BRIEF RESEARCH REPORT article
How do critical thinking ability and critical thinking disposition relate to the mental health of university students.

- School of Education, Huazhong University of Science and Technology, Wuhan, China
Theories of psychotherapy suggest that human mental problems associate with deficiencies in critical thinking. However, it currently remains unclear whether both critical thinking skill and critical thinking disposition relate to individual differences in mental health. This study explored whether and how the critical thinking ability and critical thinking disposition of university students associate with individual differences in mental health in considering impulsivity that has been revealed to be closely related to both critical thinking and mental health. Regression and structural equation modeling analyses based on a Chinese university student sample ( N = 314, 198 females, M age = 18.65) revealed that critical thinking skill and disposition explained a unique variance of mental health after controlling for impulsivity. Furthermore, the relationship between critical thinking and mental health was mediated by motor impulsivity (acting on the spur of the moment) and non-planning impulsivity (making decisions without careful forethought). These findings provide a preliminary account of how human critical thinking associate with mental health. Practically, developing mental health promotion programs for university students is suggested to pay special attention to cultivating their critical thinking dispositions and enhancing their control over impulsive behavior.

Introduction
Although there is no consistent definition of critical thinking (CT), it is usually described as “purposeful, self-regulatory judgment that results in interpretation, analysis, evaluation, and inference, as well as explanations of the evidential, conceptual, methodological, criteriological, or contextual considerations that judgment is based upon” ( Facione, 1990 , p. 2). This suggests that CT is a combination of skills and dispositions. The skill aspect mainly refers to higher-order cognitive skills such as inference, analysis, and evaluation, while the disposition aspect represents one's consistent motivation and willingness to use CT skills ( Dwyer, 2017 ). An increasing number of studies have indicated that CT plays crucial roles in the activities of university students such as their academic performance (e.g., Ghanizadeh, 2017 ; Ren et al., 2020 ), professional work (e.g., Barry et al., 2020 ), and even the ability to cope with life events (e.g., Butler et al., 2017 ). An area that has received less attention is how critical thinking relates to impulsivity and mental health. This study aimed to clarify the relationship between CT (which included both CT skill and CT disposition), impulsivity, and mental health among university students.
Relationship Between Critical Thinking and Mental Health
Associating critical thinking with mental health is not without reason, since theories of psychotherapy have long stressed a linkage between mental problems and dysfunctional thinking ( Gilbert, 2003 ; Gambrill, 2005 ; Cuijpers, 2019 ). Proponents of cognitive behavioral therapy suggest that the interpretation by people of a situation affects their emotional, behavioral, and physiological reactions. Those with mental problems are inclined to bias or heuristic thinking and are more likely to misinterpret neutral or even positive situations ( Hollon and Beck, 2013 ). Therefore, a main goal of cognitive behavioral therapy is to overcome biased thinking and change maladaptive beliefs via cognitive modification skills such as objective understanding of one's cognitive distortions, analyzing evidence for and against one's automatic thinking, or testing the effect of an alternative way of thinking. Achieving these therapeutic goals requires the involvement of critical thinking, such as the willingness and ability to critically analyze one's thoughts and evaluate evidence and arguments independently of one's prior beliefs. In addition to theoretical underpinnings, characteristics of university students also suggest a relationship between CT and mental health. University students are a risky population in terms of mental health. They face many normative transitions (e.g., social and romantic relationships, important exams, financial pressures), which are stressful ( Duffy et al., 2019 ). In particular, the risk increases when students experience academic failure ( Lee et al., 2008 ; Mamun et al., 2021 ). Hong et al. (2010) found that the stress in Chinese college students was primarily related to academic, personal, and negative life events. However, university students are also a population with many resources to work on. Critical thinking can be considered one of the important resources that students are able to use ( Stupple et al., 2017 ). Both CT skills and CT disposition are valuable qualities for college students to possess ( Facione, 1990 ). There is evidence showing that students with a higher level of CT are more successful in terms of academic performance ( Ghanizadeh, 2017 ; Ren et al., 2020 ), and that they are better at coping with stressful events ( Butler et al., 2017 ). This suggests that that students with higher CT are less likely to suffer from mental problems.
Empirical research has reported an association between CT and mental health among college students ( Suliman and Halabi, 2007 ; Kargar et al., 2013 ; Yoshinori and Marcus, 2013 ; Chen and Hwang, 2020 ; Ugwuozor et al., 2021 ). Most of these studies focused on the relationship between CT disposition and mental health. For example, Suliman and Halabi (2007) reported that the CT disposition of nursing students was positively correlated with their self-esteem, but was negatively correlated with their state anxiety. There is also a research study demonstrating that CT disposition influenced the intensity of worry in college students either by increasing their responsibility to continue thinking or by enhancing the detached awareness of negative thoughts ( Yoshinori and Marcus, 2013 ). Regarding the relationship between CT ability and mental health, although there has been no direct evidence, there were educational programs examining the effect of teaching CT skills on the mental health of adolescents ( Kargar et al., 2013 ). The results showed that teaching CT skills decreased somatic symptoms, anxiety, depression, and insomnia in adolescents. Another recent CT skill intervention also found a significant reduction in mental stress among university students, suggesting an association between CT skills and mental health ( Ugwuozor et al., 2021 ).
The above research provides preliminary evidence in favor of the relationship between CT and mental health, in line with theories of CT and psychotherapy. However, previous studies have focused solely on the disposition aspect of CT, and its link with mental health. The ability aspect of CT has been largely overlooked in examining its relationship with mental health. Moreover, although the link between CT and mental health has been reported, it remains unknown how CT (including skill and disposition) is associated with mental health.
Impulsivity as a Potential Mediator Between Critical Thinking and Mental Health
One important factor suggested by previous research in accounting for the relationship between CT and mental health is impulsivity. Impulsivity is recognized as a pattern of action without regard to consequences. Patton et al. (1995) proposed that impulsivity is a multi-faceted construct that consists of three behavioral factors, namely, non-planning impulsiveness, referring to making a decision without careful forethought; motor impulsiveness, referring to acting on the spur of the moment; and attentional impulsiveness, referring to one's inability to focus on the task at hand. Impulsivity is prominent in clinical problems associated with psychiatric disorders ( Fortgang et al., 2016 ). A number of mental problems are associated with increased impulsivity that is likely to aggravate clinical illnesses ( Leclair et al., 2020 ). Moreover, a lack of CT is correlated with poor impulse control ( Franco et al., 2017 ). Applications of CT may reduce impulsive behaviors caused by heuristic and biased thinking when one makes a decision ( West et al., 2008 ). For example, Gregory (1991) suggested that CT skills enhance the ability of children to anticipate the health or safety consequences of a decision. Given this, those with high levels of CT are expected to take a rigorous attitude about the consequences of actions and are less likely to engage in impulsive behaviors, which may place them at a low risk of suffering mental problems. To the knowledge of the authors, no study has empirically tested whether impulsivity accounts for the relationship between CT and mental health.
This study examined whether CT skill and disposition are related to the mental health of university students; and if yes, how the relationship works. First, we examined the simultaneous effects of CT ability and CT disposition on mental health. Second, we further tested whether impulsivity mediated the effects of CT on mental health. To achieve the goals, we collected data on CT ability, CT disposition, mental health, and impulsivity from a sample of university students. The results are expected to shed light on the mechanism of the association between CT and mental health.
Participants and Procedure
A total of 314 university students (116 men) with an average age of 18.65 years ( SD = 0.67) participated in this study. They were recruited by advertisements from a local university in central China and majoring in statistics and mathematical finance. The study protocol was approved by the Human Subjects Review Committee of the Huazhong University of Science and Technology. Each participant signed a written informed consent describing the study purpose, procedure, and right of free. All the measures were administered in a computer room. The participants were tested in groups of 20–30 by two research assistants. The researchers and research assistants had no formal connections with the participants. The testing included two sections with an interval of 10 min, so that the participants had an opportunity to take a break. In the first section, the participants completed the syllogistic reasoning problems with belief bias (SRPBB), the Chinese version of the California Critical Thinking Skills Test (CCSTS-CV), and the Chinese Critical Thinking Disposition Inventory (CCTDI), respectively. In the second session, they completed the Barrett Impulsivity Scale (BIS-11), Depression Anxiety Stress Scale-21 (DASS-21), and University Personality Inventory (UPI) in the given order.
Measures of Critical Thinking Ability
The Chinese version of the California Critical Thinking Skills Test was employed to measure CT skills ( Lin, 2018 ). The CCTST is currently the most cited tool for measuring CT skills and includes analysis, assessment, deduction, inductive reasoning, and inference reasoning. The Chinese version included 34 multiple choice items. The dependent variable was the number of correctly answered items. The internal consistency (Cronbach's α) of the CCTST is 0.56 ( Jacobs, 1995 ). The test–retest reliability of CCTST-CV is 0.63 ( p < 0.01) ( Luo and Yang, 2002 ), and correlations between scores of the subscales and the total score are larger than 0.5 ( Lin, 2018 ), supporting the construct validity of the scale. In this study among the university students, the internal consistency (Cronbach's α) of the CCTST-CV was 0.5.
The second critical thinking test employed in this study was adapted from the belief bias paradigm ( Li et al., 2021 ). This task paradigm measures the ability to evaluate evidence and arguments independently of one's prior beliefs ( West et al., 2008 ), which is a strongly emphasized skill in CT literature. The current test included 20 syllogistic reasoning problems in which the logical conclusion was inconsistent with one's prior knowledge (e.g., “Premise 1: All fruits are sweet. Premise 2: Bananas are not sweet. Conclusion: Bananas are not fruits.” valid conclusion). In addition, four non-conflict items were included as the neutral condition in order to avoid a habitual response from the participants. They were instructed to suppose that all the premises are true and to decide whether the conclusion logically follows from the given premises. The measure showed good internal consistency (Cronbach's α = 0.83) in a Chinese sample ( Li et al., 2021 ). In this study, the internal consistency (Cronbach's α) of the SRPBB was 0.94.
Measures of Critical Thinking Disposition
The Chinese Critical Thinking Disposition Inventory was employed to measure CT disposition ( Peng et al., 2004 ). This scale has been developed in line with the conceptual framework of the California critical thinking disposition inventory. We measured five CT dispositions: truth-seeking (one's objectivity with findings even if this requires changing one's preconceived opinions, e.g., a person inclined toward being truth-seeking might disagree with “I believe what I want to believe.”), inquisitiveness (one's intellectual curiosity. e.g., “No matter what the topic, I am eager to know more about it”), analyticity (the tendency to use reasoning and evidence to solve problems, e.g., “It bothers me when people rely on weak arguments to defend good ideas”), systematically (the disposition of being organized and orderly in inquiry, e.g., “I always focus on the question before I attempt to answer it”), and CT self-confidence (the trust one places in one's own reasoning processes, e.g., “I appreciate my ability to think precisely”). Each disposition aspect contained 10 items, which the participants rated on a 6-point Likert-type scale. This measure has shown high internal consistency (overall Cronbach's α = 0.9) ( Peng et al., 2004 ). In this study, the CCTDI scale was assessed at Cronbach's α = 0.89, indicating good reliability.
Measure of Impulsivity
The well-known Barrett Impulsivity Scale ( Patton et al., 1995 ) was employed to assess three facets of impulsivity: non-planning impulsivity (e.g., “I plan tasks carefully”); motor impulsivity (e.g., “I act on the spur of the moment”); attentional impulsivity (e.g., “I concentrate easily”). The scale includes 30 statements, and each statement is rated on a 5-point scale. The subscales of non-planning impulsivity and attentional impulsivity were reversely scored. The BIS-11 has good internal consistency (Cronbach's α = 0.81, Velotti et al., 2016 ). This study showed that the Cronbach's α of the BIS-11 was 0.83.
Measures of Mental Health
The Depression Anxiety Stress Scale-21 was used to assess mental health problems such as depression (e.g., “I feel that life is meaningless”), anxiety (e.g., “I find myself getting agitated”), and stress (e.g., “I find it difficult to relax”). Each dimension included seven items, which the participants were asked to rate on a 4-point scale. The Chinese version of the DASS-21 has displayed a satisfactory factor structure and internal consistency (Cronbach's α = 0.92, Wang et al., 2016 ). In this study, the internal consistency (Cronbach's α) of the DASS-21 was 0.94.
The University Personality Inventory that has been commonly used to screen for mental problems of college students ( Yoshida et al., 1998 ) was also used for measuring mental health. The 56 symptom-items assessed whether an individual has experienced the described symptom during the past year (e.g., “a lack of interest in anything”). The UPI showed good internal consistency (Cronbach's α = 0.92) in a Chinese sample ( Zhang et al., 2015 ). This study showed that the Cronbach's α of the UPI was 0.85.
Statistical Analyses
We first performed analyses to detect outliers. Any observation exceeding three standard deviations from the means was replaced with a value that was three standard deviations. This procedure affected no more than 5‰ of observations. Hierarchical regression analysis was conducted to determine the extent to which facets of critical thinking were related to mental health. In addition, structural equation modeling with Amos 22.0 was performed to assess the latent relationship between CT, impulsivity, and mental health.
Descriptive Statistics and Bivariate Correlations
Table 1 presents descriptive statistics and bivariate correlations of all the variables. CT disposition such as truth-seeking, systematicity, self-confidence, and inquisitiveness was significantly correlated with DASS-21 and UPI, but neither CCTST-CV nor SRPBB was related to DASS-21 and UPI. Subscales of BIS-11 were positively correlated with DASS-21 and UPI, but were negatively associated with CT dispositions.
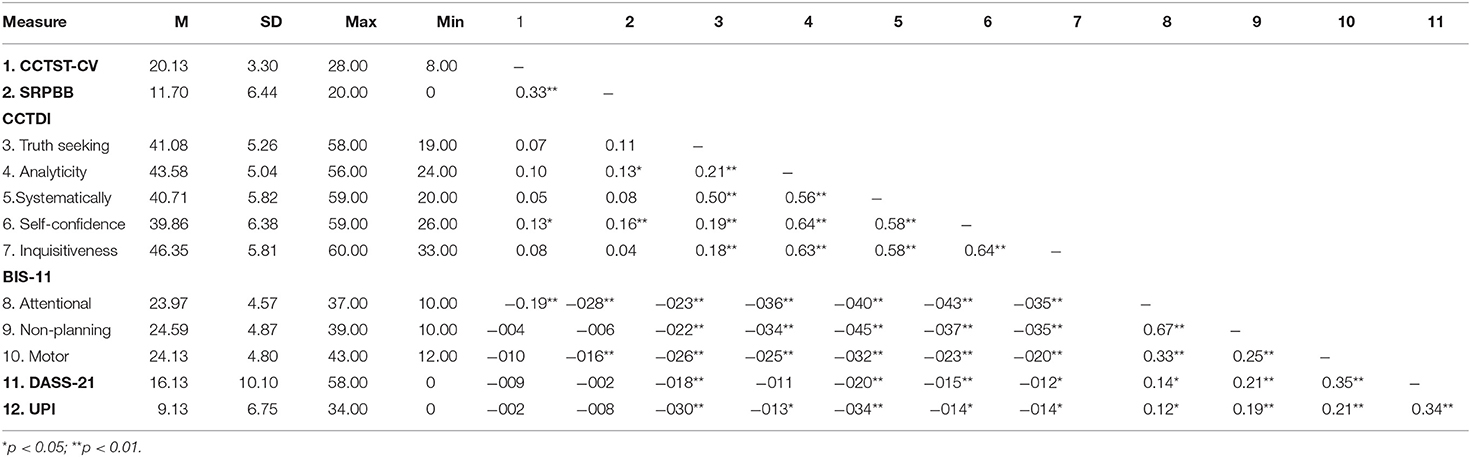
Table 1 . Descriptive results and correlations between all measured variables ( N = 314).
Regression Analyses
Hierarchical regression analyses were conducted to examine the effects of CT skill and disposition on mental health. Before conducting the analyses, scores in DASS-21 and UPI were reversed so that high scores reflected high levels of mental health. Table 2 presents the results of hierarchical regression. In model 1, the sum of the Z-score of DASS-21 and UPI served as the dependent variable. Scores in the CT ability tests and scores in the five dimensions of CCTDI served as predictors. CT skill and disposition explained 13% of the variance in mental health. CT skills did not significantly predict mental health. Two dimensions of dispositions (truth seeking and systematicity) exerted significantly positive effects on mental health. Model 2 examined whether CT predicted mental health after controlling for impulsivity. The model containing only impulsivity scores (see model-2 step 1 in Table 2 ) explained 15% of the variance in mental health. Non-planning impulsivity and motor impulsivity showed significantly negative effects on mental health. The CT variables on the second step explained a significantly unique variance (6%) of CT (see model-2 step 2). This suggests that CT skill and disposition together explained the unique variance in mental health after controlling for impulsivity. 1
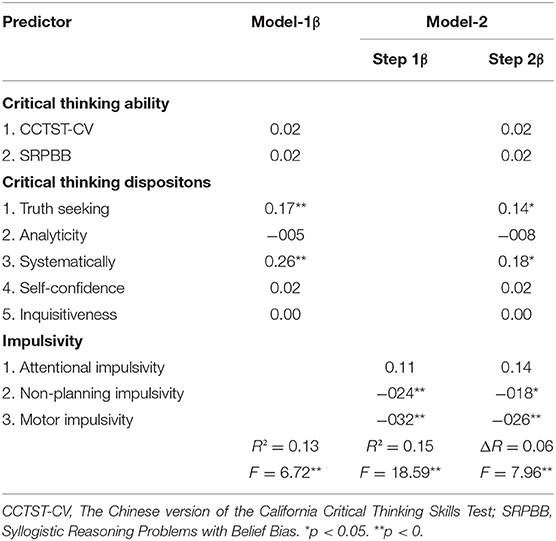
Table 2 . Hierarchical regression models predicting mental health from critical thinking skills, critical thinking dispositions, and impulsivity ( N = 314).
Structural equation modeling was performed to examine whether impulsivity mediated the relationship between CT disposition (CT ability was not included since it did not significantly predict mental health) and mental health. Since the regression results showed that only motor impulsivity and non-planning impulsivity significantly predicted mental health, we examined two mediation models with either motor impulsivity or non-planning impulsivity as the hypothesized mediator. The item scores in the motor impulsivity subscale were randomly divided into two indicators of motor impulsivity, as were the scores in the non-planning subscale. Scores of DASS-21 and UPI served as indicators of mental health and dimensions of CCTDI as indicators of CT disposition. In addition, a bootstrapping procedure with 5,000 resamples was established to test for direct and indirect effects. Amos 22.0 was used for the above analyses.
The mediation model that included motor impulsivity (see Figure 1 ) showed an acceptable fit, χ ( 23 ) 2 = 64.71, RMSEA = 0.076, CFI = 0.96, GFI = 0.96, NNFI = 0.93, SRMR = 0.073. Mediation analyses indicated that the 95% boot confidence intervals of the indirect effect and the direct effect were (0.07, 0.26) and (−0.08, 0.32), respectively. As Hayes (2009) indicates, an effect is significant if zero is not between the lower and upper bounds in the 95% confidence interval. Accordingly, the indirect effect between CT disposition and mental health was significant, while the direct effect was not significant. Thus, motor impulsivity completely mediated the relationship between CT disposition and mental health.
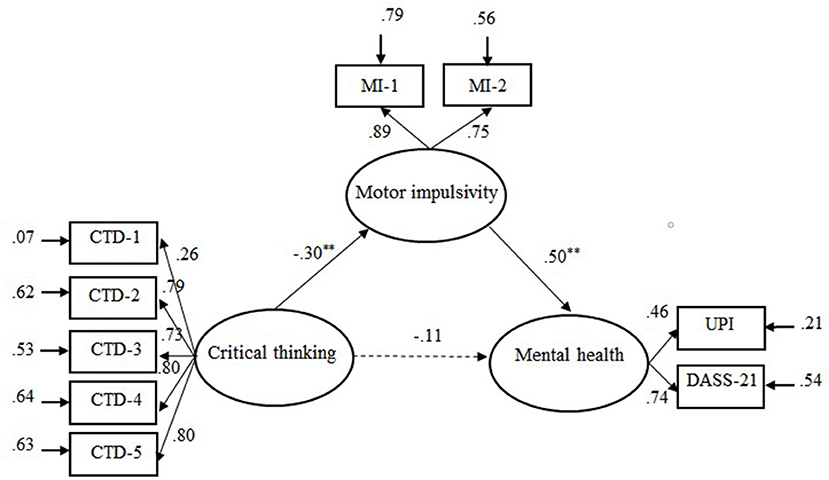
Figure 1 . Illustration of the mediation model: Motor impulsivity as mediator variable between critical thinking dispositions and mental health. CTD-l = Truth seeking; CTD-2 = Analyticity; CTD-3 = Systematically; CTD-4 = Self-confidence; CTD-5 = Inquisitiveness. MI-I and MI-2 were sub-scores of motor impulsivity. Solid line represents significant links and dotted line non-significant links. ** p < 0.01.
The mediation model, which included non-planning impulsivity (see Figure 2 ), also showed an acceptable fit to the data, χ ( 23 ) 2 = 52.75, RMSEA = 0.064, CFI = 0.97, GFI = 0.97, NNFI = 0.95, SRMR = 0.06. The 95% boot confidence intervals of the indirect effect and the direct effect were (0.05, 0.33) and (−0.04, 0.38), respectively, indicating that non-planning impulsivity completely mediated the relationship between CT disposition and mental health.
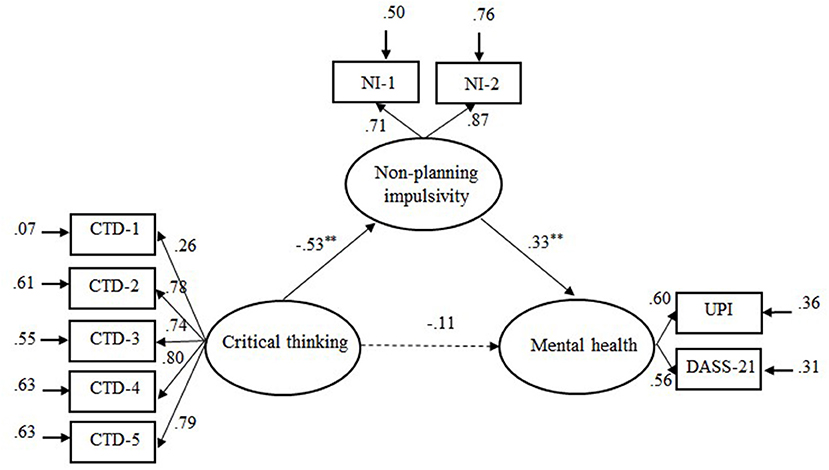
Figure 2 . Illustration of the mediation model: Non-planning impulsivity asmediator variable between critical thinking dispositions and mental health. CTD-l = Truth seeking; CTD-2 = Analyticity; CTD-3 = Systematically; CTD-4 = Self-confidence; CTD-5 = Inquisitiveness. NI-I and NI-2 were sub-scores of Non-planning impulsivity. Solid line represents significant links and dotted line non-significant links. ** p < 0.01.
This study examined how critical thinking skill and disposition are related to mental health. Theories of psychotherapy suggest that human mental problems are in part due to a lack of CT. However, empirical evidence for the hypothesized relationship between CT and mental health is relatively scarce. This study explored whether and how CT ability and disposition are associated with mental health. The results, based on a university student sample, indicated that CT skill and disposition explained a unique variance in mental health. Furthermore, the effect of CT disposition on mental health was mediated by motor impulsivity and non-planning impulsivity. The finding that CT exerted a significant effect on mental health was in accordance with previous studies reporting negative correlations between CT disposition and mental disorders such as anxiety ( Suliman and Halabi, 2007 ). One reason lies in the assumption that CT disposition is usually referred to as personality traits or habits of mind that are a remarkable predictor of mental health (e.g., Benzi et al., 2019 ). This study further found that of the five CT dispositions, only truth-seeking and systematicity were associated with individual differences in mental health. This was not surprising, since the truth-seeking items mainly assess one's inclination to crave for the best knowledge in a given context and to reflect more about additional facts, reasons, or opinions, even if this requires changing one's mind about certain issues. The systematicity items target one's disposition to approach problems in an orderly and focused way. Individuals with high levels of truth-seeking and systematicity are more likely to adopt a comprehensive, reflective, and controlled way of thinking, which is what cognitive therapy aims to achieve by shifting from an automatic mode of processing to a more reflective and controlled mode.
Another important finding was that motor impulsivity and non-planning impulsivity mediated the effect of CT disposition on mental health. The reason may be that people lacking CT have less willingness to enter into a systematically analyzing process or deliberative decision-making process, resulting in more frequently rash behaviors or unplanned actions without regard for consequences ( Billieux et al., 2010 ; Franco et al., 2017 ). Such responses can potentially have tangible negative consequences (e.g., conflict, aggression, addiction) that may lead to social maladjustment that is regarded as a symptom of mental illness. On the contrary, critical thinkers have a sense of deliberativeness and consider alternate consequences before acting, and this thinking-before-acting mode would logically lead to a decrease in impulsivity, which then decreases the likelihood of problematic behaviors and negative moods.
It should be noted that although the raw correlation between attentional impulsivity and mental health was significant, regression analyses with the three dimensions of impulsivity as predictors showed that attentional impulsivity no longer exerted a significant effect on mental effect after controlling for the other impulsivity dimensions. The insignificance of this effect suggests that the significant raw correlation between attentional impulsivity and mental health was due to the variance it shared with the other impulsivity dimensions (especially with the non-planning dimension, which showed a moderately high correlation with attentional impulsivity, r = 0.67).
Some limitations of this study need to be mentioned. First, the sample involved in this study is considered as a limited sample pool, since all the participants are university students enrolled in statistics and mathematical finance, limiting the generalization of the findings. Future studies are recommended to recruit a more representative sample of university students. A study on generalization to a clinical sample is also recommended. Second, as this study was cross-sectional in nature, caution must be taken in interpreting the findings as causal. Further studies using longitudinal, controlled designs are needed to assess the effectiveness of CT intervention on mental health.
In spite of the limitations mentioned above, the findings of this study have some implications for research and practice intervention. The result that CT contributed to individual differences in mental health provides empirical support for the theory of cognitive behavioral therapy, which focuses on changing irrational thoughts. The mediating role of impulsivity between CT and mental health gives a preliminary account of the mechanism of how CT is associated with mental health. Practically, although there is evidence that CT disposition of students improves because of teaching or training interventions (e.g., Profetto-Mcgrath, 2005 ; Sanja and Krstivoje, 2015 ; Chan, 2019 ), the results showing that two CT disposition dimensions, namely, truth-seeking and systematicity, are related to mental health further suggest that special attention should be paid to cultivating these specific CT dispositions so as to enhance the control of students over impulsive behaviors in their mental health promotions.
Conclusions
This study revealed that two CT dispositions, truth-seeking and systematicity, were associated with individual differences in mental health. Furthermore, the relationship between critical thinking and mental health was mediated by motor impulsivity and non-planning impulsivity. These findings provide a preliminary account of how human critical thinking is associated with mental health. Practically, developing mental health promotion programs for university students is suggested to pay special attention to cultivating their critical thinking dispositions (especially truth-seeking and systematicity) and enhancing the control of individuals over impulsive behaviors.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by HUST Critical Thinking Research Center (Grant No. 2018CT012). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
XR designed the study and revised the manuscript. ZL collected data and wrote the manuscript. SL assisted in analyzing the data. SS assisted in re-drafting and editing the manuscript. All the authors contributed to the article and approved the submitted version.
This work was supported by the Social Science Foundation of China (grant number: BBA200034).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. ^ We re-analyzed the data by controlling for age and gender of the participants in the regression analyses. The results were virtually the same as those reported in the study.
Barry, A., Parvan, K., Sarbakhsh, P., Safa, B., and Allahbakhshian, A. (2020). Critical thinking in nursing students and its relationship with professional self-concept and relevant factors. Res. Dev. Med. Educ. 9, 7–7. doi: 10.34172/rdme.2020.007
CrossRef Full Text | Google Scholar
Benzi, I. M. A., Emanuele, P., Rossella, D. P., Clarkin, J. F., and Fabio, M. (2019). Maladaptive personality traits and psychological distress in adolescence: the moderating role of personality functioning. Pers. Indiv. Diff. 140, 33–40. doi: 10.1016/j.paid.2018.06.026
Billieux, J., Gay, P., Rochat, L., and Van der Linden, M. (2010). The role of urgency and its underlying psychological mechanisms in problematic behaviours. Behav. Res. Ther. 48, 1085–1096. doi: 10.1016/j.brat.2010.07.008
PubMed Abstract | CrossRef Full Text | Google Scholar
Butler, H. A., Pentoney, C., and Bong, M. P. (2017). Predicting real-world outcomes: Critical thinking ability is a better predictor of life decisions than intelligence. Think. Skills Creat. 25, 38–46. doi: 10.1016/j.tsc.2017.06.005
Chan, C. (2019). Using digital storytelling to facilitate critical thinking disposition in youth civic engagement: a randomized control trial. Child. Youth Serv. Rev. 107:104522. doi: 10.1016/j.childyouth.2019.104522
Chen, M. R. A., and Hwang, G. J. (2020). Effects of a concept mapping-based flipped learning approach on EFL students' English speaking performance, critical thinking awareness and speaking anxiety. Br. J. Educ. Technol. 51, 817–834. doi: 10.1111/bjet.12887
Cuijpers, P. (2019). Targets and outcomes of psychotherapies for mental disorders: anoverview. World Psychiatry. 18, 276–285. doi: 10.1002/wps.20661
Duffy, M. E., Twenge, J. M., and Joiner, T. E. (2019). Trends in mood and anxiety symptoms and suicide-related outcomes among u.s. undergraduates, 2007–2018: evidence from two national surveys. J. Adolesc. Health. 65, 590–598. doi: 10.1016/j.jadohealth.2019.04.033
Dwyer, C. P. (2017). Critical Thinking: Conceptual Perspectives and Practical Guidelines . Cambridge: Cambridge University Press.
Google Scholar
Facione, P. A. (1990). Critical Thinking: Astatement of Expert Consensus for Purposes of Educational Assessment and Instruction . Millibrae, CA: The California Academic Press.
Fortgang, R. G., Hultman, C. M., van Erp, T. G. M., and Cannon, T. D. (2016). Multidimensional assessment of impulsivity in schizophrenia, bipolar disorder, and major depressive disorder: testing for shared endophenotypes. Psychol. Med. 46, 1497–1507. doi: 10.1017/S0033291716000131
Franco, A. R., Costa, P. S., Butler, H. A., and Almeida, L. S. (2017). Assessment of undergraduates' real-world outcomes of critical thinking in everyday situations. Psychol. Rep. 120, 707–720. doi: 10.1177/0033294117701906
Gambrill, E. (2005). “Critical thinking, evidence-based practice, and mental health,” in Mental Disorders in the Social Environment: Critical Perspectives , ed S. A. Kirk (New York, NY: Columbia University Press), 247–269.
PubMed Abstract | Google Scholar
Ghanizadeh, A. (2017). The interplay between reflective thinking, critical thinking, self-monitoring, and academic achievement in higher education. Higher Educ. 74. 101–114. doi: 10.1007/s10734-016-0031-y
Gilbert, T. (2003). Some reflections on critical thinking and mental health. Teach. Phil. 24, 333–339. doi: 10.5840/teachphil200326446
Gregory, R. (1991). Critical thinking for environmental health risk education. Health Educ. Q. 18, 273–284. doi: 10.1177/109019819101800302
Hayes, A. F. (2009). Beyond Baron and Kenny: Statistical mediation analysis in the newmillennium. Commun. Monogr. 76, 408–420. doi: 10.1080/03637750903310360
Hollon, S. D., and Beck, A. T. (2013). “Cognitive and cognitive-behavioral therapies,” in Bergin and Garfield's Handbook of Psychotherapy and Behavior Change, Vol. 6 . ed M. J. Lambert (Hoboken, NJ: Wiley), 393–442.
Hong, L., Lin, C. D., Bray, M. A., and Kehle, T. J. (2010). The measurement of stressful events in chinese college students. Psychol. Sch. 42, 315–323. doi: 10.1002/pits.20082
CrossRef Full Text
Jacobs, S. S. (1995). Technical characteristics and some correlates of the california critical thinking skills test, forms a and b. Res. Higher Educ. 36, 89–108.
Kargar, F. R., Ajilchi, B., Goreyshi, M. K., and Noohi, S. (2013). Effect of creative and critical thinking skills teaching on identity styles and general health in adolescents. Proc. Soc. Behav. Sci. 84, 464–469. doi: 10.1016/j.sbspro.2013.06.585
Leclair, M. C., Lemieux, A. J., Roy, L., Martin, M. S., Latimer, E. A., and Crocker, A. G. (2020). Pathways to recovery among homeless people with mental illness: Is impulsiveness getting in the way? Can. J. Psychiatry. 65, 473–483. doi: 10.1177/0706743719885477
Lee, H. S., Kim, S., Choi, I., and Lee, K. U. (2008). Prevalence and risk factors associated with suicide ideation and attempts in korean college students. Psychiatry Investig. 5, 86–93. doi: 10.4306/pi.2008.5.2.86
Li, S., Ren, X., Schweizer, K., Brinthaupt, T. M., and Wang, T. (2021). Executive functions as predictors of critical thinking: behavioral and neural evidence. Learn. Instruct. 71:101376. doi: 10.1016/j.learninstruc.2020.101376
Lin, Y. (2018). Developing Critical Thinking in EFL Classes: An Infusion Approach . Singapore: Springer Publications.
Luo, Q. X., and Yang, X. H. (2002). Revising on Chinese version of California critical thinkingskillstest. Psychol. Sci. (Chinese). 25, 740–741.
Mamun, M. A., Misti, J. M., Hosen, I., and Mamun, F. A. (2021). Suicidal behaviors and university entrance test-related factors: a bangladeshi exploratory study. Persp. Psychiatric Care. 4, 1–10. doi: 10.1111/ppc.12783
Patton, J. H., Stanford, M. S., and Barratt, E. S. (1995). Factor structure of the Barratt impulsiveness scale. J Clin. Psychol. 51, 768–774. doi: 10.1002/1097-4679(199511)51:63.0.CO;2-1
Peng, M. C., Wang, G. C., Chen, J. L., Chen, M. H., Bai, H. H., Li, S. G., et al. (2004). Validity and reliability of the Chinese critical thinking disposition inventory. J. Nurs. China (Zhong Hua Hu Li Za Zhi). 39, 644–647.
Profetto-Mcgrath, J. (2005). Critical thinking and evidence-based practice. J. Prof. Nurs. 21, 364–371. doi: 10.1016/j.profnurs.2005.10.002
Ren, X., Tong, Y., Peng, P., and Wang, T. (2020). Critical thinking predicts academic performance beyond general cognitive ability: evidence from adults and children. Intelligence 82:101487. doi: 10.1016/j.intell.2020.101487
Sanja, M., and Krstivoje, S. (2015). Developing critical thinking in elementary mathematics education through a suitable selection of content and overall student performance. Proc. Soc. Behav. Sci. 180, 653–659. doi: 10.1016/j.sbspro.2015.02.174
Stupple, E., Maratos, F. A., Elander, J., Hunt, T. E., and Aubeeluck, A. V. (2017). Development of the critical thinking toolkit (critt): a measure of student attitudes and beliefs about critical thinking. Think. Skills Creat. 23, 91–100. doi: 10.1016/j.tsc.2016.11.007
Suliman, W. A., and Halabi, J. (2007). Critical thinking, self-esteem, and state anxiety of nursing students. Nurse Educ. Today. 27, 162–168. doi: 10.1016/j.nedt.2006.04.008
Ugwuozor, F. O., Otu, M. S., and Mbaji, I. N. (2021). Critical thinking intervention for stress reduction among undergraduates in the Nigerian Universities. Medicine 100:25030. doi: 10.1097/MD.0000000000025030
Velotti, P., Garofalo, C., Petrocchi, C., Cavallo, F., Popolo, R., and Dimaggio, G. (2016). Alexithymia, emotion dysregulation, impulsivity and aggression: a multiple mediation model. Psychiatry Res. 237, 296–303. doi: 10.1016/j.psychres.2016.01.025
Wang, K., Shi, H. S., Geng, F. L., Zou, L. Q., Tan, S. P., Wang, Y., et al. (2016). Cross-cultural validation of the depression anxiety stress scale−21 in China. Psychol. Assess. 28:e88. doi: 10.1037/pas0000207
West, R. F., Toplak, M. E., and Stanovich, K. E. (2008). Heuristics and biases as measures of critical thinking: associations with cognitive ability and thinking dispositions. J. Educ. Psychol. 100, 930–941. doi: 10.1037/a0012842
Yoshida, T., Ichikawa, T., Ishikawa, T., and Hori, M. (1998). Mental health of visually and hearing impaired students from the viewpoint of the University Personality Inventory. Psychiatry Clin. Neurosci. 52, 413–418.
Yoshinori, S., and Marcus, G. (2013). The dual effects of critical thinking disposition on worry. PLoS ONE 8:e79714. doi: 10.1371/journal.pone.007971
Zhang, J., Lanza, S., Zhang, M., and Su, B. (2015). Structure of the University personality inventory for chinese college students. Psychol. Rep. 116, 821–839. doi: 10.2466/08.02.PR0.116k26w3
Keywords: mental health, critical thinking ability, critical thinking disposition, impulsivity, depression
Citation: Liu Z, Li S, Shang S and Ren X (2021) How Do Critical Thinking Ability and Critical Thinking Disposition Relate to the Mental Health of University Students? Front. Psychol. 12:704229. doi: 10.3389/fpsyg.2021.704229
Received: 04 May 2021; Accepted: 21 July 2021; Published: 19 August 2021.
Reviewed by:
Copyright © 2021 Liu, Li, Shang and Ren. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xuezhu Ren, renxz@hust.edu.cn
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- First Appointment Online Booking
- One To One Therapy
- Specialist in PTSD & Trauma Online Counselling
- Executive Coaching & Management Therapy
- Professional Patient Referral Therapy Services
- Bipolar Disorder Therapy
- Anger Management Therapy
- Anxiety Therapy
- Confidence Therapy
- Depression Therapy
- Marriage Therapy
- Panic Therapy
- Sex Therapy
- Trauma / PTSD Therapy
- Full List of Therapy Services
- How To Stress Less.
- How To Change Your Life.
- Hypnotherapy Audiobooks
- Meditation Audiobooks
- Audiobooks With Audible
- Audiobooks With iTunes
- Erectile Dysfunction Solutions
- Premature Ejaculation Solution
- Weight Loss Support
- Supplements For The Brain
- Recommended Brands
- Recommended Reading
- Training & Workshops For Your Business
The Science Behind Critical Thinking and Its Role in Mental Health
In the journey towards understanding and improving mental health, one cannot overlook the influence of a powerful cognitive tool known as critical thinking..
Here we will delve into the science underpinning critical thinking and shed light on its role in bolstering mental health.
Exploring the Foundations of Critical Thinking
The term 'critical thinking' encompasses a broad set of cognitive skills and dispositions aimed at objective analysis and evaluation of information. It involves thinking in a clear, logical, and reflective manner to make reasoned judgements. Critical thinking is not merely being critical in the negative sense, but rather, it's about engaging with information critically - questioning, analysing, and evaluating - to reach a sound, unbiased conclusion.
The science behind critical thinking is rooted in various cognitive processes, including perception, memory, attention, and problem-solving. It involves the prefrontal cortex, the part of the brain associated with complex cognitive behaviour, decision-making, and social behaviour. A strong capacity for critical thinking implies that these cognitive processes and brain regions are functioning optimally.
Critical Thinking and Mental Health: The Connection
The relationship between critical thinking and mental health is more intertwined than it might initially appear. Many mental health issues can be traced back to negative or distorted thinking patterns. These unhelpful thinking styles can lead to emotional distress and behavioural problems. It's here that critical thinking comes into play, as it equips individuals with the ability to identify, analyse, and ultimately challenge these negative thought patterns.
The Interplay of Perception and Critical Thinking
Perception, the process of interpreting the information that we receive through our senses, plays a significant role in critical thinking. It shapes our understanding of the world around us and influences our reactions to various situations. However, perception can sometimes be biased or distorted, leading to misunderstandings or misconceptions.
Critical thinking allows us to scrutinise our perceptions and question their accuracy. It encourages us to seek evidence and consider alternative perspectives, leading to a more accurate and comprehensive understanding of our experiences. This process can have a profound impact on our mental health, as it helps to challenge distorted perceptions that can fuel negative emotions or unhealthy behaviours.
Memory's Role in Critical Thinking
Memory, another key cognitive process, also intersects with critical thinking. Our memories of past experiences can shape our current thoughts, feelings, and behaviours. However, memories are not always accurate representations of reality. They can be influenced by our current mood, biases, and beliefs, leading to distorted recollections.
Critical thinking can help us evaluate our memories objectively. It prompts us to question the accuracy of our recollections and consider the influence of external factors. This reflective approach can prevent us from basing our beliefs or behaviours on distorted memories, thereby enhancing our mental health.
Attention and Its Influence on Critical Thinking
Attention, the cognitive process of selectively concentrating on one aspect while ignoring others, is crucial for critical thinking. It enables us to focus on relevant information and ignore irrelevant distractions. However, attention can be biased towards negative information, especially in individuals with mental health issues such as anxiety or depression.
Critical thinking skills can aid in managing attentional biases. It involves questioning why we are focusing on certain aspects and ignoring others, considering the impact of this focus, and making a conscious effort to direct our attention in a more balanced manner. This approach can reduce negative bias, improve emotional well-being, and enhance overall mental health.
Problem-Solving: A Crucial Component of Critical Thinking
Problem-solving is an integral part of critical thinking. It involves identifying problems, generating potential solutions, and evaluating these solutions to make an informed decision. Individuals with strong problem-solving skills are often good critical thinkers, as they can analyse situations objectively, consider various solutions, and make reasoned decisions based on evidence. In the context of mental health, problem-solving skills can help manage stress, navigate life's challenges, and improve overall well-being.
Cognitive Biases and Critical Thinking
Cognitive biases, systematic errors in thinking that influence our judgements and decisions, can impede critical thinking. They can lead to distorted perceptions, irrational beliefs, and poor decision-making, which can negatively impact mental health. Common cognitive biases include confirmation bias, where we focus on information that confirms our pre-existing beliefs, and negativity bias, where we pay more attention to negative information.
Critical thinking can help us recognise and overcome these cognitive biases. It encourages us to question our biases, seek diverse perspectives, and make decisions based on objective evidence rather than biased perceptions. By mitigating the impact of cognitive biases, critical thinking can promote healthier thought patterns, better decision-making, and improved mental health.
The Impact of Critical Thinking on Emotional Intelligence
Emotional intelligence, the ability to understand, use, and manage our own emotions in positive ways, can be enhanced through critical thinking. By critically analysing our emotional responses, we can gain insights into our emotional patterns, understand the triggers for certain emotions, and develop effective strategies to manage these emotions. This understanding can lead to improved emotional regulation, better interpersonal relationships, and enhanced mental health.
Critical Thinking and Resilience
Critical thinking also plays a significant role in building resilience, the ability to bounce back from adversity. Resilient individuals use critical thinking to understand the nature of the adversity, explore various coping strategies, and make informed decisions to overcome the challenge. This ability not only helps manage the immediate adversity but also fosters mental strength, which can safeguard against future challenges.
In conclusion, the science behind critical thinking and its role in mental health is a fascinating and integral area of exploration. By enhancing our cognitive processes, helping us navigate our emotions, and bolstering our resilience, critical thinking serves as a powerful tool for mental health.
At times, life can be overwhelming and leave us feeling lost, anxious, or depressed.
Counselling can provide the support and guidance needed to navigate difficult times and achieve mental well-being. We offer a safe and confidential space to explore your thoughts, feelings, and concerns. We believe that everyone deserves access to quality mental health care, and we strive to provide an inclusive and non-judgmental environment for all.
If you are struggling with mental health issues or feeling overwhelmed, we invite you to reach out to us for support. We are here to listen, guide, and empower you towards a healthier and happier life. Don't let mental health challenges hold you back from living your best life. Contact us today to schedule an appointment and take the first step towards better mental health.

How Do Critical Thinking Ability and Critical Thinking Disposition Relate to the Mental Health of University Students?
Affiliation.
- 1 School of Education, Huazhong University of Science and Technology, Wuhan, China.
- PMID: 34489809
- PMCID: PMC8416899
- DOI: 10.3389/fpsyg.2021.704229
Theories of psychotherapy suggest that human mental problems associate with deficiencies in critical thinking. However, it currently remains unclear whether both critical thinking skill and critical thinking disposition relate to individual differences in mental health. This study explored whether and how the critical thinking ability and critical thinking disposition of university students associate with individual differences in mental health in considering impulsivity that has been revealed to be closely related to both critical thinking and mental health. Regression and structural equation modeling analyses based on a Chinese university student sample ( N = 314, 198 females, M age = 18.65) revealed that critical thinking skill and disposition explained a unique variance of mental health after controlling for impulsivity. Furthermore, the relationship between critical thinking and mental health was mediated by motor impulsivity (acting on the spur of the moment) and non-planning impulsivity (making decisions without careful forethought). These findings provide a preliminary account of how human critical thinking associate with mental health. Practically, developing mental health promotion programs for university students is suggested to pay special attention to cultivating their critical thinking dispositions and enhancing their control over impulsive behavior.
Keywords: critical thinking ability; critical thinking disposition; depression; impulsivity; mental health.
Copyright © 2021 Liu, Li, Shang and Ren.
How do mental disorders impact our decision-making?
For some people suffering from illnesses such as schizophrenia and substance use disorder – previously referred to as “ substance abuse ” – making the right choices can be extremely difficult.
In fact, many mental illnesses feature problems with cognition (thinking and comprehension), including depression and bipolar disorder. Decision-making ability varies in healthy people, too, sometimes as a consequence of differences in genetics .
What’s happening in the brains of these people that puts them on unequal footing to the rest of us?
Even simple decisions are complex
It’s important to note in day-to-day situations, there’s often no distinctly “right” or “wrong” choice to be made. However, some choices do result in healthier or more productive outcomes for us and those around us.
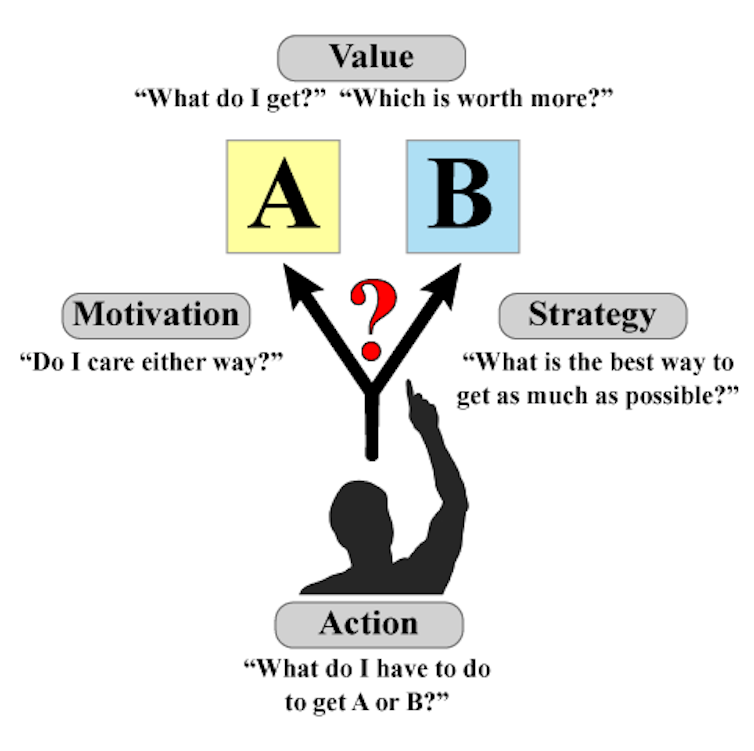
Our brains carry out a suite of complex processes when making decisions. And there are four important factors in each decision we make: value, motivation, action and strategy.
- Mapping health risks for people with mental disorders
- Researchers recognised for expanding knowledge of schizophrenia
- Research bears fruit for schizophrenia patients
When choosing between two options, say A and B, we first need to understand which choice will be more rewarding, or provide more value . Our personal motivation to attain this reward then acts to bias which option we choose, or whether we make a choice at all.
Understanding what action is required to obtain A, or B, is also important. Combining all this information, we try to understand which strategy will maximise our rewards. And this lets us improve our decision-making ability over time.
Connections interrupted by mental disorders
We refer to our personal history and past experiences to guide our future choices. But mental disorders often cause problems in the decision-making process.
Research shows people with schizophrenia can have trouble understanding the relationship between their actions and the outcomes . This means they might keep selecting A, even if they know it’s no longer as valuable as B.
They’re also more willing to adopt strategies based on less information, in other words “ jump to conclusions ”, about outcomes.
Substance use disorder, particularly with stimulants such as methamphetamine or cocaine, often leads to people getting stuck when certain outcomes change .
For example, if we reversed all the street lights so red meant “go” and green meant “stop” without telling anyone, most people would get an initial shock but would eventually alter their behaviour.
People with stimulant dependence, however, would take longer to learn to stop on the green light – even if they kept getting into car accidents. This is because excessive stimulant use impacts regions in the brain that are crucial to adapting to changing environments.
How the brain decodes each decision
The human brain contains multiple circuits (like pathways) and chemical messengers called “neurotransmitters”. These are responsible for guiding the processes discussed above.
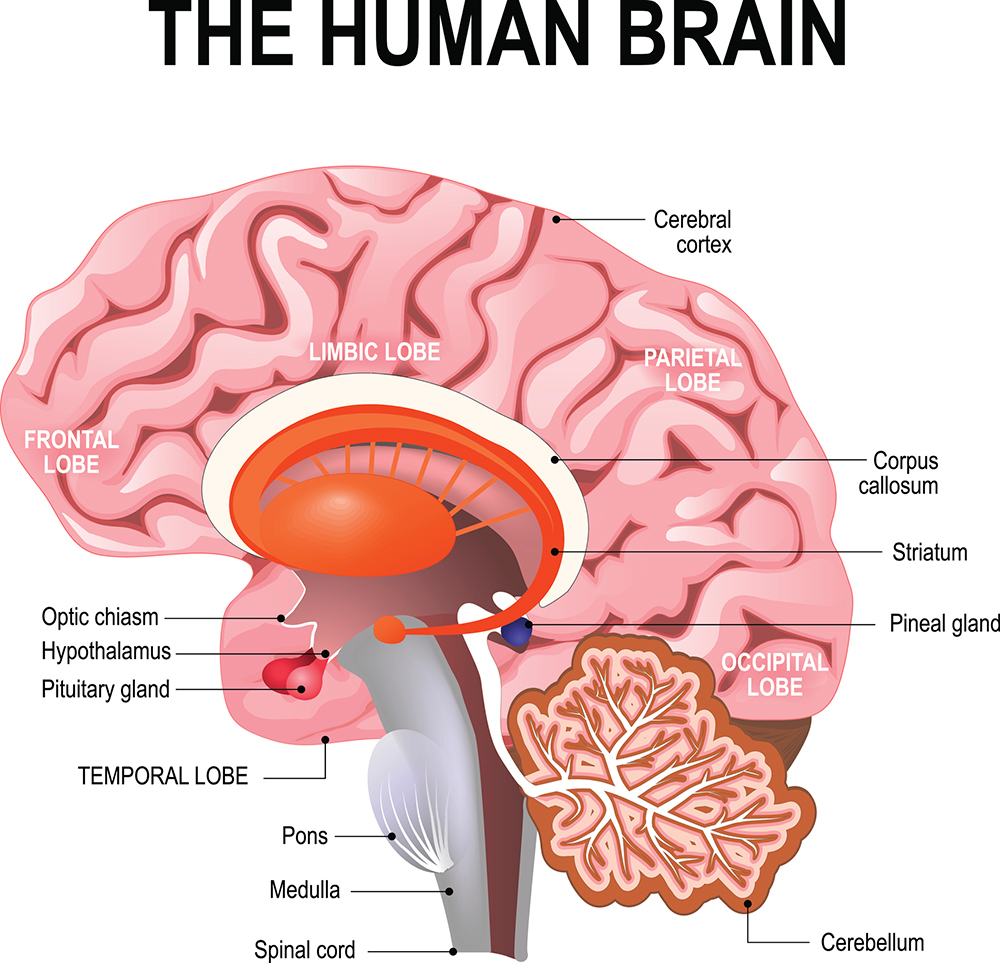
The decision-making circuits commonly associated with schizophrenia and substance use disorder include areas of the “cortex” – the outer part of our brain important for complex thought (especially the frontal lobe) – that “talk” to hub areas such as the “striatum”. The striatum lets us select and then initiate an action to achieve a specific goal.
Different cortical areas are used to compute different processes in the brain. The prefrontal cortex helps us understand when a strategy needed for success changes. So, if we replaced all the traffic lights with sirens, the prefrontal cortex would help us realise this and adjust.
When the anticipated outcome of a choice changes (such as if A was better, but then suddenly B became better), the orbitofrontal cortex helps us identify this. Similarly, the striatum is key for anticipating what an outcome will be and when we will get the reward.
Dopamine helps make choice a reality
Extensive research efforts have found the brains of people experiencing schizophrenia function differently in multiple areas. It’s believed this could contribute to decision-making problems.
For the psychotic symptoms observed in schizophrenia (such as hallucinations and delusions), alterations in the neurotransmitter dopamine are important. Dopamine is a chemical in the brain that’s key for anticipating rewards, making decisions and controlling the physical actions necessary to act on our choices.
In our research , we’ve argued increases in dopamine in the striatum may cause problems with how the brain integrates information from the cortex, resulting in decision-making difficulties. However, this may only be the case in some individuals .
Stimulants also cause excessive dopamine release. They can alter the balance between goal-directed behaviours, which are flexible and respond to environmental changes – and habits, which are automatic and hard to break.
Usually, when we learn something new our brain keeps adapting and incorporating new information. But this is slow and cognitively demanding. Substance dependence can accelerate a person’s progression to habitual behaviour, wherein a set strategy or response become ingrained.
This then makes it hard to stop seeking drugs, even if the individual no longer finds them enjoyable .
How to help people make better decisions
Unfortunately, problems with cognitive ability are hard to treat. There are no medications for schizophrenia or stimulant dependence shown to reliably improve cognition . This is a consequence of the human brain’s complexity.
That said, there are ways we can all improve our memory and decision-making, which may also help those with mental illnesses causing cognition problems.
For instance, cognitive remediation therapy is a behavioural approach that trains the brain to respond to certain situations better. For people with schizophrenia, it may improve visual memory and perhaps more complex decision-making.
Not being able to navigate decisions day-to-day is one of the most debilitating aspects of disorders that impact cognition. This leads to difficulties in maintaining work, keeping friends and leading a fulfilling life.
We need more research to understand how different brains make different decisions. Hopefully then we can improve the lives of those living with mental illness.
James Kesby , UQ Amplify Researcher, The University of Queensland and Shuichi Suetani , Psychiatrist, Queensland Brain Institute, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article .
- Builders transform parking lot into avenue for dementia rese...
- The importance of brain health to prevent dementia
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 06 December 2017
Food for thought: how nutrition impacts cognition and emotion
- Sarah J. Spencer 1 ,
- Aniko Korosi 2 ,
- Sophie Layé 3 ,
- Barbara Shukitt-Hale 4 &
- Ruth M. Barrientos 5
npj Science of Food volume 1 , Article number: 7 ( 2017 ) Cite this article
153k Accesses
147 Citations
189 Altmetric
Metrics details
- Neuroendocrine diseases
More than one-third of American adults are obese and statistics are similar worldwide. Caloric intake and diet composition have large and lasting effects on cognition and emotion, especially during critical periods in development, but the neural mechanisms for these effects are not well understood. A clear understanding of the cognitive–emotional processes underpinning desires to over-consume foods can assist more effective prevention and treatments of obesity. This review addresses recent work linking dietary fat intake and omega-3 polyunsaturated fatty acid dietary imbalance with inflammation in developing, adult, and aged brains. Thus, early-life diet and exposure to stress can lead to cognitive dysfunction throughout life and there is potential for early nutritional interventions (e.g., with essential micronutrients) for preventing these deficits. Likewise, acute consumption of a high-fat diet primes the hippocampus to produce a potentiated neuroinflammatory response to a mild immune challenge, causing memory deficits. Low dietary intake of omega-3 polyunsaturated fatty acids can also contribute to depression through its effects on endocannabinoid and inflammatory pathways in specific brain regions leading to synaptic phagocytosis by microglia in the hippocampus, contributing to memory loss. However, encouragingly, consumption of fruits and vegetables high in polyphenolics can prevent and even reverse age-related cognitive deficits by lowering oxidative stress and inflammation. Understanding relationships between diet, cognition, and emotion is necessary to uncover mechanisms involved in and strategies to prevent or attenuate comorbid neurological conditions in obese individuals.
Similar content being viewed by others

Microdosing with psilocybin mushrooms: a double-blind placebo-controlled study

Alzheimer’s disease risk reduction in clinical practice: a priority in the emerging field of preventive neurology
Investigating nutrient biomarkers of healthy brain aging: a multimodal brain imaging study
Introduction.
Cognitive and emotional dysfunctions are an increasing burden in our society. The exact factors and underlying mechanisms precipitating these disorders have not yet been elucidated. Next to our genetic makeup, the interplay between specific environmental challenges occurring during well-defined developmental periods seems to play an important role. Interestingly, such brain dysfunction most often co-occurs with metabolic disorders (e.g., obesity) and/or poor dietary habits; obesity and poor diet can lead to negative health implications including cognitive and mood dysfunctions, suggesting a strong interaction between these elements (Fig. 1 ). Obesity is a global phenomenon, with around 38% of adults and 18% of children and adolescents worldwide classified as either overweight or obese. 1 Even in the absence of obesity, poor diet is commonplace, 2 with, for instance, many eating foods that are highly processed and lacking in important polyphenols and anti-oxidants or that contain well-below the recommended levels of omega-3 polyunsaturated fatty acids (PUFA). In this review, we will discuss the extent of, and mechanisms for, diet’s influence on mood and cognition during different stages of life, with a focus on microglial activation, glucocorticoids and endocannabinoids (eCBs).
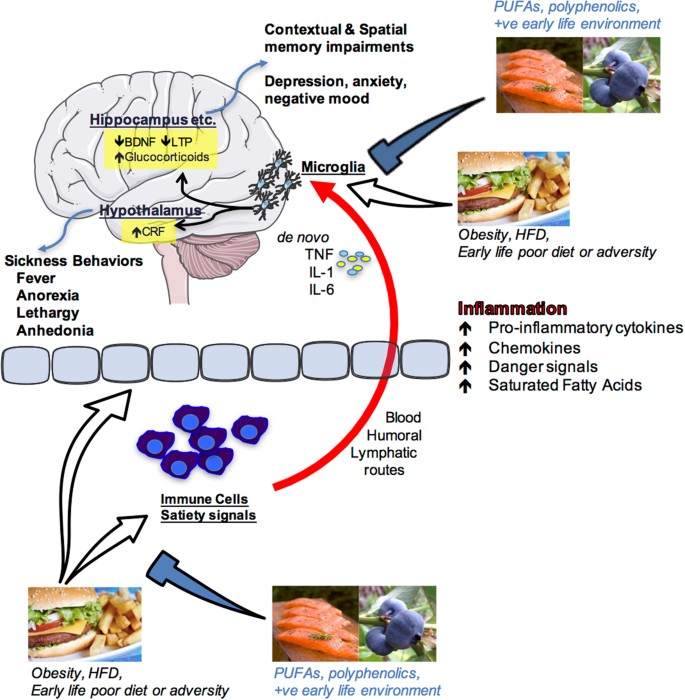
Schematic depiction of how nutrition influences cognition and emotion. Overeating, obesity, acute high-fat diet consumption, poor early-life diet or early life adversity can produce an inflammatory response in peripheral immune cells and centrally as well as having impact upon the blood–brain interface and circulating factors that regulate satiety. Peripheral pro-inflammatory molecules (cytokines, chemokines, danger signals, fatty acids) can signal the immune cells of the brain (most likely microglia) via blood-borne, humoral, and/or lymphatic routes. These signals can either sensitize or activate microglia leading to de novo production of pro-inflammatory molecules such as interleukin-1beta (IL1β), IL-6, and tumor necrosis factor alpha (TNFα) within brain structures that are known to mediate cognition (hippocampus) and emotion (hypothalamus, amygdala, prefrontal cortex and others). Amplified inflammation in these regions impairs proper functioning leading to memory impairments and/or depressive-like behaviors. Polyunsaturated fatty acids (PUFA), polyphenolics, and a positive (+ve) early life environment (appropriate nutrition and absence of significant stress or adversity) can prevent these negative outcomes by regulating peripheral and central immune cell activity. Images are adapted from Servier Medical Art, which is licensed under a Creative Commons Attribution 3.0 Unported License https://creativecommons.org/licenses/by/3.0/ . Salmon and hamburger images were downloaded from Bing.com with the License filter set to “free to share, and use commercially”. The blueberry image is courtesy of author Assistant Prof. Ruth Barrientos
Perinatal diet disrupts cognitive function long-term, a role for microglia
Poor diet in utero and during early postnatal life can cause lasting changes in many aspects of metabolic and central functions, including impairments in cognition and accelerated brain aging, 3 but see. 4 Maternal gestational diabetes and even a junk food diet in the non-diabetic can lead to metabolic complications, including diabetes and obesity in the offspring. 5 , 6 It can also cause changes in reward processing in the offspring brain such that they grow to prefer foods high in fat and sucrose. 7 , 8 Similarly, early introduction of solid food in children and high childhood consumption of fatty foods and sweetened drinks can accelerate weight gain and lead to metabolic complications long-term that may be associated with poorer executive function. 9 On the other hand, some dietary supplements can positively influence cognition, as is seen with supplementation of baby formula with long chain omega-3 PUFA improving cognition in babies. 10 In these randomized control trials (RCTs), an omega-3 PUFA-enriched formula beginning shortly after birth, or 6 weeks’ breast feeding, significantly improved performance of 9-month old babies on a problem solving task (a two-step task to retrieve a rattle, known to correlate with performance on IQ tasks).
From animal models, it is clear that the effects of diet in early life are far-reaching. Even obesity in rat sires (that play no part in rearing the offspring) leads to pancreatic beta cell dysfunction in female offspring, which can be passed on to the next generation. 11 Obesity and high-fat diet feeding in rat and mouse dams during pregnancy and lactation leads to impairments in several tests of mood, including those modeling depressive and anxious behaviors, as well as negatively impacting cognition. 12 Diet in the post-partum to weaning period can impact similar behaviors. 13
Additional to the impact of a prenatal diet, over-consumption of the mother’s milk during the first 3 weeks of a rat’s life leads to lasting obesity in males and females. 14 This neonatal overfeeding also disrupts cognitive function. For example, neonatally overfed rats perform poorly in the novel object recognition test and in the delayed spatial win-shift radial arm maze, as adults, compared with control rats. 15 These findings are interesting to compare with the effects of poor diet in adults where a longer-term high-fat diet (around 20 weeks in the rat) 16 , 17 , 18 and / or high-fat diet in conjunction with a pre-diabetic phenotype 19 is necessary to induce cognitive dysfunction. While there are no differences in post-learning synaptogenesis (synaptophysin) or apoptosis (caspase-3) to explain the effects seen in the neonatally overfed, these rats do have an impaired microglial response to the learning task. 15
Microglia are one of the major immune cell populations in the brain. In development, they are essential for synaptic pruning, while in a mature animal their major role is in mounting a pro-inflammatory immune response and phagocytosing pathogens and injured brain cells. 20 Hyper-activated microglia can lead to cognitive dysfunction through excess pro-inflammatory cytokine production causing impaired long-term potentiation-induction, reduced production of plasticity-related molecules including brain-derived neurotrophic factor and insulin-like growth factor-1, and reduced synaptic plasticity 20 However, an appropriate microglial response may also be essential for effective learning.
Neonatally overfed rats have more microglia in the CA1 region of the hippocampus at postnatal day 14, i.e., while they still have access to excess maternal milk and are undergoing accelerated weight gain. These microglia also have larger soma and retracted processes, indicative of a more activated phenotype. By the time these rats reach adulthood, there persists an increase in the area immunolabelled with microglial marker Iba1 in the dentate gyrus. In the neonatally overfed, the microglial response to a learning task is less robust than in controls. This effect is associated with a suppression of cell proliferation in control animals relative to the neonatally overfed, potentially to preserve existing neuronal networks and minimize novel inputs while learning takes place. 21 Interestingly, global inducible microglial and monocyte depletion can lead to improved performance in the Barnes maze, 22 suggesting withdrawal of microglial activity at specific learning phases is important for learning. These findings implicate microglia in the long-term effects of early life overfeeding on cognition suggesting normal microglia must be able to robustly respond to learning tasks and neonatal overfeeding impairs their ability to do so.
Neuroinflammatory processes, including the role of microglia, can clearly be impacted by neonatal diet and represent at least one contributing mechanism for how cognitive function is affected. Neuroinflammation and microglia can also be impacted by other early life events and play a significant role in how stress during development alters long-term physiology.
Early-life stress (ES) programs vulnerability to cognitive disorders
ES alters brain structure and function life-long, leading to increased vulnerability to develop emotional and cognitive disorders as is evident from several preclinical and clinical studies. 23 , 24 , 25 The exact underlying mechanisms for such programming remain elusive. There is extensive seminal work indicating a key role for sensory stimuli from the mother and neuroendocrine factors (e.g., stress hormones) in this programming, 26 , 27 however it has been recently suggested that these factors might act synergistically with metabolic and nutritional elements. 28 In fact, ES is associated with increased vulnerability to develop metabolic disorders such as obesity, which mostly co-occur with cognitive deficits, 29 , 30 and both ES and an adverse early nutritional environment lead to strikingly similar cognitive impairments later in life, 28 , 31 suggesting that metabolic factors and nutritional elements might mediate some of the ES effects on brain structure and function.
The brain has a very high demand for nutrients in this early period and nutritional imbalances affect normal neurodevelopment resulting in lasting cognitive deficits. 32 Understanding the role of metabolic factors and specific nutrients in this context is key to develop effective peripheral (e.g., nutritional) intervention strategies. A mouse model of the chronic ES of limited nesting and bedding material during the first postnatal week has been shown to lead to aberrant maternal care, which leads to cognitive decline in the ES offspring. 24 , 33 , 34
The hippocampus, a brain region key for cognitive functions, is permanently altered in its structure and function in these ES-exposed offspring. The hippocampus is in fact particularly sensitive to the early-life environment as it continues its development into the postnatal period. 35 Adult neurogenesis (AN) is a unique form of plasticity, which takes place in the hippocampus, consisting of the proliferation of neuronal progenitor cells that differentiate and mature into fully functional neurons that subsequently integrate into the existing hippocampal circuitry. These newly formed neurons are involved in various aspects of hippocampus-dependent learning and memory. 36 AN is affected persistently by ES 24 , 37 and, more precisely, while ES exposure initially increases neurogenesis (i.e., proliferation and differentiation of newborn cells) at postnatal day 9, at later time points (postnatal day 150), the survival of the newly born cells is reduced. 24 In addition, ES affects the neuroinflammatory profile in a lasting manner, with, for example, increased CD68 (phagocytic microglia expression) in adulthood. 38
Importantly, ES persistently affects peripheral adipose tissue metabolism as well. White adipose mass (WAT), plasma leptin (the adipokine released from the WAT) and leptin mRNA expression in WAT are persistently reduced in ES-exposed offspring. 39 In addition, exposure of ES mice to an unhealthy western style diet, leads to a higher increase in adiposity in these mice when compared to controls. These findings suggest that ES exposure leads to metabolic dysregulation and a greater vulnerability to develop obesity in a moderately obesogenic environment. Whether these metabolic alterations contribute to the ES-induced cognitive deficits warrants further investigation. 39
In addition to peripheral metabolism, ES-induced alterations in the nutritional composition of the dam’s milk, and/or nutrient intake/absorption by the pup 25 , 28 , 40 could have lasting consequences for brain structure and function. Indeed, the essential micronutrient, methionine, a critical component of the one-carbon (1-C) metabolism that is required for methylation, and for synthesis of proteins, phospholipids and neurotransmitters, is reduced after ES exposure in plasma and hippocampus of postnatal day 9 offspring. Importantly, a short supplementation of the maternal diet only during ES exposure with essential 1-C metabolism-associated micronutrients not only restores methionine levels peripherally as well as centrally, but rescues (some of) the effects of ES on hippocampal cognitive measures in adulthood and prevents the ES-induced hypothalamic-pituitary–adrenal axis hyperactivity at postnatal day 9. 25
These studies highlight the importance of studying metabolic factors and nutrients in the ES-induced effects on the brain. In the near future, it will be key to further understand the exact mechanisms mediating the effects of nutrients and metabolic factors and the windows of opportunity for interventions on brain function, as this will open entirely new avenues for targeted nutrition for vulnerable populations. However, while the early life period is a window of particular vulnerability to the programming effects of diet and other environmental influences, diet at other phases of life is also important in dictating mood and cognition.
Adult consumption of a high-fat diet: a vulnerability factor for hippocampal-dependent memory
Adults in developed countries are consuming diets higher in saturated fats and/or refined sugars than ever before. Indeed, recent reports show that approximately 12% of American adults’ daily energy intake comes from saturated fats and 13% from added sugars, 41 significantly more than what is recommended (5–10%) by the US Department of Agriculture and the Department of Health and Human Services. Not surprisingly, these dietary habits have contributed to the increasing prevalence of obesity among adults, which is currently approximately 37% in the US, a sharp rise from the 13% prevalence rate of 1960. 42
These statistics are alarming because aside from its well-known provocation of cardiovascular disease, metabolic syndrome, and type 2 diabetes, obesity has now also been associated with mild cognitive impairments and dementia. There is growing evidence that neuroinflammation may underlie obesity-induced cognitive deficits. 9 Recently, studies have demonstrated that short-term consumption (1–7 days) of an unhealthy diet (e.g., high saturated fat and/or high sugar) triggers neuroinflammatory processes, suggesting that obesity per se may not be necessary to cause cognitive disruptions. 43 , 44 For the last 10–15 years, the hypothalamus has received the vast majority of the attention with regard to obesity-induced neuroinflammatory responses and functional declines, 45 perhaps due to its close proximity to the third ventricle, circumventricular organs, and mediobasal eminence, where inflammatory signals from the periphery have easier entry into the brain. Indeed, long chain saturated fatty acids have been shown to directly pass into the hypothalamus producing an inflammatory response there through activation of toll-like receptor 4 signaling. 46 , 47 This active passage of saturated fatty acids, however, has not been observed in the hippocampus, a key brain region that mediates learning and memory. 46 Nonetheless, high-fat diet consumption has been demonstrated to impair hippocampus-dependent memory function in humans and rodents. For example, compared to rodents that consumed a control diet, those that consumed a high-fat and/or high-sugar diet exhibited robust impairments in various types of memory (e.g., spatial, contextual), as indicated by weaker performances in the Y-maze, 48 radial arm maze, 15 novel object recognition task, 15 novel place recognition task, 44 , 49 Morris water maze, 50 and contextual fear conditioning. 18 , 51 Also, adult humans who consumed a high-fat diet for 5 days exhibited significantly reduced focused attention and reduced retrieval speed of information from working and episodic memory, compared with those who consumed a standard diet. 52
Many of these studies, and others, have shown that high-fat diet-induced cognitive deteriorations are accompanied by elevated neuroinflammatory markers or responses in the hippocampus. 15 , 18 , 44 , 48 , 49 , 50 , 51 , 53 However, the mechanisms by which these neuroinflammatory processes signal and/or affect the hippocampus are not entirely clear. There is growing evidence that high-fat diets may compromise the hippocampus by sensitizing the immune cells (most likely microglia) of this brain structure, thus priming the inflammatory response to subsequent challenging stimuli. 18 , 50 , 51 For example, one study demonstrated that adult rats that had eaten a high-fat diet for 5 months exhibited a sensitized hippocampus such that when they received a relatively mild stressor (a single, 2 s, 1.5 mA footshock) following a learning session the neuroinflammatory response in the hippocampus was potentiated compared to the response of rats that had eaten the regular chow, and this response led to deficits in long-term contextual memory. 18 Another study showed that just 3 days of consuming a high-fat diet was sufficient to sensitize the hippocampus of adult rats. Here, a low-dose peripheral immune challenge (with lipopolysaccharide; LPS) produced an exaggerated neuroinflammatory response in the hippocampus of these rats compared to those that consumed the regular chow, and also led to contextual memory deficits. 51
Significantly elevated pro-inflammatory cytokines in the hippocampus have been shown to deteriorate various mechanisms that enable synaptic plasticity (such as long-term potentiation), and thus long-term memory. 54 Sobesky et al. 51 demonstrated that high-fat diet consumption primes the cells of the hippocampus by elevating the glucocorticoid steroid hormone corticosterone in this region. Despite its classic role as an immunosuppressant, there is increasing evidence demonstrating that corticosterone can prime hippocampal microglia and potentiate the inflammatory response to a subsequent challenge. 55 , 56 , 57 For example, Frank et al. 55 elegantly showed that when corticosterone was elevated prior to a peripheral immune challenge (LPS), the resulting inflammatory response in the hippocampus was potentiated. In contrast, when corticosterone was elevated after the immune challenge, the neuroinflammatory response was suppressed. These findings suggest that the temporal relationship between the corticosterone increase and the immune challenge dictates whether a pro-inflammatory or anti-inflammatory response will result. 55 Sobesky et al. 51 found that rats that consumed the high-fat diet for 3 days exhibited significantly increased levels of corticosterone in their hippocampus compared to rats that consumed the regular chow or a novel macronutrient-matched control diet. This high-fat diet-induced corticosterone rise was accompanied by increases in the endogenous danger-associated molecular pattern high-mobility group box 1 (HMGB1), the interleukin (IL)-1 inflammasome-associated protein NLRP3, and the microglial activation marker cd11b. high-fat diet alone did not, however, elevate the pro-inflammatory cytokine IL-1β unless rats were subsequently challenged with a low-dose of LPS. Thus, LPS challenge potentiated the pro-inflammatory response in the hippocampus of high-fat diet-fed rats compared to the response to LPS in chow-fed rats. To evaluate the role of corticosterone signaling in neuroinflammatory priming caused by consumption of high-fat diet, Sobesky et al. 51 administered the glucocorticoid receptor antagonist, mifepristone, prior to high-fat diet consumption. This resulted in a normalized hippocampal IL-1β response to low-dose LPS. Furthermore, mifepristone significantly reduced the high-fat diet + LPS-induced expression of HMGB1, IκBα, and NLRP3. Moreover, mifepristone treatment effectively prevented contextual memory deficits caused by high-fat diet consumption combined with LPS challenge. These data provide strong evidence for the idea that (a) high-fat diet consumption increases corticosterone within the hippocampus, and (b) this corticosterone is a key mediator in sensitizing microglia or other immune cells of the hippocampus; (c) sensitized microglia produce a potentiated neuroinflammatory response to subsequent immune or stressful challenges, thus producing cognitive deficits. Notably, though, while high-fat diet per se can have significant detrimental impact on cognitive processes, specific dietary components may be able to reverse these effects, omega-3 PUFA are one such potentially beneficial component.
Dietary omega-3 PUFA regulate neuroinflammation and eCBs: role in mood and cognitive disorders
Since their discovery in the early 20th century, considerable attention has been paid to the roles of PUFA in brain functions. Omega-3 and omega-6 PUFA are essential fatty acids, meaning that they have to be provided by the diet. Western diet contains excessive amounts of omega-6 PUFA as compared to omega-3 leading to an unbalanced ratio between these two fatty acids with cardiovascular and brain health consequences. Essential omega-3 and omega-6 fatty acids are found in green vegetables, seeds and nuts although coming from different sources with linolenic acid (LA, 18:2 omega-6) found in most plants, coconut and palm and α-linolenic acid (ALA, 18:3 omega-3) in green leafy vegetables, flax and walnuts. Once consumed, LA and ALA are metabolized into arachidonic acid (AA, 20:4 omega-6) and docosahexaenoic acid (DHA, 22:6 omega-3), respectively.
AA and DHA are the main omega-6 and omega-3 long chain PUFA found in the brain. Both long chain PUFA have pivotal roles in brain physiology as they regulate fundamental neurobiological processes, in particular the ones involved in cognition and mood. 58 , 59 AA and DHA are esterified to the phospholipid of neuronal and glial cell membranes with a total brain phospholipid proportion of around 10% for AA and 20% for DHA. Due to the limited capacity of the brain to synthesize long chain PUFA, preformed DHA can be provided by dietary supply of oily fishes. Hence, increased consumption of DHA-rich products results in a partial replacement of AA by DHA in brain cell membranes. 60 Conversely, a lower omega-3 PUFA intake leads to lower brain levels of DHA with increased AA levels. Higher AA and DHA are reported in women as compared to men, suggesting a gender difference in PUFA levels. 61 These differences could be linked to sex hormones as they differentially influence PUFA metabolism with estrogen stimulating, and testosterone inhibiting, the conversion of both omega-3 and omega-6 precursors into their respective long chain metabolites. However, whether these differences in PUFA have a role in specific brain diseases with a gender component has been poorly questioned and requires further investigation.
After its direct consumption and/or metabolization in the liver, DHA is increased in the blood and is likely to freely enter into the brain as non-esterified fatty acid. 58 More recently, Mfsd2a (major facilitator superfamily domain-containing protein 2a), which is expressed by brain endothelial cells and adiponectin receptor 1 in the retina, has been revealed to be important to DHA uptake and retention. 62
Abnormal omega-3 PUFA levels have been extensively described in both the peripheral tissues and in the brain of patients with mood disorders or cognitive decline, leading to a large number of RCTs aiming at evaluating the effectiveness of long chain omega-3 PUFA dietary supplementation on mood and cognitive disorders. 58 , 63 Overall, the results are discordant, due to the heterogeneity of methods used to evaluate the depressive and/or cognitive symptoms, the form, dose and duration of the omega-3 PUFA supplementation, the lack of evaluation of nutritional intake and metabolism of PUFA prior to starting the supplementation, or the lack of evaluation of genotype-associated risk factors. 64 However, despite the discrepancies in the results, it is important to note that several RCTs performed in patients with depressive disorders revealed an additional effect of long chain omega-3 PUFA supplementation to antidepressant treatments. 65 Of note, a recent study identifies that depressive patients presenting a high level of inflammatory markers are more responsive to long chain omega-3 PUFA supplementation. 66 This observation is highly relevant as these PUFA are potent regulators of inflammation 58 and inflammation is a crucial component of mood disorders. Concerning cognitive decline, despite poor positive results of PUFA dietary supplementation in Alzheimer’s disease (AD) patients, RCTs using DHA supplementation in subjects carrying the apolipoprotein E ε4 (APOE4) allele, a risk factor for AD, reveal an improvement of pre-dementia. 64 Overall, discrepancies in clinical studies strongly support the need for preclinical studies aimed at depicting the mechanisms of omega-3 PUFA on brain dysfunctions, which should help to better target populations at risk of cognitive and mood disorders. In addition, the consideration of omega-3 PUFA levels in food to cover the physiological requirement of these PUFA for an optimal brain function is a challenge for the food industry.
Through direct or indirect effects, DHA and AA modulate neurotransmission and neuroinflammation, which are key processes in cognition and mood. 58 , 59 Unesterified long chain PUFA are released from cell membranes upon the activation of phospholipase A2 (PLA2) to exert their effects. 67 Once released, AA and DHA are metabolized into bioactive mediators through cyclooxygenase (COX), lipoxygenases (LOX) and cytochrome P450. 68 The conversion of AA into several prostanoids, including prostaglandins (PG), leukotrienes (LT), thromboxanes (TX) and lipoxins (LX), is crucial in the progression of inflammation, including in the brain. 58 DHA is also metabolized through the COX/LOX pathways to generate metabolites with anti-inflammatory and pro-resolutive properties. 68 In the brain, LOX-derived specialized proresolving mediators (SPMs), neuroprotectin D1 (NPD1), resolvin D5 (RvD5), and maresin 1 (MaR1) are detected. 68 , 69 Some of these SPMs potently modulate neuroinflammation in vivo and in vitro, through their direct effect on microglia. 70 , 71 DHA and SPMs are impaired at the periphery and in the brains of AD patients. 72 , 73 Interestingly, decreased DHA distribution in AD patient brains correlates with synaptic loss rather than amyloid beta (Aβ) deposition. 74 In addition, DHA or SPMs promote phagocytosis of Aβ42 by microglia 75 and modulate microglia number and activation in vivo. 76 Whether SPMs play a role in the protective activity of long chain omega-3 PUFA in mood and cognitive disorders associated to neuroinflammation remains to be established.
eCBs are other key PUFA-derived lipid mediators in the brain. The main brain AA-derived eCBs are the fatty acid ethanolamides anandamide (AEA) and 2-arachidonoylglycerol (2-AG), while docosahexaenoylethanolamide (DHEA or synaptamide) is an eCB-like derived from DHA. 77 ECBs half-life in the brain is regulated by specific catabolizing enzymes fatty acid amide hydrolase for AEA and DHEA and monoacylglycerol lipase for 2-AG. Regarding neuroinflammatory processes, AA-derived eCBs are oxidized into bioactive PG by COX and LOX, which promote inflammation. 78 AEA and 2-AG bind to at least two cannabinoid receptors, type 1 (CB1) and type 2 (CB2), which are Gi/o protein-coupled with numerous signaling pathways in the brain. 79 , 80 DHEA has a lower binding affinity for CB1 and CB2 receptors as compared to AEA and 2-AG and rather bind GPR receptors, in particular GPR110 in the brain. The dietary omega-3/omega-6 PUFA ratio directly influences the proportion of ethanolamides derived from AA and DHA. 81 The modulation of eCB is accompanied by the impairment of neuronal CB1R activity and synaptic activity in several brain structures. 82 , 83 2-AG and AEA regulate synaptic function by suppressing excitatory and inhibitory synapse neurotransmitter release by acting as retrograde messengers at presynaptic CB1. 84 The importance of brain eCB signaling in the understanding of how altered dietary intake of PUFA correlates with a range of neurological disorders is of high interest. 81 However, other dietary factors may also contribute to improved cognition and prevention of cognitive disorders. Polyphenolic-rich foods are a further example that have been shown to have benefit, particularly in the context of aging.
Dietary interventions with polyphenolic-rich foods can improve neuronal and behavior deficits associated with aging
It is estimated that approximately 20% of the US total population will be older than 65 by the year 2050, which is almost double what it is today. 85 Additionally, the US is faced with an increasingly overweight/obese population that is at heightened risk for metabolic disorders, resulting in diabetes and cardiovascular disease, and concomitant behavioral impairment. Aging and metabolic dysregulation are both associated with numerous cognitive and motor deficits on tasks that require fine motor control, balance, short-term and long-term memory, or executive function. Studies in both humans and animal models have demonstrated that oxidative stress and inflammation, as well as impaired insulin resistance, are common features in cardio-metabolic and vascular disease, obesity, and age-related declines in cognitive and motor function. 86 Neuroinflammation occurs locally in the brain; however, peripheral inflammatory cells and circulating inflammatory mediators (e.g., cytokines) can also infiltrate the brain, and this occurs more readily as we age. 87 Therefore, strategies must be found to reduce oxidative and inflammatory vulnerability to age-related changes and reverse deficits in motor and cognitive function.
Targeting peripheral inflammation and insulin signaling could reduce insulin resistance and infiltration of inflammatory mediators into the brain and, as a result, reduce the incidence of a variety of age-related deficits. Studies have shown that plants, particularly colorful fruit or vegetable-bearing plants, contain polyphenolic compounds that have potent antioxidant and anti-inflammatory activities, 88 and increased fruit and vegetable intake has been associated with reduced fasting insulin levels. 89 Evidence is accumulating that consumption of these polyphenol-rich foods, particularly berry fruit, may be a strategy to forestall or even reverse age-related neuronal deficits resulting from neuroinflammation. 90 Recently this evidence has been extended to double-blind, placebo-controlled, randomized human intervention studies that have demonstrated that the consumption of flavonoid/polyphenols is associated with benefits to cognitive function. 91
Preclinical studies have led to the hypothesis that the key to reducing the incidence of age-related deficits in behavior is to alter the neuronal environment with polyphenolic-rich foods like berry fruit, such that neuroinflammation and oxidative stress, and the vulnerability to them, would be reduced. In early studies with animal models, crude blueberry (BB) or strawberry extracts significantly attenuated 92 and reversed 93 age-related motor and cognitive deficits in senescent rodents. BB supplementation also protected 9 month old C57Bl/6 mice against the damaging effects of consuming a high-fat diet. 94 Novel object recognition memory was impaired by the high-fat diet, but blueberry supplementation prevented recognition memory deficits in a time-dependent manner. Spatial memory, as measured by the Morris water maze, was also improved after 5 months on the diets. 94 Subsequent research suggested that berry fruit polyphenols may possess a multiplicity of actions in addition to their anti-inflammatory and antioxidant activities. 90 Additionally, the anthocyanins contained in blueberries have been shown to enter the brain, and their concentrations were correlated with cognitive performance. 95
Epidemiological studies that have focused on fruit and vegetable intake and cognitive function have also largely found that adequate consumption can prevent cognitive decline, while low intake is associated with increased cognitive decline. 85 Specifically, increased intake of blueberries and strawberries, as well as increased intakes of anthocyanidins and total flavanoids, were associated with slowing the rate of cognitive decline by up to 2.5 years. 96
The ability of berry fruit to protect against age-related cognitive decline has also been examined in a growing number of double-blind, placebo-controlled, randomized, human intervention studies. Thus, blueberry juice significantly improved word list recall and paired associate learning in older men and women with age-related memory decline that consumed it, relative to baseline, with paired associate learning also significantly improved relative to placebo controls. 97 A recent study 98 that measured similar cognitive tasks as those in the rodent studies, showed that freeze-dried blueberries (24 g/day, equivalent to one cup of fresh blueberries) for 90 days improved two measures of executive function in older adults (ages 60–75). Participants in the blueberry group showed significantly fewer repetition errors in the California Verbal Learning test as well as reduced switch cost on a task-switching test across study visits, relative to controls who consumed placebo powder. However, no improvement in gait or balance was observed following blueberry intake. 98 Finally, 12 weeks of blueberry concentrate supplementation improved brain perfusion, task-related activation, and cognitive function (i.e., working memory) in healthy older adults who consumed 30 mL blueberry concentrate providing 387 mg anthocyanidins. 99 These studies suggest that berry fruit might be an effective strategy to prevent, delay, or reverse cognitive dysfunction during aging.
Cognitive aging does not occur simultaneously across cognitive domains, with various domains peaking in early adulthood before reaching a plateau or declining. Therefore, interventions early in life may yield health benefits that are only measureable in later life. Blueberries have been shown to have positive cognitive benefits in two acute, cross-over designed studies in school-aged children (ages 7–10). The first study 100 showed that consumption of a flavonoid-rich blueberry (200 g) drink led to significantly better delayed word-list recall, compared to a matched vehicle group, on the Rey auditory-verbal learning test, suggesting more effective coding of memory items. However, there was no benefit of blueberry intervention on measures of attention, response inhibition, or visuospatial memory, and a negative impact on proactive interference. 100 The second study 100 by the same group examined cognition at baseline, and then 1.15, 3, and 6 h after consuming placebo (vehicle) or blueberry drinks containing 15 or 30 g freeze-dried wild blueberry (WBB) powder. Consumption of WBB powder improved recall at 1.15 h, improved delayed word recognition, which was sustained at each time point measured, and improved accuracy on a challenging interference task at 3 h. The best cognitive performance was seen after the 30 g dose, and particularly on those tasks with a higher cognitive demand. 100
As humans age, their ability to defend against the effects of oxidative stress and inflammation weakens, putting elderly people at increased risk for neuronal disease and degradation. Neuroprotective foods, such as berries and other dark-colored fruits, represent one way to protect aging brains against this damage by reducing inflammation and oxidative stress in the brain, thereby protecting against cognitive declines in aged populations.
This review has highlighted the latest advances in how foods and patterns of consumption at different times of development affect the brain, and the behavioral manifestations that may result from these effects. For example, early life overfeeding can permanently sensitize the brain’s neuroinflammatory response to challenging stimuli resulting in cognitive and immune dysfunctions throughout life. ES alters brain function, via metabolic and nutritional factors, to increase vulnerability to develop emotional and cognitive disorders. Long-term and short-term consumption of high saturated fatty foods during adulthood produces a sensitized inflammatory phenotype, via a glucocorticoid rise, in the hippocampus, leading to learning and memory vulnerabilities. Imbalance of omega-3 and omega-6 PUFA contribute to neurodevelopmental disorders by altering microglial activation resulting in abnormal formation of neuronal networks and activity. Finally, consumption of fruits and vegetables high in polyphenolics can prevent and reverse age-related cognitive deficits by lowering oxidative stress and inflammation. Collectively these data show that attention to dietary composition is important for lasting impact beyond the metabolic and highlight the promising likelihood that we may improve our cognition throughout life and into the aging period with simple dietary interventions. These data highlight the need for food industries and science, alike, to focus on research and development of nutritional strategies that are most appropriate to support our cognitive and emotional health; foods that are high in omega-3 PUFA and polyphenolics may be a promising place to start.
Data availability
No data sets were generated or analyzed during the current study.
Ng, M. et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384 , 766–781 (2014).
Article Google Scholar
Imamura, F. et al. Dietary quality among men and women in 187 countries in 1990 and 2010: a systematic assessment. Lancet Glob. Health 3 , e132–e142 (2015).
de Rooij, S. R., Wouters, H., Yonker, J. E., Painter, R. C. & Roseboom, T. J. Prenatal undernutrition and cognitive function in late adulthood. Proc. Natl. Acad. Sci. USA 107 , 16881–16886 (2010).
de Groot, R. H. et al. Prenatal famine exposure and cognition at age 59 years. Int. J. Epidemiol. 40 , 327–337 (2011).
Dabelea, D. et al. Intrauterine exposure to diabetes conveys risks for type 2 diabetes and obesity: a study of discordant sibships. Diabetes 49 , 2208–2211 (2000).
Article CAS Google Scholar
Boney, C. M., Verma, A., Tucker, R. & Vohr, B. R. Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics 115 , e290–296 (2005).
Ong, Z. Y. & Muhlhausler, B. S. Maternal “junk-food” feeding of rat dams alters food choices and development of the mesolimbic reward pathway in the offspring. FASEB. J. 25 , 2167–2179 (2011).
Gugusheff, J. R., Ong, Z. Y. & Muhlhausler, B. S. A maternal “junk-food” diet reduces sensitivity to the opioid antagonist naloxone in offspring postweaning. FASEB. J. 27 , 1275–1284 (2013).
Miller, A. A. & Spencer, S. J. Obesity and neuroinflammation: a pathway to cognitive impairment. Brain Behav. Immun. 42 , 10–21 (2014).
Drover, J., Hoffman, D. R., Castaneda, Y. S., Morale, S. E. & Birch, E. E. Three randomized controlled trials of early long-chain polyunsaturated fatty acid supplementation on means-end problem solving in 9-month-olds. Child Dev. 80 , 1376–1384 (2009).
Ng, S. F. et al. Chronic high-fat diet in fathers programs beta-cell dysfunction in female rat offspring. Nature 467 , 963–966 (2010).
Rivera, H. M., Christiansen, K. J. & Sullivan, E. L. The role of maternal obesity in the risk of neuropsychiatric disorders. Front. Neurosci. 9 , 194 (2015).
Bolton, J. L. & Bilbo, S. D. Developmental programming of brain and behavior by perinatal diet: focus on inflammatory mechanisms. Dialogues Clin. Neurosci. 16 , 307–320 (2014).
Google Scholar
Stefanidis, A. & Spencer, S. J. Effects of neonatal overfeeding on juvenile and adult feeding and energy expenditure in the rat. PLoS One 7 , e52130 (2012).
De Luca, S. N. et al. Early life overfeeding impairs spatial memory performance by reducing microglial sensitivity to learning. J. Neuroinflammation 13 , 112 (2016).
Jeon, B. T. et al. Resveratrol attenuates obesity-associated peripheral and central inflammation and improves memory deficit in mice fed a high-fat diet. Diabetes 61 , 1444–1454 (2012).
Lu, J. et al. Ursolic acid improves high fat diet-induced cognitive impairments by blocking endoplasmic reticulum stress and IkappaB kinase beta/nuclear factor-kappaB-mediated inflammatory pathways in mice. Brain Behav. Immun. 25 , 1658–1667 (2011).
Sobesky, J. L. et al. High-fat diet consumption disrupts memory and primes elevations in hippocampal IL-1beta, an effect that can be prevented with dietary reversal or IL-1 receptor antagonism. Brain Behav. Immun. 42 , 22–32 (2014).
Soares, E. et al. Spatial memory impairments in a prediabetic rat model. Neuroscience 250 , 565–577 (2013).
Di Benedetto, S., Muller, L., Wenger, E., Duzel, S. & Pawelec, G. Contribution of neuroinflammation and immunity to brain aging and the mitigating effects of physical and cognitive interventions. Neurosci. Biobehav. Rev. 75 , 114–128 (2017).
Dupret, D. et al. Spatial learning depends on both the addition and removal of new hippocampal neurons. PLoS Biol. 5 , e214 (2007).
Elmore, M. R. et al. Colony-stimulating factor 1 receptor signaling is necessary for microglia viability, unmasking a microglia progenitor cell in the adult brain. Neuron 82 , 380–397 (2014).
Heim, C., Newport, D. J., Mletzko, T., Miller, A. H. & Nemeroff, C. B. The link between childhood trauma and depression: insights from HPA axis studies in humans. Psychoneuroendocrinology 33 , 693–710 (2008).
Naninck, E. F. et al. Chronic early life stress alters developmental and adult neurogenesis and impairs cognitive function in mice. Hippocampus 25 , 309–328 (2015).
Naninck, E. F. et al. Early micronutrient supplementation protects against early stress-induced cognitive impairments. FASEB. J. 31 , 505–518 (2017).
Weaver, I. C. et al. Epigenetic programming by maternal behavior. Nat. Neurosci. 7 , 847–854 (2004).
Ivy, A. S. et al. Hippocampal dysfunction and cognitive impairments provoked by chronic early-life stress involve excessive activation of CRH receptors. J. Neurosci. 30 , 13005–13015 (2010).
Lucassen, P. J. et al. Perinatal programming of adult hippocampal structure and function; emerging roles of stress, nutrition and epigenetics. Trends Neurosci. 36 , 621–631 (2013).
Danese, A. & Tan, M. Childhood maltreatment and obesity: systematic review and meta-analysis. Mol. Psychiatry 19 , 544–554 (2014).
Maniam, J., Antoniadis, C. P., Wang, K. W. & Morris, M. J. Early life stress induced by limited nesting material produces metabolic resilience in response to a high-fat and high-sugar diet in male rats. Front. Endocrinol. 6 , 138 (2015).
Monk, C., Georgieff, M. K. & Osterholm, E. A. Research review: maternal prenatal distress and poor nutrition—mutually influencing risk factors affecting infant neurocognitive development. J. Child Psychol. Psychiatry 54 , 115–130 (2013).
Brown, A. S., van Os, J., Driessens, C., Hoek, H. W. & Susser, E. S. Further evidence of relation between prenatal famine and major affective disorder. Am. J. Psychiatry 157 , 190–195 (2000).
Ivy, A. S., Brunson, K. L., Sandman, C. & Baram, T. Z. Dysfunctional nurturing behavior in rat dams with limited access to nesting material: a clinically relevant model for early-life stress. Neuroscience 154 , 1132–1142 (2008).
Rice, C. J., Sandman, C. A., Lenjavi, M. R. & Baram, T. Z. A novel mouse model for acute and long-lasting consequences of early life stress. Endocrinology 149 , 4892–4900 (2008).
Pleasure, S. J., Collins, A. E. & Lowenstein, D. H. Unique expression patterns of cell fate molecules delineate sequential stages of dentate gyrus development. J. Neurosci. 20 , 6095–6105 (2000).
CAS Google Scholar
Oomen, C. A., Bekinschtein, P., Kent, B. A., Saksida, L. M. & Bussey, T. J. Adult hippocampal neurogenesis and its role in cognition. Wiley Interdiscip. Rev. Cogn. Sci. 5 , 573–587 (2014).
Korosi, A. et al. Early-life stress mediated modulation of adult neurogenesis and behavior. Behav. Brain Res. 227 , 400–409 (2012).
Hoeijmakers, L. et al. Early-life stress lastingly alters the neuroinflammatory response to amyloid pathology in an Alzheimer’s disease mouse model. Brain Behav. Immun. 63 , 160–175 (2017).
Yam, K. Y. et al. Exposure to chronic early-life stress lastingly alters the adipose tissue, the leptin system and changes the vulnerability to western-style diet later in life in mice. Psychoneuroendocrinology 77 , 186–195 (2017).
Yam, K. Y., Naninck, E. F., Schmidt, M. V., Lucassen, P. J. & Korosi, A. Early-life adversity programs emotional functions and the neuroendocrine stress system: the contribution of nutrition, metabolic hormones and epigenetic mechanisms. Stress 18 , 328–342 (2015).
Micha, R. et al. Global, regional, and national consumption levels of dietary fats and oils in 1990 and 2010: a systematic analysis including 266 country-specific nutrition surveys. BMJ 348 , g2272 (2014).
Fryar, C. D., Carroll, M. D. & Ogden, C. L. Prevalence of overweight, obesity, and extreme obesity among adults aged 20 and over: United States, 1960–1962 through 2013–2014. NCHS Data Brief , 1–6 (2016).
Thaler, J. P. et al. Obesity is associated with hypothalamic injury in rodents and humans. J. Clin. Invest. 122 , 153–162 (2012).
Beilharz, J. E., Maniam, J. & Morris, M. J. Short-term exposure to a diet high in fat and sugar, or liquid sugar, selectively impairs hippocampal-dependent memory, with differential impacts on inflammation. Behav. Brain Res. 306 , 1–7 (2016).
De Souza, C. T. et al. Consumption of a fat-rich diet activates a proinflammatory response and induces insulin resistance in the hypothalamus. Endocrinology 146 , 4192–4199 (2005).
Milanski, M. et al. Saturated fatty acids produce an inflammatory response predominantly through the activation of TLR4 signaling in hypothalamus: implications for the pathogenesis of obesity. J. Neurosci. 29 , 359–370 (2009).
Maric, T., Woodside, B. & Luheshi, G. N. The effects of dietary saturated fat on basal hypothalamic neuroinflammation in rats. Brain Behav. Immun. 36 , 35–45 (2014).
Almeida-Suhett, C. P., Graham, A., Chen, Y. & Deuster, P. Behavioral changes in male mice fed a high-fat diet are associated with IL-1beta expression in specific brain regions. Physiol. Behav. 169 , 130–140 (2017).
Tran, D. M. & Westbrook, R. F. A high-fat high-sugar diet-induced impairment in place-recognition memory is reversible and training-dependent. Appetite 110 , 61–71 (2017).
Boitard, C. et al. Impairment of hippocampal-dependent memory induced by juvenile high-fat diet intake is associated with enhanced hippocampal inflammation in rats. Brain Behav. Immun. 40 , 9–17 (2014).
Sobesky, J. L. et al. Glucocorticoids mediate short-term high-fat diet induction of neuroinflammatory priming, the NLRP3 inflammasome, and the danger signal HMGB1. eNeuro 3 , 1–17 (2016).
Holloway, C. J. et al. A high-fat diet impairs cardiac high-energy phosphate metabolism and cognitive function in healthy human subjects. Am. J. Clin. Nutr. 93 , 748–755 (2011).
Tantot, F. et al. The effect of high-fat diet consumption on appetitive instrumental behavior in rats. Appetite 108 , 203–211 (2017).
Barrientos, R. M., Kitt, M. M., Watkins, L. R. & Maier, S. F. Neuroinflammation in the normal aging hippocampus. Neuroscience 309 , 84–99 (2015).
Frank, M. G., Miguel, Z. D., Watkins, L. R. & Maier, S. F. Prior exposure to glucocorticoids sensitizes the neuroinflammatory and peripheral inflammatory responses to E. coli lipopolysaccharide. Brain Behav. Immun. 24 , 19–30 (2010).
Barrientos, R. M. et al. Greater glucocorticoid receptor activation in hippocampus of aged rats sensitizes microglia. Neurobiol. Aging 36 , 1483–1495 (2015).
Frank, M. G., Hershman, S. A., Weber, M. D., Watkins, L. R. & Maier, S. F. Chronic exposure to exogenous glucocorticoids primes microglia to pro-inflammatory stimuli and induces NLRP3 mRNA in the hippocampus. Psychoneuroendocrinology 40 , 191–200 (2014).
Bazinet, R. P. & Laye, S. Polyunsaturated fatty acids and their metabolites in brain function and disease. Nat. Rev. Neurosci. 15 , 771–785 (2014).
Joffre, C., Nadjar, A., Lebbadi, M., Calon, F. & Laye, S. n-3 LCPUFA improves cognition: the young, the old and the sick. Prostaglandins Leukot. Essent. Fat. Acids 91 , 1–20 (2014).
Joffre, C. et al. Modulation of brain PUFA content in different experimental models of mice. Prostaglandins Leukot. Essent. Fat. Acids 114 , 1–10 (2016).
Kitson, A. P., Stroud, C. K. & Stark, K. D. Elevated production of docosahexaenoic acid in females: potential molecular mechanisms. Lipids 45 , 209–224 (2010).
Nguyen, L. N. et al. Mfsd2a is a transporter for the essential omega-3 fatty acid docosahexaenoic acid. Nature 509 , 503–506 (2014).
Saunders, E. F. et al. Omega-3 and Omega-6 polyunsaturated fatty acids in bipolar disorder: a review of biomarker and treatment studies. J. Clin. Psychiatry 77 , e1301–e1308 (2016).
Yassine, H. N. et al. Association of docosahexaenoic acid supplementation with alzheimer disease stage in apolipoprotein E epsilon4 carriers: a review. JAMA. Neurol. 74 , 339–347 (2017).
Bozzatello, P., Brignolo, E., De Grandi, E. & Bellino, S. Supplementation with omega-3 fatty acids in psychiatric disorders: a review of literature data. J. Clin. Med. 5 , 1–43 (2016).
Rapaport, M. H. et al. Inflammation as a predictive biomarker for response to omega-3 fatty acids in major depressive disorder: a proof-of-concept study. Mol. Psychiatry 21 , 71–79 (2016).
Burke, J. E. & Dennis, E. A. Phospholipase A2 structure/function, mechanism, and signaling. J. Lipid Res. 50 Suppl, S237–242 (2009).
Serhan, C. N. Pro-resolving lipid mediators are leads for resolution physiology. Nature 510 , 92–101 (2014).
Bazan, N. G. The docosanoid neuroprotectin D1 induces homeostatic regulation of neuroinflammation and cell survival. Prostaglandins Leukot. Essent. Fat. Acids 88 , 127–129 (2013).
Rey, C. et al. Resolvin D1 and E1 promote resolution of inflammation in microglial cells in vitro. Brain Behav. Immun. 55 , 249–259 (2016).
Lukiw, W. J. & Bazan, N. G. Neuroinflammatory signaling upregulation in Alzheimer’s disease. Neurochem. Res. 25 , 1173–1184 (2000).
Zhu, M. et al. Pro-resolving lipid mediators improve neuronal survival and increase Abeta42 phagocytosis. Mol. Neurobiol. 53 , 2733–2749 (2016).
Freund-Levi, Y. et al. Effects of omega-3 fatty acids on inflammatory markers in cerebrospinal fluid and plasma in Alzheimer’s disease: the OmegAD study. Dement. Geriatr. Cogn. Disord. 27 , 481–490 (2009).
Yuki, D. et al. DHA-PC and PSD-95 decrease after loss of synaptophysin and before neuronal loss in patients with Alzheimer’s disease. Sci. Rep. 4 , 7130 (2014).
Hjorth, E. et al. Omega-3 fatty acids enhance phagocytosis of Alzheimer’s disease-related amyloid-beta42 by human microglia and decrease inflammatory markers. J. Alzheimers Dis. 35 , 697–713 (2013).
Hopperton, K. E., Trepanier, M. O., Giuliano, V. & Bazinet, R. P. Brain omega-3 polyunsaturated fatty acids modulate microglia cell number and morphology in response to intracerebroventricular amyloid-beta 1-40 in mice. J. Neuroinflammation 13 , 257 (2016).
Kim, H. Y. & Spector, A. A. Synaptamide, endocannabinoid-like derivative of docosahexaenoic acid with cannabinoid-independent function. Prostaglandins Leukot. Essent. Fat. Acids 88 , 121–125 (2013).
Alhouayek, M. & Muccioli, G. G. COX-2-derived endocannabinoid metabolites as novel inflammatory mediators. Trends Pharmacol. Sci. 35 , 284–292 (2014).
Marsicano, G. & Lutz, B. Neuromodulatory functions of the endocannabinoid system. J. Endocrinol. Invest. 29 , 27–46 (2006).
Stella, N. Cannabinoid and cannabinoid-like receptors in microglia, astrocytes, and astrocytomas. Glia 58 , 1017–1030 (2010).
Bosch-Bouju, C., Layé, S. Dietary Omega-6/Omega-3 and Endocannabinoids: Implications for Brain Health and Diseases in Cannabinoids in Health and Disease (ed Meccariello, R.) InTech. https://doi.org/10.5772/62498 (2016).
Lafourcade, M. et al. Nutritional omega-3 deficiency abolishes endocannabinoid-mediated neuronal functions. Nat. Neurosci. 14 , 345–350 (2011).
Thomazeau, A., Bosch-Bouju, C., Manzoni, O. & Laye, S. Nutritional n-3 PUFA deficiency abolishes endocannabinoid gating of hippocampal long-term potentiation. Cereb. Cortex 27 , 2571–2579 (2017).
Castillo, P. E., Younts, T. J., Chavez, A. E. & Hashimotodani, Y. Endocannabinoid signaling and synaptic function. Neuron 76 , 70–81 (2012).
Miller, M. G., Thangthaeng, N., Poulose, S. M. & Shukitt-Hale, B. Role of fruits, nuts, and vegetables in maintaining cognitive health. Exp. Gerontol. 94 , 24–28 (2016).
Panza, F. et al. Metabolic syndrome and cognitive impairment: current epidemiology and possible underlying mechanisms. J. Alzheimers Dis. 21 , 691–724 (2010).
McGeer, P. L. & McGeer, E. G. The inflammatory response system of brain: implications for therapy of Alzheimer and other neurodegenerative diseases. Brain Res. Brain Res. Rev. 21 , 195–218 (1995).
Stevenson, D. E. & Hurst, R. D. Polyphenolic phytochemicals—just antioxidants or much more? Cell. Mol. Life Sci. 64 , 2900–2916 (2007).
Cavallo, D. N., Horino, M. & McCarthy, W. J. Adult intake of minimally processed fruits and vegetables: associations with cardiometabolic disease risk factors. J. Acad. Nutr. Diet. 116 , 1387–1394 (2016).
Miller, M. G. & Shukitt-Hale, B. Berry fruit enhances beneficial signaling in the brain. J. Agric. Food Chem. 60 , 5709–5715 (2012).
Lamport, D. J., Saunders, C., Butler, L. T. & Spencer, J. P. Fruits, vegetables, 100% juices, and cognitive function. Nutr. Rev. 72 , 774–789 (2014).
Joseph, J. A. et al. Long-term dietary strawberry, spinach, or vitamin E supplementation retards the onset of age-related neuronal signal-transduction and cognitive behavioral deficits. J. Neurosci. 18 , 8047–8055 (1998).
Joseph, J. A. et al. Reversals of age-related declines in neuronal signal transduction, cognitive, and motor behavioral deficits with blueberry, spinach, or strawberry dietary supplementation. J. Neurosci. 19 , 8114–8121 (1999).
Carey, A. N., Gomes, S. M. & Shukitt-Hale, B. Blueberry supplementation improves memory in middle-aged mice fed a high-fat diet. J. Agric. Food Chem. 62 , 3972–3978 (2014).
Andres-Lacueva, C. et al. Anthocyanins in aged blueberry-fed rats are found centrally and may enhance memory. Nutr. Neurosci. 8 , 111–120 (2005).
Devore, E. E., Kang, J. H., Breteler, M. M. & Grodstein, F. Dietary intakes of berries and flavonoids in relation to cognitive decline. Ann. Neurol. 72 , 135–143 (2012).
Krikorian, R. et al. Blueberry supplementation improves memory in older adults. J. Agric. Food Chem. 58 , 3996–4000 (2010).
Miller, M. G., Hamilton, D. A., Joseph, J. A. & Shukitt-Hale, B. Dietary blueberry improves cognition among older adults in a randomized, double-blind, placebo-controlled trial. Eur. J. Nutr. https://doi.org/10.1007/s00394-017-1400-8 (2017).
Bowtell, J. L., Aboo-Bakkar, Z., Conway, M., Adlam, A. R. & Fulford, J. Enhanced task related brain activation and resting perfusion in healthy older adults after chronic blueberry supplementation. Appl. Physiol. Nutr. Metabol. 42 , 773–779 (2017).
Whyte, A. R. & Williams, C. M. Effects of a single dose of a flavonoid-rich blueberry drink on memory in 8 to 10 y old children. Nutrition 31 , 531–534 (2015).
Download references
Acknowledgements
This work was supported by funding from by a National Health and Medical Research Council Career Development Fellowship, a Club Melbourne Fellowship and a Brain Foundation Research Gift to S.J.S., an NWO Meervoud and NWO Food Cognition and Behavior (NWO-FCB), JPI-Nutricog to A.K., and funding from the USDA Intramural, U.S. Highbush Blueberry Council, and California Strawberry Commission to B.SH.
Author information
Authors and affiliations.
School of Health and Biomedical Sciences, RMIT University, Melbourne, VIC, 3788, Australia
Sarah J. Spencer
Swammerdam Institute for Life Sciences, Center for Neuroscience, University of Amsterdam, Amsterdam, 1098 XH, Netherlands
Aniko Korosi
Nutrition et Neurobiologie Intégrée, INRA, Bordeaux University, Bordeaux, UMR1286, France
Sophie Layé
USDA-ARS, Human Nutrition Research Center On Aging at Tufts University, Boston, MA, 02111-1524, USA
Barbara Shukitt-Hale
Department of Psychology & Neuroscience, and Center for Neuroscience, University of Colorado, Campus Box 345, Boulder, CO, 80309-0345, USA
Ruth M. Barrientos
You can also search for this author in PubMed Google Scholar
Contributions
All authors made substantial contributions to the design and conception of the work, drafting it, revising it critically for important intellectual content. All authors approve the completed version.
Corresponding author
Correspondence to Sarah J. Spencer .
Ethics declarations
Competing interests.
The authors declare that they have no competing financial interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Spencer, S.J., Korosi, A., Layé, S. et al. Food for thought: how nutrition impacts cognition and emotion. npj Sci Food 1 , 7 (2017). https://doi.org/10.1038/s41538-017-0008-y
Download citation
Received : 30 April 2017
Revised : 24 July 2017
Accepted : 10 August 2017
Published : 06 December 2017
DOI : https://doi.org/10.1038/s41538-017-0008-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Identifying distinct subtypes of mother-to-infant bonding using latent profile analysis in a nationwide japanese study.
- Kosuke Hagiwara
- Takahiro Tabuchi
Archives of Women's Mental Health (2024)
Nutritional strategies cause memory damage and alter biochemical parameters without causing neuroinflammation
- Keila Rufatto de Souza
- Nicole Alessandra Engel
- Gislaine Tezza Rezin
Metabolic Brain Disease (2024)
Exploring the effects of health behaviors and mental health on students’ academic achievement: a cross-sectional study on lebanese university students
- Dalal Hammoudi Halat
- Souheil Hallit
- Mohamad Rahal
BMC Public Health (2023)
Human nutritional relevance and suggested nutritional guidelines for vitamin A5/X and provitamin A5/X
- Torsten Bohn
- Julian Hellman-Regen
Nutrition & Metabolism (2023)
Intestinal gluconeogenesis: metabolic benefits make sense in the light of evolution
- Amandine Gautier-Stein
- Gilles Mithieux
Nature Reviews Gastroenterology & Hepatology (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

Critical Thinking in Mental Health
So what is critical thinking? Basically it is just thinking about the evidence before you and measuring the likelihood of it being true or false, or partly true or partly false. There is even a Foundation and Center for Critical Thinking , a Critical Thinking Company , and a massive amount of websites with “official” definitions.
Critical thinking is discussed in academics at all educational levels, although because of varying definitions some don’t support the concept. In general, however, being able to critically think about new information is a good skill, especially as we get more and more inundated with information in our world.
When I am teaching my students about critical thinking I always focus on it as it relates to the mental health of their future clients. There is so much information out there that gets presented to mental health professionals as truth that if we aren’t good at critical thinking we could be putting our patients at risk. I have seen it before, where a therapist tries a “new” approach to treatment that is later discovered to be problematic.
I share this because as I finish up my first month of blogging for this site I realized that as much as I enjoy sharing new research, it is important to note that research is ever changing in the mental health world, and all new ideas and information needs to be approached with caution.
If you needed to see a therapist I would advocate you ask about treatment modalities, especially if specific techniques are being used. For example, sometimes I just let my client talk because that is what they need – I don’t consider that a modality itself. But if I felt that client would benefit from specific forms of cognitive-behavioral therapy I would share specific information about it, so they could look into it further if they wanted. Not all therapists think like I do though. So protect yourself – be a critical thinker when seeking therapy to ensure techniques used are based on actual evidence. It is the only way I would seek therapy.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- World Psychiatry
- v.18(2); 2019 Jun
Mental illness and well‐being: an affect regulation perspective
James j. gross.
1 Department of Psychology, Stanford University, Stanford, CA, USA
Helen Uusberg
2 Institute of Psychology, University of Tartu, Tartu, Estonia
Andero Uusberg
Mental health crucially depends upon affective states such as emotions, stress responses, impulses and moods. These states shape how we think, feel and behave. Often, they support adaptive functioning. At other times, however, they can become detrimental to mental health via maladaptive affect generation processes and/or maladaptive affect regulation processes. Here, we present an integrative framework for considering the role of affect generation and regulation in mental illness and well‐being. Our model views affect generation as an iterative cycle of attending to, appraising and responding to situations. It views affect regulation as an iterative series of decisions aimed at altering affect generation. Affect regulation decisions include identifying what, if anything, should be changed about affect, selecting where to intervene in the affect generation cycle, choosing how to implement this intervention, and monitoring the regulation attempt to decide whether to maintain, switch or stop it. Difficulties with these decisions, often arising from biased inputs to them, can contribute to manifestations of mental illness such as clinical symptoms, syndromes and disorders. The model has a number of implications for clinical assessment and treatment. Specifically, it offers a common set of concepts for characterizing different affective states; it highlights interactions between affect generation and affect regulation; it identifies assessment and treatment targets among the component processes of affect regulation; and it is applicable to prevention and treatment of mental illness as well as to promotion and restoration of psychological well‐being.
Someone in good mental health enjoys not only freedom from mental illness but also substantial psychological well‐being. As the World Health Organization puts it, “mental health is a state of well‐being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community” 1 .
These characteristics of mental health depend, among other things, upon affective states such as emotions, stress responses, impulses and moods. An instance of affect can be viewed as more or less healthy, depending on whether its intensity, duration, frequency or type facilitates or threatens mental health in a given context 2 , 3 . For example, becoming a bit anxious before a job interview can be healthy when it improves motivation and performance. Intense anxiety, by contrast, can be unhealthy when it impairs performance and contributes to avoidance of future social challenges.
Some form of unhealthy affect can be found among the defining features of 40 to 75% of mental disorders 2 , 4 . It is therefore important to understand how affect becomes unhealthy, and what can be done to prevent or treat unhealthy affect. These questions have long been of interest for psychology and psychiatry 5 . To mention only a few major lines of inquiry, the psychodynamic tradition has related affect to contests between desires and constraints 6 ; the stress and coping tradition has elucidated cognitive antecedents and physiological consequences of affect 7 , 8 ; and the affective neuroscience tradition has revealed some of the brain mechanisms underlying affective behaviors 9 , 10 , 11 .
The diversity of literature on affect and mental health has resulted in a large number of poorly integrated accounts. For instance, accounts of affect in mental illness 12 tend to be separate from accounts of affect in well‐being 13 . Separate accounts can also be found for similar affective phenomena in different mental illnesses 14 . Adding to the complexity, different accounts often operate on different levels of analysis, from neurochemical to psychosocial. The fragmented set of explanations for the role of affect in mental health makes it difficult for practitioners and researchers to conceptualize individual cases; to analyze transdiagnostic mechanisms; and to integrate advances from ongoing research.
One way to address these limitations is to construct integrative frameworks that explain different kinds of affect across mental illness as well as well‐being. When seeking to understand how unhealthy affect arises, it is important to realize that, once generated , an emotion, a stress response, an impulse or a mood need not continue to dominate behavior, because people routinely use affect regulation to change these affective states 8 , 15 , 16 , 17 , 18 , 19 , 20 , 21 . Thus, unhealthy affect can result from problematic affect generation, problematic affect regulation, or some combination of the two.
Unhealthy affect may be said to be due to affect regulation failure when affect regulation is not successfully engaged to counteract maladaptive affect generation. Unhealthy affect may be said to be due to affect misregulation when affect regulation aggravates matters by changing affect in a maladaptive direction. Both affect regulation failure and affect misregulation can increase the risk of mental illness as well as hinder psychological well‐being. Conversely, adaptive affect regulation can prevent, reverse or alleviate mental illness as well as promote well‐being.
In this paper, we offer an integrative framework for thinking about the interplay between affect generation and affect regulation in mental health. We focus primarily on mental illness, but the principles we discuss are equally relevant for psychological well‐being. We also focus primarily on affect regulation but, in order to understand how affect can be regulated, we also need to consider how affect is generated.
In the first two sections of the paper, we present the process model of affect regulation, an integrative framework that views affect generation as a four‐stage process that can be altered by another four‐stage process of affect regulation 15 , 22 , 23 . In the third section of the paper, we use this framework to identify affect regulation difficulties that contribute to mental illnesses, drawing examples from a variety of symptoms, syndromes and disorders. In the final section, we consider several implications of the process model of affect regulation for clinical assessment and treatment.
AFFECT GENERATION
We use “affect” as an umbrella term to denote emotions such as anxiety or joy; stress responses such as feeling threatened or feeling challenged; impulses such as an urge to flee or to have a drink; and moods such as depression or elation. Despite their differences, what these diverse processes have in common is that they all involve valuation – a good‐for‐me vs. bad‐for‐me distinction – that can shape behavior 15 , 24 , 25 , 26 , 27 . For instance, anxiety, feeling threatened, an urge to flee, and depression all signal that something is unpleasant and worth avoiding. Joy, feeling challenged, an urge to drink, and elation all signal that something is pleasant and worth approaching. Valuation reflects what a situation has to offer in relation to what the individual values, needs or wants. The function of affective states is therefore to shape behavior in accordance with the relationship between situation and motivational concerns.
Given their shared function, affective states can be analyzed using common concepts. Following a cybernetic approach 15 , 28 , 29 , 30 , we view affect as a series of iterative cycles comprising four stages: a) a situation that can be experienced or imagined; b) attention that shapes how the situation is perceived; c) appraisal of the situation in light of motivational concerns; and d) a response to the situation that can entail changes in subjective experience, physiology, and/or facial or whole‐body behavior (see Figure 1 ). For instance, an emotion of anxiety may arise when a person experiences or imagines a job interview (situation); pays attention to what could go wrong (attention); appraises the situation as threatening (appraisal); and feels anxious, starts to sweat, and wishes to flee (response).

Affect generation. Different affective states such as emotions, stress responses, impulses and moods can be viewed as iterative cycles of attending to, appraising and responding to situations.
The affective responses generated on one iteration of this feedback loop may become part of the situation stage of a subsequent iteration. For instance, the person may now realize that he is being interviewed while anxious and perspiring (situation), fixate on increased chances of failure (attention), appraise the situation as even more threatening (appraisal), and experience even stronger anxiety (response). Successive iterations of the affect generation loop can produce increasingly selective attention, elaborate appraisals, and specific responses.
We suggest that the same four iterative stages are involved in different kinds of affective states, although the stages can differ in their automaticity, specificity, duration, and other features. One way to organize different affective states within this framework is to place them on a continuum based on how many affect generation stages are generally part of the conscious experience of the given affective state.
At one end of this continuum are emotions, where all four stages are generally part of the experience. Emotions such as anxiety or joy tend to involve strong feelings directed at a situation that commands attention and is at least in part consciously appraised 27 , 31 .
At the other end of the continuum are moods such as depression or elation, that tend to be experienced as diffuse feelings and action tendencies (i.e., only the response stage). We argue that the remaining affect generation stages play a role in moods outside of conscious awareness. Thus, moods tend to relate to situations that have been selectively perceived and appraised largely outside of awareness 32 , 33 .
Between emotions and moods in the continuum are stress responses and impulses. Stress responses, such as feeling threatened or feeling challenged 8 , 34 , resemble emotions in that the attention, appraisal and response stages are usually part of the experience. However, instead of a single identifiable situation, these experiences revolve around broader circumstances, such as a divorce or a new job, that span several specific situations.
Impulses, such as an urge to flee or to have a drink, can be viewed as affective states experienced as a constellation of the response and the situation stages. Impulses can feel almost like reflexes – strong action tendencies (i.e., response stage) elicited by some threat or opportunity (i.e., situation stage) 17 . We argue that the intermediate stages of selectively perceiving and appraising the situation are often operative in impulses, albeit outside awareness.
The four‐stage model of affect generation is a flexible way to appreciate both commonalities and differences among different kinds of affective states. Importantly for current purposes, the model also suggests that unhealthy affect can be traced back to maladaptive unfolding of one or more of the four affect generation stages. Sometimes, unhealthy affect arises simply due to a maladaptive situation, such as being a victim of violence. When unhealthy affect arises from otherwise adaptive situations, however, it may be because of maladaptive unfolding of attention, appraisal or response stages of affect generation. For instance, the mental health consequences of maladaptive attention are illustrated by the role of attention biases in mood and anxiety disorders 35 , 36 . The consequences of maladaptive appraisal are illustrated by the role of interpretation biases in people with depressive symptoms 37 . The consequences of maladaptive affective responses are illustrated by the role of low physiological reactivity in externalizing syndromes such as sociopathy 38 .
Maladaptive affect generation is therefore an important part of a comprehensive account of unhealthy affect. However, in this paper, our primary focus is affect regulation. This is because maladaptive affect generation manifests in unhealthy affect mostly when affect regulation fails to neutralize – or even further aggravates – the maladaptive affect.
AFFECT REGULATION
Affect regulation involves intentional (but not necessarily conscious) attempts to change the intensity, duration, frequency or type of current or anticipated affect 39 . We focus in this paper on self‐generated or intrinsic affect regulation, which can be distinguished from other‐generated or extrinsic affect regulation 40 , 41 . The latter – which involves one person's attempt to regulate the affective states of another person – is also important for mental health, but falls beyond the scope of this paper.
Mirroring the four kinds of affective states distinguished earlier, we may distinguish four kinds of affect regulation: a) emotion regulation 15 , 16 , 42 ; b) regulation of stress, i.e. coping 8 , 43 ; c) regulation of impulses, i.e. self‐regulation 17 , 44 ; and d) mood regulation 18 , 45 . Even though the type of affect targeted by regulation can be important to distinguish, our analysis of common mechanisms of affect generation suggests that there are also common mechanisms of affect regulation.
The process model of affect regulation highlights these shared mechanisms by addressing two fundamental questions: a) how can affect be regulated (strategies), and b) what processes underlie affect regulation (stages).
Affect regulation strategies
To understand how affect can be regulated, it is useful to return to the four stages of the affect generation loop outlined in Figure 1 . Given the stages of situation, attention, appraisal and response, we can distinguish four families of affect regulation strategies, based on which affect generation stage they primarily influence (see Figure 2 ).

Affect regulation strategies. Four families of affect regulation strategies can be distinguished based on which stage of affect generation they primarily seek to alter.
Situational strategies seek to alter affect generation at the situation stage, by selecting which situations are encountered ( situation selection ) or modifying what is going on in them ( situation modification ) 44 . For instance, people wishing to lift their depressed mood may call a friend (situation selection) or guide an already ongoing conversation to uplifting topics (situation modification).
Attentional strategies seek to alter affect generation at the attention stage, by changing what aspects of the situation are attended to 46 . For instance, the person experiencing depressed mood may distract himself from negative thoughts by diverting his attention to a game such as Tetris.
Cognitive strategies seek to alter affect generation at the appraisal stage, by modifying how the situation is viewed in light of goals, values, and other motivational concerns 47 . For instance, depressed mood could be fought off by considering how things are not as bad as they initially seemed.
Finally, response modulation strategies seek to alter affect at the response stage, by counteracting the affect‐related experiential, behavioral or physiological changes. For instance, the person experiencing depressed mood may prepare a cup of coffee to energize his body.
In addition to mood regulation, the same strategy families have been found to be relevant for regulating emotions 42 , stress 22 as well as impulses 44 , 48 .
Each of the four broad ways of changing affect can be effective, but each has different costs and benefits 49 , 50 . For instance, strategies that intervene early in the affect generation cycle can provide powerful relief from the affective state 51 , but this may come at the cost of limited learning 52 , 53 . As researchers have identified different costs and benefits of regulation strategies, it has become clear that adaptive affect regulation requires matching strategies to the characteristics of the affect being regulated, the individual, and the current context 54 , 55 , 56 . For instance, in a context where a frustrating situation can be improved, it is sensible to try to change the situation rather than to use cognitive strategies to change how the situation is appraised. By contrast, in a context where nothing much could be done to improve the situation, it is sensible to use cognitive rather than situational strategies 57 , 58 , 59 .
Affect regulation stages
If deciding how to best regulate affect appears such a complex task, how is it accomplished? The process model of affect regulation addresses this question by envisioning a series of four stages: identification, selection, implementation and monitoring (see Figure 3 ). Each stage can be thought of as a decision that the person makes, consciously or otherwise 60 , 61 . Returning to the example of the person experiencing depressed mood, what decisions does he need to make to regulate his mood?

Affect regulation stages. Affect regulation consist of key decisions that people make, consciously or otherwise, during four stages. At the identification stage, people decide what, if anything, should change about affect. At the selection stage, they decide which affect regulation strategy to use in service of that goal. At the implementation stage, they decide which actions to take as part of the chosen strategy to alter the affect generation process. The monitoring stage consists of iterative updates to the identification, selection and implementation decisions that amounts to a separate decision about whether ongoing efforts should be maintained, switched or stopped.
First, at the identification stage, he needs to decide that his current mood should be improved. This decision then activates the selection stage, where he needs to decide which affect regulation strategy to use (i.e., where to intervene in the affect generation cycle). For instance, he may select an attentional strategy to keep his mind off ruminative thoughts. Strategy selection triggers the implementation stage, where the person needs to decide which specific actions to take. For instance, he may play a game of Tetris.
As the chosen actions intervene in affect generation, all three decisions may need to be updated – whether the affect continues to require regulation, whether an attentional strategy continues to be the best strategy, and whether playing Tetris continues to be the best course of action. The continued iteration of the three decisions can be thought of as a separate monitoring stage of affect regulation, where the person needs to decide whether to maintain, switch or stop the ongoing affect regulation attempt.
To better understand the identification, selection, implementation and monitoring stages, it is helpful to consider what information is processed to reach the decisions required at each stage. The process model of affect regulation suggests that each stage makes use of two main inputs, and we now turn to describing the role that these inputs play in each of the four stages.
The identification decision of what, if anything, should change about affect (i.e., what is the regulation goal) relies on: a) a representation of the current affective state together with alternative states, and b) the evaluation of the costs and benefits of these states in the given context.
The first input to the identification decision thus requires representing ongoing affective states together with other states that the person could experience in the given situation. The importance of this input is illustrated by the finding that people who are good at detecting and labelling their affective states tend to also be good at affect regulation 62 , 63 .
The second input to the identification decision consists of the evaluation of the current and alternative affective states based on their costs and benefits. Most of the time, people evaluate affective states in light of the hedonic motive to increase pleasant feelings and decrease unpleasant feelings. However, people can also make counter‐hedonic (i.e., instrumental) evaluations, for instance when they wish to be angrier than they currently are because they believe that this will help them negotiate 64 .
When the identification stage is working well, the person detects the current affective state together with alternatives, evaluates them appropriately, and decides (consciously or otherwise) what, if anything, should change about the current affective state.
A decision to change affect triggers the selection stage, at which point the person decides where to intervene in affect generation (i.e., which regulation strategy to use). The selection decision relies on: a) a representation of available regulation strategies, and b) the evaluation of the costs and benefits of these strategies in the given context.
The availability of strategies can vary between situations as well as individuals. For instance, cognitive strategies are more likely to be considered in situations that have multiple interpretations 65 . Different individuals may consider different strategies based on their skills and abilities. For instance, attentional strategies work better for people with relatively high working memory capacity 66 , suggesting that they are more likely to consider these strategies as a viable regulation option.
The second input to the selection decision is the evaluation of costs and benefits of available strategies 67 . One major benefit of each available strategy is its expected efficacy to change affect. For instance, when attempting to downregulate intense emotions, people tend to prefer distraction (an attentional strategy) over reappraisal (a cognitive strategy), because the former is believed to be more effective 67 . Some of the major costs include the time and effort needed to use the strategy 68 . Other costs and benefits, more specific to different strategies, individuals and contexts, also help to shape the eventual choice of strategy.
When the selection stage is working well, the person represents available strategies, evaluates them appropriately, and decides which regulation strategy to use.
The selection decision triggers the implementation stage, where the person decides how to enact the selected strategy in the given context. This stage is needed because the broad strategies of intervening at one of the four stages of affect generation can be enacted in different ways 69 , sometimes referred to as regulation tactics. For instance, having made an identification decision to lift depressed mood, and a selection decision to rely on attentional strategies, the person may decide to play Tetris as a way to get his mind off his negative thoughts. Such an implementation decision relies on: a) a representation of different actions afforded by the situation, and b) the evaluation of the costs and benefits of these actions in the given context.
The implementation stage is where the regulation process reaches its target, as specific mental or physical actions impact the affect generation process (see Figure 3 ). For instance, playing Tetris diverts cognitive resources away from the attention stage involved in generating depressed mood.
When the implementation stage is working well, the person represents actions afforded by the specific context, evaluates them appropriately, and decides how to enact the regulation attempt.
The identification, implementation and selection decisions form an iterative cycle. As the strategy selected to serve the identified regulation goal is implemented , each of these decisions may need to be updated to mirror changes in the regulated affect as well as in the broader context. Iterative updates to the affect regulation decisions can be viewed as a separate monitoring stage, involving a decision to either maintain, switch or stop the regulation attempt. Inputs to this decision include: a) changes in affect, which can be spontaneous as well as caused by ongoing regulation, and b) changes in context.
As long as the regulation attempt continues to produce desired changes to affect, and the context also does not change substantially, the person can maintain regulation by relying on the latest identification, selection and implementation decisions (e.g., play Tetris to fend off rumination in order to lift depressed mood). However, if affect resists change, or changes in undesired ways, the chosen implementation, strategy or regulation goal can be switched , or the regulation attempt can be stopped altogether. Switching or stopping may also be mandated by a change in context, such as when a friend calls in the middle of the Tetris game.
To be adaptive, affect regulation should respond with optimal flexibility to changes in affect as well as in context 43 , 55 . Not enough flexibility can lead to overuse of certain affect regulation behaviors, whereas too much flexibility can lead to lack of persistence.
When the monitoring stage is working well, the person appropriately represents ongoing changes in affect as well as in context, and decides to maintain, switch or stop regulation accordingly.

MALADAPTIVE AFFECT REGULATION AND MENTAL ILLNESS
The process model of affect regulation outlined in the previous sections can be helpful for considering how maladaptive affect regulation can contribute to mental illness. The identification, selection, implementation and monitoring decisions can be considered maladaptive when they are misaligned with the targeted affective state, the current motives of the person, and/or contextual demands 54 , 55 , 56 . In this section, we consider how each of these decisions can become maladaptive. We use selective examples of manifestations of mental illness such as different symptoms, syndromes and disorders. Note that, even when we discuss a particular mechanism in relation to a particular manifestation, we do not intend to imply that a given manifestation could not be related to other mechanisms nor that a given mechanism could not be involved in other manifestations of mental illness.
Identification difficulties
Unhealthy affect may arise from the identification stage of affect regulation when the decision of what, if anything, should change about an affective state is maladaptive. This can happen when a person encounters difficulty with at least one of the inputs to the identification decision, i.e., by misrepresenting affective states and/or misevaluating their costs and benefits.
The first kind of difficulty is characteristic of individuals high on trait alexithymia, who struggle to attend to and accurately identify their affective experiences 70 . Compared to healthy controls, these individuals have been found to engage in maladaptive affect regulation patterns 71 which may arise from the low granularity with which they represent affect. Alexithymia is also common among individuals with mental illnesses such as autism spectrum disorder 72 or eating disorders 73 , suggesting that the unhealthy affect characterizing these mental illnesses may also arise in part from misrepresented affective states.
The second difficulty associated with the identification stage involves misevaluation of the costs and benefits of either the current affective state or alternative states that could be experienced. For example, people with panic disorder tend to overestimate the costs of current anxiety 74 . They may interpret a normal anxiety‐related increase in heart rate as a sign of imminent heart failure, or anxiety‐related thoughts as a sign of imminent loss of their grip on reality. Such overestimation of costs of affect can produce a maladaptive identification decision to launch an unnecessary regulation attempt. In addition to costs, people can also misestimate the benefits of affective states. For instance, individuals with bipolar disorder often choose not to downregulate maladaptive positive affect, even though they are able to do so when instructed 75 . One reason may be that individuals with bipolar disorder overvalue the hedonic benefits of positive affective states at the expense of the costs of these states as well as the benefits of alternative states 76 .
Selection difficulties
Unhealthy affect may arise from the selection stage of affect regulation when the decision about which regulation strategy to use in order to accomplish the regulation goal is maladaptive. This can happen when a person encounters difficulty with at least one of the inputs to this decision, i.e., by misrepresenting available strategy options and/or misevaluating the costs and benefits of these strategies.
One reason for misrepresenting available strategies may be that the person has limited skills or experiences with different strategies. For instance, people with alcohol use disorder may struggle to consider strategies other than consuming alcohol, which they are most familiar with 77 . A similar limitation may characterize individuals suffering from binge eating disorder, who often engage in unhealthy eating patterns for affect regulatory purposes 78 .
Another way the selection stage may contribute to unhealthy affect is via difficulties with evaluating the costs and benefits of different strategies. Many mental illnesses are associated with misevaluation of maladaptive regulation strategies. For example, engagement in non‐suicidal self‐injury relies in part on the evaluation of this costly behavior as an effective affect regulation strategy 79 , 80 . People with generalized anxiety disorder meanwhile view worry, another strategy with negative consequences, as productive (e.g., “Worrying helps me to be prepared and avoid adversities”) or as an indicator of good character (e.g., “Worrying means that I care”) 83 .
Difficulties with the cost‐benefit analysis of strategy options may also arise from more general decision biases. For instance, a broad range of mental illnesses are associated with amplified temporal discounting, whereby immediate outcomes are overvalued relative to long‐term outcomes even more than in healthy populations 81 . Amplified discounting can bias affect regulation strategy selection towards underestimating long‐term costs and benefits relative to short‐term ones. For instance, people with social anxiety disorder tend to choose behavioral avoidance to reduce anxiety despite it severely restricting social or professional outlooks for the future 82 .
Implementation difficulties
Unhealthy affect may arise from the implementation stage of affect regulation when the decision about how to enact the selected strategy in a given situation is maladaptive. This can happen when a person encounters difficulty with at least one of the inputs to this decision, i.e., by misrepresenting available affordances for action and/or misevaluating their costs and benefits.
The first difficulty may arise when a person fails to consider action affordances beyond obvious ones suggested by habit and the environment. For instance, someone looking for ways to implement a situational strategy for increasing excitement may fail to consider options beyond watching the TV that happens to be in the room. Detecting less obvious action affordances often requires cognitive control 84 , a set of processes that tends to be impaired across a range of mental illnesses 85 . Cognitive control impairments are particularly relevant in attention‐deficit/hyperactivity disorder (ADHD) 86 , which is also characterized by maladaptive affect regulation 87 . Our analysis suggests that maladaptive affect regulation in ADHD may stem, among other pathways, from difficulties to detect less obvious regulation tactics.
Another difficulty encountered at the implementation stage is the misevaluation of costs and benefits of different action affordances. This suggests that mental illnesses that impair predictions about action outcomes, such as major depressive disorder 88 , 89 , may contribute to maladaptive affect regulation by making it harder to appropriately evaluate action affordances even if they are detected. For instance, a person may come up with more ways than watching TV to implement an attentional strategy to feel more excited, but then fail to consider some of their outcomes, leading to a maladaptive choice. According to the present framework, one mechanism through which affect regulation becomes maladaptive in people with depressive symptoms 90 may therefore involve misevaluation of the action affordances that have been detected during the affect regulation process.
Monitoring difficulties
Unhealthy affect may arise from the monitoring stage of affect regulation, when the decision to maintain, switch or stop regulation is maladaptive. This can happen when the person encounters difficulties with at least one of the inputs to this decision, i.e., by misrepresenting changes to the regulated affect and/or to the relevant context. As the consequences of these difficulties are quite similar, we will not distinguish between them. Instead, we consider two directions of misrepresentations – under‐representing changes in affect or context that contributes to insufficient regulation flexibility, and over‐representing changes in affect or context that contributes to too high regulation flexibility 55 .
Insufficient flexibility can lead to unnecessary maintenance of regulation efforts that have already succeeded or are unlikely to succeed. Such inertia in regulation has been observed for numerous mental illnesses. For example, people with generalized anxiety disorder continue to worry despite it elevating anxiety and being cognitively costly 91 , 92 . Similarly, people with major depressive disorder continue to ruminate despite it increasing rather than decreasing depressed mood 93 .
At the other extreme, the monitoring decision can become overly flexible when changes in affect or context are over‐represented. This difficulty can manifest in premature switches between strategies and their implementation before they have had a chance to become effective, or premature stopping of regulation altogether 55 . For instance, borderline personality disorder is characterized both by frequent shifts in affective states 94 as well as high levels of impulsivity 95 . This suggests that one reason for the affective lability in individuals suffering from borderline personality disorder may be insufficient persistence in applying affect regulation, i.e. overly high affect regulation flexibility.
IMPLICATIONS FOR ASSESSMENT AND TREATMENT
Assessment and treatment of unhealthy affect is central to a number of psychotherapeutic approaches, including cognitive‐behavioral therapy 96 , dialectical‐behavioral therapy 97 , acceptance and mindfulness‐based interventions 98 , 99 , 100 , 101 , emotion‐focused therapy 102 , affect regulation training 103 , and emotion regulation therapy 104 . The present framework complements these approaches by offering four broad insights that have implications for clinical assessment as well as treatment.
First, the framework suggests that problems with different affective states, such as emotions, stress responses, impulses and moods, can be analyzed in common terms. Second, unhealthy affect usually arises from some combination of maladaptive affect generation and maladaptive affect regulation. Third, maladaptive affect regulation can arise from identification, selection, implementation and monitoring decisions. Finally, affective processes are equally relevant for mental illness and psychological well‐being. In this final section, we briefly discuss the assessment and treatment implications of each of these insights.
Common concepts for different affective states
Emotions, stress responses, impulses and moods have often been studied as separate phenomena, leading to separate assessment instruments and treatment approaches. Without denying instances where such distinctions are useful, the process model of affect regulation suggests that is also reasonable to focus on the similarities rather than differences between affective states.
The framework highlights the iterative stages of situation, attention, appraisal and response, and the ways to regulate them, as a set of concepts that are sufficiently broad to capture different affective states. For instance, take a problematic affect such as generalized anxiety, that is experienced as a diffuse feeling with variable awareness of the situation, attention and appraisal stages of affect generation. Working with a client reporting this affective pattern, a clinician may seek to reveal the contents of these antecedent stages 105 . What are the situational triggers for these states? Are there selective perceptual processes involved? How is the selectively perceived situation appraised? Even though the client may initially lack awareness of these stages, he may provide reliable information through interviewing techniques such as behavioral chain analysis 97 . Relevant information may also be obtained through daily assessment techniques that can recover aspects of situations and cognitions that tend to be less available at later recall 106 .
Focusing on similarities between different affective states can also be useful for selecting and tailoring treatments for specific clients. For example, borrowing an insight from systematic desensitization 107 , a therapist may develop a hierarchy of affective states based on how difficult they are for a client to regulate. For instance, a client may resist unhealthy food with ease, downregulate his anger with moderate success, but almost never overcome a bout of depressed mood. The therapist could incorporate this hierarchy into a program of guided affect regulation practice that introduces different regulation techniques using assignments from the lower end of the hierarchy and gradually moving upwards. For instance, a client could first foster healthier eating habits through situation modification by putting healthy snacks in easily accessible locations. He may then use this experience as a helpful metaphor for finding ways to use situation modification to improve his depressed mood.
Interplay of affect generation and regulation
The process model of affect regulation suggests that the same manifestation of unhealthy affect may arise from different mixtures of maladaptive affect generation and maladaptive affect regulation 2 .
On the one hand, this suggests that affect generation and affect regulation form an integrated dynamic system that can be analyzed as a single functional unit. For instance, for many clinical purposes, such as initial screening for affective disturbances, it is largely unimportant whether a problematic affective pattern reflects overly strong affect generation or overly weak affect regulation. On the other hand, the process model also exemplifies the value of separating the contributions of affect generation and regulation to unhealthy affect. Teasing these contributions apart can be challenging, as the client may have limited awareness of the functioning of different affective processes. The interviewing techniques discussed above may be adapted to this task. In addition, the research community has started to devise promising combinations of self‐report, behavioral and statistical approaches for separating affect generation from affect regulation 39 .
Differentiating affect generation from affect regulation can also be important for designing targeted treatments. In many cases, people suffer from a combination of maladaptive affect generation and maladaptive affect regulation, and thus benefit from simultaneous – or sensibly sequenced – treatments targeting both. For instance, in the case of major depressive disorder, pharmacological interventions can be used to treat maladaptive affect generation, while psychotherapy can be used to improve affect regulation 108 . Omitting one or the other component from the treatment regime would reduce its overall efficacy. There can also be cases where the unhealthy affective pattern can be traced back to a single primary source among affect generation and affect regulation processes. In these instances, adequate targeting of treatment becomes even more important. For instance, consider a client who is already relatively proficient in affect regulation but suffers primarily from maladaptive affect generation. If offered only further affect regulation training, with no help with maladaptive generation, he might experience reduced self‐efficacy that could lead to deterioration of the therapeutic relationship and treatment compliance.
Decomposing affect regulation
The third implication of the process model of affect regulation is that the stages of identification, selection, implementation and monitoring, and their respective inputs, can be used as more specific targets for assessment as well as treatment.
For instance, an assessment approach could be designed to determine difficulties with identifying regulation goals, selecting regulation strategies, implementing them through contextually suitable actions, and monitoring the outcomes to make necessary modifications. Parts of these phenomena can be assessed using existing self‐report instruments, such as the Toronto Alexithymia Scale 109 , the Emotion Regulation Questionnaire 110 , the Cognitive Emotion Regulation Questionnaire 111 , the Difficulties in Emotion Regulation Scale 112 , the Coping Flexibility Scale 113 , and many others. However, as these measures assess overlapping but incomplete aspects of the four affect regulation stages, we encourage future efforts to design comprehensive measures of the process model of affect regulation. These efforts may extend beyond self‐reports to behavioral and psychophysiological assessments such as measuring affective responses to standardized stimuli using physiological correlates under specific instructions 114 .
Clarifying whether a particular affect regulation problem arises from difficulties during the identification, selection, implementation or monitoring stage can be an important step toward making informed decisions about personalized treatment options. For instance, people who exhibit difficulties during the identification stage due to misrepresentation of current affective states might benefit from mindfulness‐based therapy modules and technological aids. People who exhibit difficulties during the selection stage might benefit from learning new adaptive strategies, from increasing strategy specific self‐efficacy, as well as from modification of dysfunctional beliefs contributing to misevaluation of strategies. People who struggle with the implementation stage might benefit from external aids such as mobile applications with suggestions on how to execute different strategies. People who struggle with the monitoring stage might benefit from mindfulness interventions to increase awareness about changes in the affective state and context as well as training to switch between strategies according to changing circumstances. In most cases, individual clients may exhibit difficulties with more than one, but not necessarily all, decisions involved in affect regulation.
From mental illness to well‐being
Although this paper has focused primarily on mental illness, the process model of affect regulation is equally relevant when considering the role of affect in psychological well‐being 115 . The goals of psychiatry and clinical psychology extend from preventing and reversing maladaptive affect generation and regulation patterns to promoting and restoring their adaptive counterparts. To live up to this ideal, assessment as well as treatment approaches should be designed without forgetting about healthy affect. For instance, assessment approaches should target affective states that are known to improve well‐being. These include hedonically positive experiences such as satisfaction, happiness or love, as well as affective states that can be hedonically negative but still add eudaimonic value by providing meaning, elevating experiences, or fostering personal growth 116 .
Psychological well‐being is equally relevant for designing interventions. We have seen how the process model of affect regulation can be used to organize regulation techniques aimed at reducing hedonically negative (e.g., depressed mood) and instrumentally harmful affective states (e.g., maladaptive positive affect in bipolar disorder). However, the process model is an equally useful framework for organizing techniques that promote hedonically positive or instrumentally helpful affective states. For instance, situational strategies such as going for hike can be used to generate pleasant mood 117 . Attentional strategies such as focusing on things that a person is grateful for can be used to promote happiness and a sense of meaning 118 . Cognitive strategies such as contrasting a mental image of a job well done with the current situation where more work is needed can be used to promote feeling challenged and thereby more motivated 119 . Response modulation strategies such as exercising can be used to generate feelings of being relaxed and fulfilled 120 . Promoting each of these behaviors can further benefit from analyzing their antecedents within the identification, selection, implementation and monitoring stages.
CONCLUSIONS
We have proposed a process model of affect regulation as a common framework for understanding how affect is generated, how it can be regulated, and how both processes jointly contribute to mental health. This framework conceives of affect generation as a four‐stage feedback loop, and affect regulation as a coordinated four‐stage decision process. Adaptive functioning of each of these stages promotes mental health and well‐being, whereas maladaptive functioning of these stages can increase the risk of mental illness.
We believe that the process model of affect regulation offers a useful framework for clinical research as well as practice. The model is in line with broader efforts to reveal the transdiagnostic dimensions underlying mental illnesses 14 , 121 . It relates complex affective patterns to simple psychological mechanisms such as feedback loops 29 and decision processes 122 , 123 , which are amenable for computational and neural research.
The model calls for more research, in particular to realize the assessment and treatment avenues it opens up. On the one hand, it is important to provide further evidence that different symptoms, syndromes and disorders are indeed linked to difficulties in different affect generation and affect regulation stages. On the other hand, it is also important to clarify how existing treatments impact these stages as well as to devise novel treatments.
We hope that, by facilitating and scaffolding these important advances, the process model of affect regulation can contribute to the advancement of evidence‐based personalized psychiatry and psychotherapy.
ACKNOWLEDGEMENT
This work was supported by the Estonian Research Council grants IUT2‐13, PUTJD‐79, and MOBTP‐17.
Thinking about mental health
Asu experts discuss stigmas, solutions for mental health awareness month.

Photo courtesy iStock/Getty Images
At its most basic level, mental health is related to how we think and feel.
It is the intensity or disproportionate reaction of those thoughts and feelings that can determine our level of mental health.
According to the Centers for Disease Control and Prevention, mental health includes our emotional, psychological and social well-being, and affects how we think, feel and act. It also helps determine how we handle stress, relate to others and make healthy choices.
“Our mental health becomes the filter through which we experience the world,” said Aaron Krasnow , associate vice president of health, counseling and wellness at Arizona State University. “It’s the filter for our relationships with others and determines our views of ourselves.”
Mental health resources at ASU
• ASU Health Services
• ASU Wellness
• ASU Center for Mindfulness
• ASU Employee Assistance Program
This May is Mental Health Awareness Month, which was established in 1949. The mission of the month is to increase awareness of the importance of mental health and wellness in our lives, and to educate the public about the reality of living with a mental health condition.
According to the World Health Organization, mental health conditions involve significant disturbances in thinking, emotional regulation or behavior. The most common conditions in the U.S. are anxiety and depression, which make up nearly 30% of all mental illness diagnoses.
Mental health diagnosis can also include illnesses such as bipolar disorder, post-traumatic stress disorder, eating disorders, disruptive behavior, dissocial and neurodevelopmental disorders.
According to the Centers for Disease Control and Prevention, factors that can contribute to mental illness include adverse childhood experiences — such as trauma or a history of abuse — ongoing (chronic) medical conditions — such as a traumatic brain injury — biological factors or chemical imbalances in the brain.
Stigmas and misconceptions
But throughout history, mental illnesses has often been misunderstood.
According to the National Alliance on Mental Illness, the pervasive stigma lies in the misconception that mental health conditions are a personal and moral failing — rather than illnesses requiring treatment, like any other health issue.
Stigmas can be evident in the language often associated with mental illness: crazy, psycho, loony bin.
These attitudes can compound a person’s suffering and inner struggles, leading to shame and isolation.
“Those who live with and treat mental illness know that stigma is a major contributing factor,” said Alexandra Brewis , a Regents and President's Professor in the School of Human Evolution and Social Change . “The threat or experiences of being judged means people may be less willing to seek help and are more likely to discontinue treatment.
"The discriminations triggered by stigmas also make life more difficult in many other arenas, like being denied employment or safe and affordable housing. These then feed back into worse mental health. Without stigma, mental health is much easier to achieve and sustain.”
Stigma sticks like super glue. Once it is attached to a disease, it is incredibly difficult to remove because it requires substantial cultural changes. Alexandra Brewis Regents and President's Professor
A global issue
Nearly 58 million adults in the U.S. experienced a mental illness in 2021. According to the National Institute of Mental Health, that represents 1 in 5 adults.
And COVID-19 only exacerbated the problem.
The World Health Organization reported that the COVID-19 pandemic triggered a 25% increase in the prevalence of anxiety and depression worldwide. Megan Jehn says the pandemic was particularly hard on children.
“Epidemiologic data suggests that mental health issues are rising among kids, most likely being the result of a perfect storm of increasing challenges before COVID-19 struck and living through a highly disruptive pandemic,” said Jehn, an epidemiologist and professor of global health in the School of Human Evolution and Social Change.
A landmark study published during the pandemic found that 25.2% of youth experienced depression and 20.5% experienced anxiety during the pandemic worldwide, which is double that of pre-pandemic estimates, Jehn said.
The American Psychological Association described the pandemic as a "collective trauma" in their study “ Stress in America 2023: A Nation Recovering from Collective Trauma.”
The trauma was connected to the death of more than 1 million Americans and the cultural changes the pandemic ushered in.
“It is actually a group-level vulnerability that may have exacerbated the day-to-day stressors,” said Leah Doane , a professor in ASU’s Department of Psychology.
Stopping the stigma
Despite this, stigmas may remain because society tends to separate themselves from people with mental health issues — which compounds the loneliness for those affected.
“Part of the problem in our culture is we live in an extremely trauma- and grief-avoidance world…,” said Joanne Cacciatore , a professor at ASU’s School of Social Work whose research focuses on traumatic grief.
Cacciatore explains that people have survived many individual and collective traumas throughout history, including the Holocaust.
“They survived, but social support was essential. If we don’t have that, then suffering is even more debilitating. Loneliness and isolation are added to the traumatic grief experience,” said Cacciatore, who believes that the material covered in ASU’s trauma and bereavement graduate certificate is indispensable for mental health professionals.
Last year, the U.S. Surgeon General Vivek Murthy put out a call to action over public health crisis of loneliness, isolation and lack of connection in our country. Even before the COVID-19 pandemic, nearly half of U.S. adults reported experiencing living with a significant level of loneliness.
“We need to remember that we all belong to one another,” said Nika Gueci , executive director of ASU’s Center for Mindfulness, Compassion and Resilience . “We need to remember that we cannot live without one another right? So when we see someone in distress, then it’s really up to us to help.”
Gueci is working with the Arizona Department of Health Services on a statewide strategy to reduce loneliness and social isolation.
“It doesn’t always have to be up to them to pull themselves up. It's up to us to be there for them so that they can better be able to pull themselves up.”
The hope behind Mental Health Awareness Month is to uncover the stigmas and understand the struggles associated with those affected. And perhaps then, communities can become a source of comfort and healing for people.
Krasnow believes that as a society, the stigma around mental health seems to be subsiding — especially in younger generations.
“They are more likely to share their mental health journey and more likely to be accepting of each other,” he said. “And there is evidence of that.”
But society has a long way to go before stereotypes can be completely set aside.
“Stigma sticks like super glue,” Brewis said. “Once it is attached to a disease, it is incredibly difficult to remove because it requires substantial cultural changes.”
Brewis is focused on finding solutions to complex global health challenges. Her current work is based on field research around several matters, including stigma.
“Developing empathy is key,” Brewis said. “But that is a hard thing to teach and nurture. Interestingly, celebrities sharing their mental health struggles can move the needle and has proven to be one mechanism that can change public opinion. …
"When we start to connect a condition to someone we admire and look up to, it can foster empathy.”
More Health and medicine

$5M grant to allow ASU to help train medical professionals in areas of critical need
The College of Health Solutions at Arizona State University has been awarded a $5 million grant from the Department of Health and Human Services’ Agency for Healthcare Research and Quality to launch…

Intermittent fasting shows promise in improving gut health, weight management
A new study by researchers from Arizona State University and their colleagues highlights a dietary strategy for significant health improvement and weight management. Participants following an…
ASU research finds link between removal of uterus, brain function
The uterus has three clear jobs: periods, pregnancy and labor. At least, that’s what the medical textbooks tell us. But new research is suggesting the organ may play a bigger role in female health.…

Online Students
For All Online Programs
International Students
On Campus, need or have Visa
Campus Students
For All Campus Programs
Why is Mental Health Awareness Important?

You might take your mental health for granted when things are going well. But being aware of symptoms and treatment options can prepare you to face any unexpected challenges and support those around you.
Why is Mental Health Ignored?

La Valle holds a doctorate in clinical psychology and was the recipient of a Provost award.
“Oftentimes, mental health falls by the wayside,” he said. But taking care of this aspect of your wellness is one of the most important things you can do if you want to lead a full and productive life.
According to La Valle, if you aren’t monitoring your mental health, you could be more vulnerable to its impacts.
“If you are not actively aware of your mental state you may notice things like shortened attention span, irritability and difficulty being actively engaged with your surroundings,” said La Valle.
If you have a solid awareness about mental health, on the other hand, you can take action to avoid symptoms like these and make strides to improve your overall well-being.
Why is Mental Health Important in Everyday Life?
According to the Substance Abuse and Mental Health Services Administration ( SAMHSA ), mental health affects multiple aspects of wellness, including:
- Emotional well-being
- Psychological well-being
- Social well-being
Although mental and physical health are often discussed as separate phenomena, they’re actually quite intertwined, too.
“It is common to see someone struggling with mental health to experience physical health concerns,” La Valle said. “For example, anxiety and stress can lead to things like high blood pressure, headaches and loss of appetite.”
He noted that the reverse is also true, and there are benefits that come with exercising and taking care of your physical health.
“Engaging in regular self-care and taking care of your mental state should be scheduled into your daily routine just like doctor’s appointments, work, and chores,” La Valle said. “Taking time for yourself helps to decrease burnout and allows you to be more present in the moment.”
How Does Mental Health Affect Society at Large?
In addition to other sociological factors, world events like pandemics, war and political unrest can also affect wellness on a broad scale. For example, Mental Health America reports that global conflict can cause high levels of stress and lead to depression, even if you aren’t impacted directly.
La Valle also pointed out that social media is a double-edged sword in this regard, capable of both helping and harming the general public.
“Apps like TikTok have lots of videos surrounding mental health, many which contain misinformation,” he said. “At the same time, they also help to decrease the stigma around mental health by opening up conversations on these topics.”
Why is Mental Health More Important Now Than Ever?
There are many factors that could be contributing to this trend, but La Valle also noted that one thing is certain: the world is finally starting to pay more attention to mental health.
“Mental health has always been important,” he said. “Current research just further strengthens the connection between mental and physical health.”
He said discoveries about this connection between mental and physical health have led to more conversations, helping to change the public’s perspective on mental illness at large.
“The stigma surrounding mental health has greatly dramatically declined and individuals are seeking support now more than ever,” said La Valle. “However, we still have work to do in letting people know it’s OK to not be OK sometimes.”
What Mental Health Resources are Available?
If you or someone you know is struggling, consult a doctor or clinician. To find care, you can reach out to your insurance company or use Psychology Today’s directory to find a mental health professional in your area.
For immediate help, the following services are also available in the United States:
- 988 Suicide and Crisis Lifeline : 988
- Substance Abuse and Mental Health Services Administration : 1-800-662-HELP (4357)
- Crisis Text Line : Text "HOME" to 741741
"Feeling confident and being open about your own mental health can be really powerful," La Valle said. "Don’t be afraid to put yourself first."
A degree can change your life. Choose your program from 200+ SNHU degrees that can take you where you want to go.
Mars Girolimon ’21 ’23G is a staff writer at Southern New Hampshire University where they earned their bachelor’s and master’s, both in English and creative writing. In addition to their work in higher education, Girolimon’s short fiction is published in the North American Review, So It Goes by The Kurt Vonnegut Museum & Library, X-R-A-Y and more. They’re currently writing their debut novel, which was Longlisted for The First Pages Prize. Connect with them on LinkedIn .
Explore more content like this article

Academic Spotlight: Dr. Beth VanOrsdale, Associate Dean of Academic Effectiveness

Dealing with Anxiety: Strategies for Relief and Management

What is Post-Graduation Depression and How to Overcome It
About southern new hampshire university.

SNHU is a nonprofit, accredited university with a mission to make high-quality education more accessible and affordable for everyone.
Founded in 1932, and online since 1995, we’ve helped countless students reach their goals with flexible, career-focused programs . Our 300-acre campus in Manchester, NH is home to over 3,000 students, and we serve over 135,000 students online. Visit our about SNHU page to learn more about our mission, accreditations, leadership team, national recognitions and awards.
The independent source for health policy research, polling, and news.
The Mental Health Crisis Within the Mental Health Crisis
Drew Altman Published: May 22, 2024

I was able to make some changes while in office, including improving staffing and closing an ancient and dangerous psychiatric facility for youth built in the late 1800s, but it was far from enough to satisfy me or those families. The legislature wasn’t much interested unless a patient escape made the front pages. Despite the tireless work of advocates and a few champions in the legislature, when it came time to allocate resources in the state budget, the chronically mentally ill wasn’t a funding priority. It was one of a few longstanding problems I likely could not fundamentally affect in a term in office in a large umbrella agency with seven other demanding divisions, including Medicaid and welfare. In government, you pick your shots. For me, then, the priorities were welfare reform, Medicaid managed care, school-based social services, homelessness, and of course inevitably, the crisis of the day or week.
That night, resigned to my limitations, I asked the press and staff to leave the room and met privately with the families. Near the end of the meeting, I gave them my personal phone number, feeling that if I could not make systemic changes, I had the authority to at least help individual cases. I heard from many of them, sometimes in the middle of the night when something went terribly wrong. I learned their stories. Sometimes we found a way to help individual cases, but even with control of a third of the state budget and workforce in the department, there was often little that could be done.
Decades later at KFF, we did a survey with CNN on mental health in America in 2022. Scrolling through our findings, headlines jumped off the page. Ninety percent of the public believed there was a crisis in mental health in America. Big numbers of people reported real problems accessing and paying for mental health services. Then they were there—the families. Somewhat buried in the survey was the story in data I had learned all those years ago in New Jersey: the mental health crisis isn’t just about patients with mental illness or the teens struggling with emotional problems or individuals coping with loneliness, it’s also deeply and centrally about families.
Any family with a family member experiencing mental illness knows all too well the serious stresses and strains that are part of the experience. But there was something else in the data that was even more striking: the number of families dealing with true crisis level events—a family member living on the street; making the brutal decision to institutionalize a loved one who is a threat to themselves or others; rushing a spouse or child to an ER with a drug overdose; self-harm; suicide attempts. And while we have inadequate services for families dealing with mental illness generally, we have even fewer services and supports for the families dealing with crisis events. The numbers of families experiencing a very serious mental health-related event is so large that it may constitute a crisis within the larger mental health crisis, and it’s one that does not receive enough attention.
Our Mental Health in America survey showed that these crisis events are pervasive and include many of the worst things that can happen in a family:
- Twenty-eight percent of all Americans say that their family had to take a painful step, like institutionalizing a family member because they were a threat to themselves or others.
- Twenty-one percent said they or a family member had a drug overdose requiring an ER visit.
- Fourteen percent said they or a family member ran away from home and lived on the streets due to mental health issues.
- Sixteen percent said a family member experienced homelessness because of a mental health problem.
- Eight percent said they or a family member had a severe eating disorder requiring hospitalization or in-person treatment.
- Twenty-six percent said they or a family member engaged in cutting or self-harm behaviors.
- And 16% had a family member who died from suicide.
When we looked at the overlap between the problems, half of American families (51%) experienced one or more of these severe crises. Let that sink in: half of all American families had a severe mental health-related crisis. It means that when you measure the impact of the mental health crisis, you really need to multiply manifold, something official statistics don’t do. These are the kinds of crises that truly challenge families. Parents and siblings struggle to deal with them and may never be the same after they occur. Often families make huge sacrifices to assist family members in crisis.
The survey data show some of the consequences. Over four in ten say the crisis had a major impact on their own mental health or their family’s relationships. One in five say it had a major impact on the family’s financial situation. This group, which has the most direct experience with mental health care in this country, are more likely to believe that mental health issues in both children and adults are at a crisis level in the U.S., and that most people are not able to get the mental health services they need.
Not surprisingly, every bad outcome is complicated by poverty, and family crises like these are more likely to occur in lower income households. Fifty-seven percent of people living in households earning less than $40,000 a year experienced these crises compared with 43% of those in families earning more than $90,000.
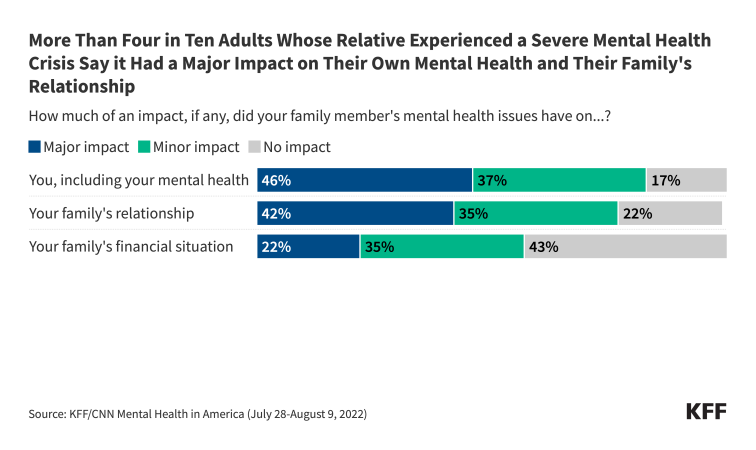
Some adults know or can figure out who to call if a family member needs help with a serious mental health-related problem, such as a drug problem or a potential suicide. Local and national crisis hotlines are sometimes available for different problems. But how many know who to call for a family fraying and in crisis? How many would be afraid to call for fear of alerting law enforcement or child protective services to some problems? Sometimes, of course, dysfunction or something worse in a family contributes to a family member’s problem or even is the problem, further complicating solutions.
NAMI , the national organization representing families with mental illness, does valiant work through its chapters providing support and advocacy, but it can only do so much and cannot manufacture services that do not exist for a family dealing with a crisis.
Ultimately, the best thing we can do for families experiencing a mental health related crisis is to more effectively address the underlying problem affecting their family member. In my next column, I will review the problems Americans have accessing mental health services.
There wasn’t a great deal I could do on the spot for those families at the psychiatric hospital in New Jersey back then. But the data are a reminder of how the mental health crisis in America affects families as well as individuals, magnifying its impact, expanding the policies and services needed to address it, and changing the way we need to think about the problem.
View all of Drew’s Beyond the Data columns.
Also of Interest
- Beyond the Data
- KFF/CNN Mental Health In America Survey
- A Look at Substance Use and Mental Health Treatment Facilities Across the U.S.
- Taking a Look at 988 Suicide & Crisis Lifeline Implementation One Year After Launch
- Search the site GO Please fill out this field.
- Newsletters
- Sexual Health
What Happens When You Don't Ejaculate (Release Sperm) for a Long Time?
Wendy Wisner is freelance journalist and international board certified lactation consultant (IBCLC). She has written about all things pregnancy, maternal/child health, parenting, and general health and wellness.
:max_bytes(150000):strip_icc():format(webp)/WendyWisner2022-d8111a5bfee84913ac464f394bc98516.jpeg)
- Side Effects
Benefits of Not Ejaculating
Benefits of ejaculating.
- Side Effects of Frequent Ejaculation
When To See a Healthcare Provider
FatCamera / Getty Images
Ejaculation refers to semen being released from the penis during orgasm. There are many reasons why someone may not ejaculate for a long time. Some people do it intentionally for personal or religious reasons. Some people abstain to increase their sperm count for fertility purposes. Other people may have a health condition that makes ejaculation difficult or impossible.
The effects of not ejaculating haven’t been studied extensively, but there is no evidence that doing so—even for extensive periods—is harmful. There are no known negative side effects of not ejaculating. That said, if you are unable to ejaculate, or are having trouble ejaculating, it’s important to see a healthcare provider to find out if you have an underlying health condition that may be causing this.
Reasons You're Not Ejaculating
There are several reasons why someone may not be ejaculating. Sometimes the reasons are intentional, and sometimes they are not.
Intentionally Abstaining
Whether or not to engage in sexual activity or masturbation is a personal choice. Some people make mindful choices not to ejaculate for specific periods or extended periods. For example:
- Many religions advise abstention from masturbation or sexual activity.
- Someone may also choose not to ejaculate for personal reasons or as a part of a spiritual journey.
- Healthcare providers might recommend abstaining from ejaculating for several days while trying to conceive or before fertility treatments .
Delayed Ejaculation
A sexual disorder called delayed ejaculation can be the cause of not ejaculating. Delayed ejaculation is defined as either a delay in the ability to ejaculate or a complete inability to ejaculate.
Delayed ejaculation is not common and experts aren’t sure what causes it. It used to be believed that relationship issues or psychological issues cause delayed ejaculation. It might be caused by endocrine, genetic, or neurobiological conditions, or it might be a medication side effect. Endocrine conditions are hormone-related, such as low testosterone.
Retrograde Ejaculation
Retrograde ejaculation is when semen is not expelled through the penis during orgasm, but enters the bladder instead. This is often referred to as a “dry orgasm” because you experience an orgasm, but you see a very low volume of semen or no semen at all.
Conditions like diabetes, previous pelvic surgeries, neurological conditions, and bladder malformations can cause retrograde ejaculation. It may also be a side effect of certain medications.
Anejaculation
Anejaculation is when you don’t ejaculate at all during sexual activity. A person with anejaculation experiences erections without ejaculation. However, they may ejaculate during nocturnal emissions (wet dreams) or while masturbating.
There are various potential causes of anejaculation, including health conditions like spinal cord injuries, diabetes, and multiple sclerosis. Potential psychological causes include a lack of body awareness, guilt or shame about sex, and performance anxiety .
People with male reproductive organs can ejaculate and produce sperm for their entire lives—there isn’t a particular age where this ability goes away. However, similarly to people with female reproductive organs, reproductive capacity decreases as they age. As such, it can be more difficult to experience erections and orgasms/ejaculations as they get older.
Side Effects of Not Ejaculating for a Long Time
There is nothing inherently harmful about not ejaculating for a long time. There are no known dangerous physical or psychological side effects. However, some general side effects are possible for certain individuals.
Physical Effects
Testes constantly produce sperm. If you don’t ejaculate it, the sperm becomes reabsorbed into the body. Some people are concerned that you will get “blue balls” if you don’t ejaculate, or pain due to sexual arousal that doesn’t end in orgasm. However, there are no known medical problems associated with this phenomenon, and any discomfort resolves without intervention.
Psychological Effects
The mental health effects of not ejaculating or abstaining from ejaculating aren’t well-researched at this time. However, many people report different emotions when they haven’t ejaculated for a long period of time. Some people might experience clarity or peace of mind , while others may report feeling more irritated or distressed.
People who experience ejaculated-related health problems, such as delayed ejaculation or anejaculation, may experience relationship stress, or anxiety surrounding sexual contact and sexual desire.
There are no reported benefits of not ejaculating, and the benefits of this practice have not been studied. Nevertheless, people who intentionally refrain may report benefits, such as mental and emotional balance, decreased fixation on sex, increased energy, and stress relief.
While many people abstain from ejaculating for several days while trying to conceive, or going through fertility treatments, the effectiveness of this practice is not clear. Research has found that abstaining from ejaculating for several days increases sperm count and semen volume. It’s less clear if this practice is helpful for other sperm aspects, such as motility (movement speed), vitality, and morphology (sperm shape).
Again, the mental health benefits of ejaculating or not ejaculating are not well studied. Still, there are some immediate benefits to experiencing orgasm, including reduced stress, improved mood, and even pain relief.
There is some evidence that ejaculation frequency might be protective against developing prostate cancer . For example, one 2016 study found that participants who reported higher rates of ejaculation were less likely to be diagnosed with prostate cancer.
Side Effects of Ejaculating Too Frequently
It’s normal to ejaculate frequently, and ejaculating daily or even several times a day has no known negative side effects. Ejaculating frequently may cause certain side effects, such as chafing of the skin (usually from masturbation specifically) or fatigue .
Some people may be concerned that frequent ejaculation may cause sex addiction or other sexual disorders. While the exact causes of sex addiction haven’t been identified yet, it is not thought to be caused by excessive masturbation or sexual activity. On the other hand, excessive masturbation or sexual activity may be a symptom of a sex addiction.
Masturbating frequently might affect sexual function, leading to issues like sexual desensitization, where you become less sensitive to sexual stimulation. Some people who masturbate frequently experience trouble getting erections or reaching orgasm through other forms of sexual activity.
It’s normal for some people to not ejaculate for a long time. In most cases, it will not cause physical or psychological harm.
See a healthcare provider if you have any concerns about your ejaculation patterns. If you are intentionally not masturbating because of guilt or shame about sex or masturbation, you may want to speak to a therapist about your feelings and concerns.
Conditions like diabetes, multiple sclerosis, and sexual disorders can result in an inability to ejaculate. Endocrine disorders, neurological disorders, and medication side effects may also cause these symptoms. A healthcare provider can evaluate you for any underlying medical conditions and discuss treatment plans.
A Quick Review
Not ejaculating for several days, weeks, or even longer, is not damaging to your health. Some people abstain from ejaculating for religious reasons, personal reasons, or to increase sperm count while trying to conceive .
If you are unable to ejaculate, you may have an underlying medical condition causing these symptoms. It's important to visit your healthcare provider for an evaluation.
Albobali Y, Madi MY. Masturbatory guilt leading to severe depression . Cureus . 2021;13(3):e13626. doi:10.7759/cureus.13626
Hanson BM, Aston KI, Jenkins TG, et al. The impact of ejaculatory abstinence on semen analysis parameters: A systematic review . J Assist Reprod Genet . 2018;35(2):213-220. doi:10.1007/s10815-017-1086-0
Gopalakrishnan R, Thangadurai P, Kuruvilla A, et al. Situational psychogenic anejaculation: A case study . Indian J Psychol Med . 2014;36(3):329-331. doi:10.4103/0253-7176.135393
Abdel-Hamid IA, Ali OI. Delayed ejaculation: Pathophysiology, diagnosis, and treatment . World J Mens Health . 2018;36(1):22-40. doi:10.5534/wjmh.17051
Society for Male Reproduction and Urology. Treatment options for patients with ejaculatory dysfunction .
Gunes S, Hekim GN, Arslan MA, et al. Effects of aging on the male reproductive system . J Assist Reprod Genet . 2016;33(4):441-454. doi:10.1007/s10815-016-0663-y
MedlinePlus. Sperm release pathway .
Levang S, Henkelman M, Neish R, et al. “Blue balls” and sexual coercion: A survey study of genitopelvic pain after sexual arousal without orgasm and its implications for sexual advances . Sex Med . 2023;11(2):qfad016. doi:10.1093/sexmed/qfad016
Mascherek A, Reidick MC, Gallinat J, et al. Is ejaculation frequency in men related to general and mental health? Looking back and looking forward . Front Psychol . 2021;12:693121. doi:10.3389/fpsyg.2021.693121
MedlinePlus. Delayed ejaculation .
Gianotten WL. The Health Benefits of Sexual Expression . In: Geuens S, Polona Mivšek A, Gianotten W. (eds). Midwifery and Sexuality . doi:10.1007/978-3-031-18432-1_4
Rider JR, Wilson KM, Sinnott JA, et al. Ejaculation frequency and risk of prostate cancer: Updated results with an additional decade of follow-up . Eur Urol . 2016;70(6):974-982. doi:10.1016/j.eururo.2016.03.027
Fong TW. Understanding and managing compulsive sexual behaviors . Psychiatry (Edgmont) . 2006;3(11):51-58.
Huang S, Niu C, Santtila P. Masturbation frequency and sexual function in individuals with and without sexual partners . Sexes . 2022; 3(2):229-243. doi:10.3390/sexes3020018
Related Articles
- Short Videos
- Web Stories
- Crushed by careers
- Diabetes Dilemma
- Diet & Fitness
- Health Diseases
- Miscellaneous
What Is Cognitive Distortion And How Does It Affect Your Mental Health?

- Written by : Manali Momaya
- Updated at: Jun 01, 2024 08:25 IST

The root cause of mental health problems starts with your thoughts. The flow of uncontrolled thoughts can lead to several minor to major mental health issues. Cognitive distortion is one such type of thinking process which can lead to anxiety, stress and other mental health issues.
Cognitive distortion are thoughts which are not based on reality or facts, most of them being negative. In this, a person tends to think or perceive reality inaccurately due to being exaggerated or irrational. For instance, if a friend, family member or a loved one is not responding to your calls and it has been a while, there’s a high possibility that negative thoughts will take over your mind.
What is Cognitive Distortion?
Giving a simple explanation, Priyal Awasthi said, “You can think of them as errors of thinking.” According to the American Psychological Association (APA), cognitive distortions are faulty or inaccurate thinking, perception, or beliefs.
Harvard Medical School defined cognitive distortion as internal mental filters or biases that increase our misery, fuel our anxiety, and make us feel bad about ourselves. Our brains are continually processing lots of information.

As per Awasthi, these distortions involve systematic errors in the way people perceive, interpret, and process information. Some common examples include:
1. All-or-nothing thinking: Seeing things as entirely black-and-white, with no shades of gray in between.
2. Overgeneralization: Drawing broad conclusions from a single event or piece of evidence.
3. Mental filtering: Focusing only on the negative aspects of a situation while disregarding the positive aspects.
4. Catastrophizing: Expecting the absolute worst-case scenario and blowing things out of proportion.
5. Personalisation: Assuming that everything is a reaction to you, even when it's not personal.
Often, such irrational thoughts are so ingrained in people's thinking patterns that they are imperceptible, making them dangerous for their well-being and ability to reason emotionally.
Signs of Cognitive Distortion
If you notice these signs frequently or they're significantly impacting your mood, behaviour, or well-being, then it's time to seek help. Awasthi helped us list these symptoms of cognitive distortion.
1. If you find yourself frequently thinking in absolutes like "always " or "never," or viewing situations as entirely good or bad with no middle ground, this could be a sign of all-or-nothing thinking or black-and-white thinking distortions.
2. If you tend to automatically assume the worst-case scenario or blow things out of proportion, you may be engaging in catastrophizing distortions.
3. If you let one single negative event decide your worth or generalise it as a pattern of failure or inadequacy, you may be overgeneralizing.
4. If you frequently engage in harsh self-criticism or put yourself really down, this could be a sign of cognitive distortions.

5. Your emotional reactions seem exaggerated or out of proportion to the situation, and you're bursting out over trivial things which you would ideally let go of.
6. You struggle to consider other viewpoints or interpretations, and your perspective seems rigid or inflexible.
7. Physical symptoms: Cognitive distortions can sometimes manifest in physical symptoms like muscle tension, headaches, or a rapid heartbeat, as they can contribute to increased stress and anxiety.
Adding, Awasthi said, “If you're experiencing these signs, it may be helpful to seek support from a therapist or counsellor to address and challenge these distorted thought patterns.”
Consequences of Cognitive Distortion

Explaining the consequences cognitive distortion can cause, Awasthi said, “Cognitive distortions can create a negative cycle where distorted thoughts lead to unhelpful emotions and behaviours, which then reinforce the distorted thinking patterns. This can significantly impair daily functioning, well-being, and life satisfaction.”
Some specific mental health issues that can stem from cognitive distortions are depression, anxiety disorders, eating disorders, obsessive-compulsive disorders, and so on, along with making the individual more susceptible to stress, worry, and low self-esteem.
She further added, “Emotionally, it can pave the way for negative emotions like sadness, anger, frustration, emotional instability, mood swings, and an overall difficulty in regulating emotions.”
International Children's Day: History, Theme, Significance
All possible measures have been taken to ensure accuracy, reliability, timeliness and authenticity of the information; however Onlymyhealth.com does not take any liability for the same. Using any information provided by the website is solely at the viewers’ discretion. In case of any medical exigencies/ persistent health issues, we advise you to seek a qualified medical practitioner before putting to use any advice/tips given by our team or any third party in form of answers/comments on the above mentioned website.
- # Cognitive distortion
- # Mental health
- # Overthinking

Why Teaching Critical Race Theory Matters for Mental Health
By learning this concept in school, children can begin to dismantle racism..
Posted November 1, 2021 | Reviewed by Devon Frye

Since the beginning of the new school year, debates around teaching Critical Race Theory (CRT) in schools have escalated. From a mental health perspective, though, I argue that the decision of whether schools should implement CRT as part of students’ curriculum is clear: It’s a vital part of the future of education .
As mental health professionals, we take an oath to do no harm . We have a duty to protect and a duty to warn. And we value the self-determination, autonomy, and inherent worth and strength of all individuals. Teaching CRT to children has mental health implications for both students of color and white students, and, as such, mental health professionals have a moral and ethical obligation to respond, react, and take a strong stance supporting CRT in schools.
What Is Critical Race Theory?
CRT is an academic concept stating that race is a social construct embedded in our social, political, legal, and economic policies, structures, systems, and institutions. Mental health professionals must understand that we do not have to be CRT scholars or work at educational institutions to apply it to our professional or advocacy work.
Understanding structural racism within our systems and policies related to education, income, housing, food, criminal justice, the environment , and health care matters greatly for addressing persistent population health inequities, including mental health inequities. Sadly, one does not have to look far to see the evidence of institutionalized racist practices and the impact of generations of bias in mental health treatment.
Racial Trauma
Compared to white patients, Black, Indigenous, and people of color are more likely to be coerced, restrained, treated with drugs , or medicated in emergency departments than to receive psychotherapy , and are more likely to be misdiagnosed or diagnosed with a serious mental illness like schizophrenia , while remaining underdiagnosed with post- traumatic stress disorder and mood disorders. To add to this, there is a lack of diversity among mental health providers , resulting in frequent racism, micro-aggressions, and barriers to support.
The pushback against teaching CRT, and an inaccurate portrayal of Black history in schools, communicates to people of color that their lived experience, perspective, and daily struggle, past and present, in a white supremacist society does not matter and will never matter. When kids believe they do not matter, it impacts identity , esteem, efficacy, and the ability to succeed. The debate and pushback could even represent yet another racial trauma that brings with it an intense emotional and mental injury.
Hiding historical trauma prolongs and amplifies present trauma and deepens its impact. The cumulative emotional and psychological wounds are carried across generations leading to higher rates of mental and physical illness, substance use, and the decimation of families and communities.
Critical Thinking—How Teaching CRT Can Benefit Students
Just as the teaching of CRT in schools is vital to the mental health of children of color, abandoning CRT in schools could negatively impact the mental health of white children. Stated simply, CRT calls for critical thinking. Critical thinking allows for the development of empathy, empathic conversations, and open and honest dialogues about race. Practicing empathy is important in building and maintaining secure social attachments, connections, and relationships.
In addition, social connection is predictive of individual mental health while disconnection leads to isolation, depression , and anxiety . Practicing empathy improves the ability to skillfully manage and respond to an emotional experience . Thus, by being empathic , and focusing on the experience of others, an individual becomes equipped to handle stressful or emotionally challenging situations.

A Step Toward Dismantling Racist Systems
Thus, CRT teaches children the tools they need to recognize white supremacy as an ideology that is built into our systems, versus imparting children with feelings of guilt or shame .
Rather, critical thinking skills empower white kids to challenge, change, and dismantle racist systems while enhancing their ability to form meaningful, healthy, and lasting connections with their peers. If Black children are old enough to experience racism, white children are old enough to learn about it, and both will benefit mentally and emotionally from having this type of open, honest, and critical dialogue.

Amanda Fialk, PhD, LCSW, LICSW , is Partner and Chief of Clinical Services at The Dorm, a young adult treatment community committed to helping young people launch fulfilling and independent lives.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience

Climate change and mental health: How extreme heat can affect mental illnesses
Assistant Professor of Geography, University of Waterloo
Disclosure statement
Peter Crank does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
University of Waterloo provides funding as a founding partner of The Conversation CA.
University of Waterloo provides funding as a member of The Conversation CA-FR.
View all partners
During heat waves, hospital admissions for mental health spike . The past 10 years were the hottest on record , and as we prepare for another scorcher of a summer, it’s time to take steps to increase our preparedness for extreme heat.
The potential for heat stress, heat exhaustion and heat stroke are well known hazards of extreme heat . Yet, physical health is not the only factor to consider under extreme heat; mental health can also suffer. Many people can relate to the sleepless nights during hot summer months , as well as anecdotal experiences of irritation and aggression when thermally uncomfortable.
But for those living with mental illnesses, the hazard of extreme heat is more dire than temperamental responses to day-to-day disruptions. From my research in Phoenix, Ariz. and the work of others during the 2021 heat dome in British Columbia, we know that the heat is exacerbating existing mental illnesses, increasing likelihoods of hospitalization and even death under warmer conditions for people with schizophrenia.
The interactions between environment and health are increasingly identified by researchers as public health concerns as air and water quality issues, as well as death tolls from heat , make headlines. Research has shown that lower socioeconomic groups, racialized people and the unhoused , are at greater risk of exposure to hotter conditions, while older adults are more vulnerable to hotter conditions.
Heat and mental illness

The relationship between mental illness and temperature has only recently been quantified as medical records and understanding of mental illnesses have improved. My work as an urban climatologist focuses on the impact of urbanization and heat on human health. I explore the variety of unexpected impacts of heat on people. Specifically, I’ve studied the population diagnosed with schizophrenia.
Schizophrenia is a mental illness that disrupts transmission of information to the brain. The part of the brain most impacted also houses our thermoregulatory functions . It’s the part that tells us we’re too hot and to start sweating or we’re too cold and should shiver to stay warm.
So those with schizophrenia aren’t able to respond to extreme heat the way the general population does; their bodies aren’t telling them to take precautions. Further, the medications used to address schizophrenia also raise core body temperature. This means that when taking the medication, people with schizophrenia are closer to the thresholds for heat stress and stroke than the general population.
In studying hospitalizations for schizophrenia in Phoenix (where summertime overnight low temperatures are, on average, at 30 C) between 2006 and 2014, I found that minimum air temperature (the overnight low temperature) has a significant relationship to the number of hospitalizations for schizophrenia on that day and the following day. Around three per cent of all schizophrenia hospitalizations during that time period can be attributed to the overnight low temperature.
The risk is highest in both extremely cold (lower than 3 C) and extremely hot conditions (higher than 30 C). These hospitalizations cost the Phoenix health-care system over US$2 million (in 2024 USD). Certainly, Canadians see much colder conditions than 3 C at night but rarely experience overnight lows above 30 C; however, the 2021 heat dome resulted in over 600 deaths in B.C. and researchers found that schizophrenia was the chronic condition most associated with risk of death during the extreme heat .
Extreme heat can have devastating impacts on those living with mental illness, our health-care system and our communities.

Schizophrenia is not the most common mental illness in Canada. However, it can serve as an example of how environmental issues can affect mental illness. One in every five Canadians experiences a mental illness each year . More than 250,000 Canadian youth experience major depression and systemic inequities exacerbated by disparities in treatment and care for those experiencing mental illness.
While there are many different factors potentially contributing to mental illness, heat plays a pervasive role in a wide range of mental health issues . Taking what steps we can to reduce this burden on those living with mental illnesses may also have knock-on benefits to the rest of society, such as reduced use of hospital emergency departments during heat waves.
Coping with climate change
So if climate change is continuing to bring hotter summers, what can be done to prevent these hospitalizations and deaths? There are measures that have broader benefits in addition to improving mental illness outcomes during extreme heat.
A common first step is ensuring access for all Canadians to air conditioning. Statistics Canada highlighted the importance of air conditioning for vulnerable populations . Warming conditions mean parts of Canada that didn’t need air conditioning 30 years ago can now become oppressively hot inside buildings without proper cooling .
Yet, air conditioning is dependent on the electrical grid and continues to produce waste heat and greenhouse gas emissions. There is a better way: designing our cities to be greener. There are a lot of previously known benefits to greening cities; reducing the urban heat island , improving air quality and in some cases increasing property values (both positive and negative outcomes).
Read more: Residential green spaces protect growing cities against climate change
However, there are some mental health benefits too. I contributed to a review of urban greenery mitigation science and highlighted the mental health benefits, including reduced depression, irritation and aggression.
Urban green space has been shown to improve mood, self-esteem and even speed up recovery from illness . So as the temperature spikes and you switch on the air conditioning and reach for the cold drinks, remember there are impacts to us all beyond just physical health, and pause to note how the heat is influencing your mood.
Extreme heat will continue to impact Canada (and increasingly so as the climate changes). However, the negative impacts on the most vulnerable, including those living with mental illness can, in part, be reduced by taking steps to ensure our cities are benefiting us all.
- Climate change
- Mental health
- Schizophrenia
- Mental illness
- Hot weather
- Extreme heat

Data Manager

Research Support Officer

Director, Social Policy

Head, School of Psychology

Senior Research Fellow - Women's Health Services

IMAGES
VIDEO
COMMENTS
Relationship Between Critical Thinking and Mental Health. Associating critical thinking with mental health is not without reason, since theories of psychotherapy have long stressed a linkage between mental problems and dysfunctional thinking (Gilbert, 2003; Gambrill, 2005; Cuijpers, 2019).Proponents of cognitive behavioral therapy suggest that the interpretation by people of a situation ...
Associating critical thinking with mental health is not without reason, since theories of psychotherapy have long stressed a linkage between mental problems and dysfunctional thinking (Gilbert, 2003; Gambrill, 2005; Cuijpers, 2019). Proponents of cognitive behavioral therapy suggest that the interpretation by people of a situation affects their ...
The science behind critical thinking is rooted in various cognitive processes, including perception, memory, attention, and problem-solving. It involves the prefrontal cortex, the part of the brain associated with complex cognitive behaviour, decision-making, and social behaviour. A strong capacity for critical thinking implies that these ...
Our mental health can affect factors like: Your self-esteem and self-worth. The way you socialize with others. The way you find meaning and value in your life. Your psychological functioning as it ...
In recent decades, approaches to critical thinking have generally taken a practical turn, pivoting away from more abstract accounts - such as emphasizing the logical relations that hold between statements (Ennis, 1964) - and moving toward an emphasis on belief and action.According to the definition that Robert Ennis (2018) has been advocating for the last few decades, critical thinking is ...
Introduction. Anxiety disorders are a major worldwide health problem with sizeable psychological, social, and economic costs (Beddington et al., 2008).The impact of anxiety on cognitive function is a major contributing factor to these costs; anxiety disorders can promote a crippling focus upon negative life-events and make concentration difficult, which can lead to problems in both social and ...
Introduction. Mental health literacy refers to beliefs and knowledge of lay individuals about mental health problems/disorders and their treatment. It is identified by how lay individuals recognize and manage their specific disorders as well as estimate their outcomes and prognoses. 1 Mental health is, to date, considered a neglected area in ...
Furthermore, the relationship between critical thinking and mental health was mediated by motor impulsivity (acting on the spur of the moment) and non-planning impulsivity (making decisions without careful forethought). These findings provide a preliminary account of how human critical thinking associate with mental health.
People cannot think critically unless they are aware of their cognitive biases, which can alter their perception of reality. Cognitive biases are mental shortcuts people take in order to process ...
How does mental illness affect cognition ... Critical thinking, planning, organization and problem solving are oftenreferred to by psychologists as the executive functions, because those are the skills that help you act upon information in an adaptive way. Take the example of cooking a meal.Even if you know how to cook each dish,to
For some people suffering from illnesses such as schizophrenia and substance use disorder - previously referred to as "substance abuse" - making the right choices can be extremely difficult. In fact, many mental illnesses feature problems with cognition (thinking and comprehension), including depression and bipolar disorder. Decision-making ability varies in healthy people, too ...
In our annual survey on the state of critical thinking, the Reboot Foundation asked people about their use of and views on social media, particularly as it related to their mental health. In the survey, our research team also asked questions about reasoning, media literacy, and critical thinking. Our goal was to take the temperature of popular ...
Find a therapist to overcome anxiety. Anxiety influences our perceptions, beliefs, reasoning, and ultimately our choices. The experience of anxiety hinders one's ability to view the situation ...
In this review, we will discuss the extent of, and mechanisms for, diet's influence on mood and cognition during different stages of life, with a focus on microglial activation, glucocorticoids ...
Depression can lead to alcoholism and suicide, but there's one lesser-known symptom of depression that people live with every day. Depression doesn't just get in the way of being happy. It can also interrupt your ability to think. It hampers your attention, memory and decision-making abilities.
Critical thinking is discussed in academics at all educational levels, although because of varying definitions some don't support the concept. In general, however, being able to critically think about new information is a good skill, especially as we get more and more inundated with information in our world.
Thinking and brain chemistry is a two-way street. While your thoughts influence your brain chemistry, your brain chemistry also influences your thoughts. For example, if you're thinking about ...
Here, we present an integrative framework for considering the role of affect generation and regulation in mental illness and well‐being. Our model views affect generation as an iterative cycle of attending to, appraising and responding to situations. It views affect regulation as an iterative series of decisions aimed at altering affect ...
At its most basic level, mental health is related to how we think and feel. It is the intensity or disproportionate reaction of those thoughts and feelings that can determine our level of mental health. According to the Centers for Disease Control and Prevention, mental health includes our emotional, psychological and social well-being, and affects how we think, feel and act.
Mindset has been studied for its effects on migraine, cancer, exercise activity, carpal tunnel surgery, chronic kidney disease, and many other conditions. So strong is the link between a healthy ...
According to the Substance Abuse and Mental Health Services Administration ( SAMHSA ), mental health affects multiple aspects of wellness, including: Emotional well-being. Psychological well-being. Social well-being. Although mental and physical health are often discussed as separate phenomena, they're actually quite intertwined, too.
Decades later at KFF, we did a survey with CNN on mental health in America in 2022. Scrolling through our findings, headlines jumped off the page. Ninety percent of the public believed there was a ...
Physical Effects. Testes constantly produce sperm. If you don't ejaculate it, the sperm becomes reabsorbed into the body. Some people are concerned that you will get "blue balls" if you don ...
Cognitive distortion is one such type of thinking process which can lead to anxiety, stress and other mental health issues. Cognitive distortion are thoughts which are not based on reality or ...
Critical thinking allows for the development of empathy, empathic conversations, and open and honest dialogues about race. Practicing empathy is important in building and maintaining secure social ...
CNN —. A new report details the role social media plays in the lives of young people, and how they manage the various pros and cons — including in the context of being a person of color or ...
Why the mental health crisis feels stuck. COVID forced us to talk — a lot — about Americans' deteriorating mental health. Four years later, the scale of the problem hardly appears to have gotten better, in large part because the system (perhaps unsurprisingly) remains ill-equipped to do much about it. Why it matters: The complexities of ...
Extreme heat will continue to affect Canada, but the negative impacts on the most vulnerable, including those living with mental illness, can be reduced by taking steps to ensure healthier cities.