experienced in making a social transition.
This case report shows the complexity of a mental health assessment following a request for GAMST in patients with PDID or DID.
The scientific literature on this subject is poor; the few articles are usually case reports. 3 A few articles show a prevalence of DID in GI cases ranging from 0% to 1.5%: a rate that is not significantly higher than that of the standard population, which is 1% to 3%. 3 Other case reports highlight 2 problems: the difficulty of making a differential diagnosis between GI and DID and the difficulty of treating people with GI and DID at the same time. 3
Our case can be understood to be at the border of these 2 problems, since the 2 syndromes had coexisted for approximately 12 months. After 6 months of psychotherapy, the decrease of the dissociative symptomatology led to the disappearance of the GI. We therefore concluded that the apparent GI was part of the PDID symptomatology. Our understanding of the change in symptomatology, which was co-constructed with the patient, was that with the recollection of the memories of the abuse, the amnestic function of the personality splitting was no longer needed. As a consequence, this decrease in the need for personality splitting reduced the presence of the different personalities, including the female ones. This made the GI disappear.
Regarding the difficulty of making a differential diagnosis between GI and DID, there are 2 case reports in the literature in which there was a misdiagnosis. These were patients with DID who requested treatment for GI. The diagnosis of GI was made, and an individual treatment plan for GI and care planning was set up. However, 1 of the 2 patients was hospitalized for a depressive reaction with suicidal ideation, and the other was incarcerated following the murder of a woman. Only after hospitalization and incarceration was the diagnosis of GI changed to DID. The authors hypothesized that the depression and murder were related to the tension among the gendered personalities as a result of the misdiagnosis and proposed treatment for GI. 3 Other case reports describe patients who sought treatment for GI, but the diagnosis of DID was withheld; instead of treatment for GI, psychotherapeutic follow-up for DID was offered, which was beneficial. 3
Concerning the difficulty of treating patients who were concerned with the comorbidity between GI and DID, in 1 case report 7 there was a decrease in GI with gender-affirming hormonal treatment; in another 8 the emergence of GI in the other personalities was described following gender-affirming surgery. In the other case reports, tension remained among the personalities of different genders regarding the gender-affirming surgery. 3
Furthermore, as stressed by the International Society for the Study of Trauma and Dissociation, 5 it is difficult to diagnose DID because of a lack of information among clinicians about dissociative disorders. When this happens, the undiagnosed patient with DID may undergo a long and frequently unsuccessful treatment for other conditions, such as posttraumatic stress disorder, depression, panic attacks, substance abuse, and eating-disordered symptoms.
Returning to our case report, in light of what we have learned from these articles in the literature, we can wonder about what would have happened if we had given FHT to this patient without psychotherapeutic treatment. We can speculate that at a certain time, the patient would have eventually had memories of the sexual abuse that led to the disappearance of his GI and asked to stop the FHT. However, we can speculate that experiencing FHT might have reinforced his feeling that it was the right option for him. This could have increased the tension among the different personalities with negative consequences for his mental health. The other personalities could have also developed GI.
Regarding the difficulties in making the differential diagnosis between GI and DID, some authors have stressed that patients with DID may frequently experience bewilderment or confusion in their gender identity and in body sex characteristics. They suggest, however, that these patients describe a global identity disturbance, unlike patients with GI, who focus more on the GI. 9 Further difficulty in the assessment of DID in patients asking for treatments for GI is that GI is usually a self-diagnosis and DID is frequently a delayed diagnosis. Patients with DID frequently hide their symptoms; therefore, these symptoms must actively be looked for. 10
Regarding the appropriateness of offering GAMST to patients with diagnoses of GI and DID, some authors stress that it is highly questionable that these patients should receive GAMST until the DID has been treated. They stress the importance, in the sessions prior to GAMST, of providing psychotherapy for the dissociative symptoms.
Other authors propose that, while not requiring integration of the alter personality before GAMST, at the very least there should be informed consent or a consensus of all the known alter personalities. 11
In our case report, where the patient was diagnosed with PDID, the issue of consent was not as problematic because, in the absence of memory gaps, the different personalities were present or activated at any time. In cases of PDID, with major splits among the different personalities, as well as memory gaps about the behaviors and thoughts of the other personalities, the issue of consent to treatment is more complex. We therefore advise offering psychotherapy to understand the experience of the different personalities in relation to the body and their views on GI care before offering GI treatment.
Mental health providers working with patients with GI should be informed that some patients seeking treatment for GI may have DID or PDID, and they should be aware of the possible comorbidity between the diagnoses. They also need to be aware of the complexity of treating these patients in terms of consent and the iatrogenic effects that GI treatments may have.
One should keep in mind that patients asking for GAMST while experiencing DID or PDID are quite rare, so systematic screening of this syndrome in all patients who have GI is not suitable, in line with the guidelines of the World Professional Association for Transgender Health. 2 However, in the presence of any type of dissociative symptoms, it is essential to assess the possible presence of DID or PDID when in contact with patients describing multiple personalities. If this is confirmed, it is advisable to propose an exploratory psychotherapeutic treatment to clarify the body experience of the different personalities as well as their consent to GI treatments.
None declared.
Conflicts of interest: None declared.
Contributor Information
Roland Hasler, Department of Psychiatry, Faculty of Medicine, University of Geneva, Geneva 1201, Switzerland. TRE Unit, Division of Psychiatric Specialities, Department of Psychiatry, University Hospital of Geneva, Geneva 1201, Switzerland.
Jérôme Pache, Sexual Medicine and Sexology Unit, Division of Psychiatric Specialities, Department of Psychiatry, University Hospital of Geneva, Geneva 1201, Switzerland.
John Köhl, Sexual Medicine and Sexology Unit, Division of Psychiatric Specialities, Department of Psychiatry, University Hospital of Geneva, Geneva 1201, Switzerland.
Lorenzo Soldati, Sexual Medicine and Sexology Unit, Division of Psychiatric Specialities, Department of Psychiatry, University Hospital of Geneva, Geneva 1201, Switzerland.

IMAGES
VIDEO
COMMENTS
Dissociative identity disorder (DID), commonly known as multiple personality disorder (MPD), is a contentious mental health condition that typically arises as a result of traumatic events to help people avoid unpleasant memories. ... the research intended to maintain methodological transparency and robustness, helping to provide an accurate and ...
Multiple personality disorder is a mental disorder characterized by the maintenance of at least. two distinct and relatively enduring personality states. Multiple personality disorder is lack of ...
Dissociative identity disorder (DID), previously referred to as multiple personality disorder (MPD), is often discounted, neglected, and misunderstood by the health care system and society.
Dissociative identity disorder (DID) is a rare disorder associated with severe behavioral health symptoms. DID was previously known as Multiple Personality Disorder until 1994. Approximately 1.5% of the population internationally has been diagnosed with dissociative identity disorder.[1] Patients with this diagnosis often have several emergency presentations, often with self-injurious behavior ...
Introduction. Dissociative identity disorder (DID), or dissociative personality disorder, is the presence of at least two varied personalities in one person [1-2].Thus, it is also referred to as multiple personality disorder [].There are several conditions found to be associated with this disorder, including depression, self-harm, post-traumatic stress disorder (PTSD), substance use disorder ...
Dissociative Identity Disorder (DID) is a complex and controversial diagnosis that has undergone multiple revisions in the Diagnostic and Statistical Manual of Mental Disorders (DSM) since its recognition in the 1950s (North, 2015). There is not a clear understanding of DID etiopathology, there is no standardized method of diagnosis, and as ...
Introduction. Multiple Personality Disorder (MPD) was first introduced in DSM-III in 1980 and re-named Dissociative Identity Disorder (DID) in subsequent editions of the diagnostic manual (American Psychiatric Association, 2013).Table 1 shows diagnostic criteria of this disorder in ICD-10, ICD-11, and DSM-5. Some healthcare providers perceive it as fairly uncommon or associated with temporary ...
Background Despite effective treatments for personality disorders being developed, consumers and carers often report negative experiences of mental health services, including challenges accessing these treatments. Methods This qualitative study used separate focus groups to compare the unique perspectives of consumer and carers, and to investigate how to improve services for individuals with ...
of behavior. Antisocial. Disregard for, and violation of, the rights of others. Borderline. Instability in interpersonal relationships, self-image, and affects and marked impulsivity. Histrionic ...
The contemporary diagnostic criteria for multiple personality disorder are vague and overinclusive, there is little literature support for the theory that MPD results from childhood trauma, and many of the techniques used to diagnose and treat the condition reinforce its symptoms. Five aspects of the diagnosis and treatment of multiple personality disorder (MPD) were examined.
Few psychological disorders in the Diagnostic Statistical Manual have generated. as much controversy as Dissociative Identity Disorder (DID). For the past 35 years. diagnoses of DID, previously referred to as Multiple Personality Disorder (MPD), have. increased exponentially, causing various psychological researchers and clinicians to.
Personality disorders are highly prevalent in clinical practice. With the introduction of the Diagnostic Statistical Manual - 5th Edition (DSM-5) the multi-axial system of diagnosis for mental disorders has disappeared, which has led to an increase in research on personality disorders (e.g. Emmelkamp & Meyerbröker, 2020).In this Special Issues, several recent developments are discussed.
Personality disorders (PDs) can be described as the manifestation of extreme personality traits that interfere with everyday life and contribute to significant suffering, functional limitations, or both. They are common and are frequently encountered in virtually all forms of health care. PDs are associated with an inferior quality of life (QoL ...
Although the disorder has its roots in childhood, most patients are not diagnosed with this condition until 20 to 50 years of age, many have received several prior, erroneous diagnoses of mental or physical disorders or both. Multiple personality disorder is understood today as chronic dissociative psychopathology that most often develops in response to severe abuse in childhood. The ...
This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development. Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).
### What you need to know ### Sources and selection criteria We searched Pubmed, Medline, Embase, the Cochrane Library, CINAHL, PsycINFO, AMED, British Nursing Index, HMIC, and Health Business Elite using the term "personality disorder". Findings from randomised controlled trials (RCTs), systematic reviews, and meta-analyses were ranked as high in quality (see table 1) and we also used our ...
A new paper argues the condition now known as "dissociative identity disorder" might help us understand the fundamental nature of reality
A Controversial Diagnosis. In 1988, Dell 1 surveyed clinicians to assess the reactions they had encountered from others as a result of their interest in dissociative identity disorder (DID), previously called multiple personality disorder. Of 62 respondents who had treated patients with DID, more than 80 percent said they had experienced "moderate to extreme" reactions from colleagues ...
Personality Development. Psychiatric Status Rating Scales. The last decade has seen the emergence of solid research on MPD and the dissociative disorders, particularly in the area of diagnosis and clinical phenomenology. A number of other areas have been opened up or advanced considerably. The most notable of these include child and adolescent ...
Keywords: mpd, did, dissociative identity disorder management, dissociative identity disorder, multiple personality disorder Introduction And Background One sign of a personality disorder is an inflexible and destructive thought pattern. Personality disorders are more prevalent in clinical patients compared to the general population [1].
Personality disorders form a class of mental disorders that are characterized. by long-lasting rigid patterns of thought and behaviour which cause serious. problems with relationships and work ...
Alexandria K. Cherry Rochester Institute of Technology. Multiple Personality Disorder, or MPD, is one of the most talked about and publicized disorders known and is the center of much debate and criticism. What is currently known about MPD has become common place over the past 20 years. The past two decades have shown an increase in the number ...
Using case formulation for prediction of the therapeutic alliance in treatment for borderline personality disorder. Pers Disord. 2022. 10.1037/per0000555. A statistical demonstration of the use of cross-lagged methodology in the context of the impact of case formulation on the alliance process in treatments for borderline personality disorder.
Introduction. Gender incongruence (GI) is characterized by a marked and persistent incongruence between an individual's experienced gender and assigned sex, which often leads to a desire to "transition" and a demand for medical treatments. Dissociative identity disorder and partial dissociative identity disorder (PDID) are poorly known ...