An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Pregnancy Childbirth


Essential components of postnatal care – a systematic literature review and development of signal functions to guide monitoring and evaluation
Hannah mccauley.
1 Liverpool School of Tropical Medicine, Pembroke Place, L3 5QA UK
Kirsty Lowe
Nicholas furtado.
2 The Global Fund for Aids Tuberculosis and Malaria, Switzerland Geneva,
Viviana Mangiaterra
3 Bocconi School of Management, Bocconi University, Milan, Italy
Nynke van den Broek
Associated data.
Postnatal Care (PNC) is one of the healthcare-packages in the continuum of care for mothers and children that needs to be in place to reduce global maternal and perinatal mortality and morbidity. We sought to identify the essential components of PNC and develop signal functions to reflect these which can be used for the monitoring and evaluation of availability and quality of PNC.
Systematic review of the literature using MESH headings for databases (Cinahl, Cochrane, Global Health, Medline, PubMed, and Web of Science). Papers and reports on content of PNC published from 2000–2020 were included. Narrative synthesis of data and development of signal function through 7 consensus-building workshops with 184 stakeholders.
Forty-Eight papers and reports are included in the systematic review from which 22 essential components of PNC were extracted and used to develop 14 signal functions. Signal functions are used in obstetrics to denote a list of interventions that address major causes of maternal and perinatal morbidity or mortality. For each signal function we identified the equipment, medication and consumables required for implementation. The prevention and management of infectious diseases (malaria, HIV, tuberculosis) are considered essential components of routine PNC depending on population disease burden or whether the population is considered at risk. Screening and management of pre-eclampsia, maternal anaemia and mental health are recommended universally. Promotion of and support of exclusive breastfeeding and uptake of a modern contraceptive method are also considered essential components of PNC. For the new-born baby, cord care, monitoring of growth and development, screening for congenital disease and commencing vaccinations are considered essential signal functions. Screening for gender-based violence (GBV) including intimate partner- violence (IPV) is recommended when counselling can be provided and/or a referral pathway is in place. Debriefing following birth (complicated or un-complicated) was agreed through consensus-building as an important component of PNC.
Conclusions
Signal functions were developed which can be used for monitoring and evaluation of content and quality of PNC. Country adaptation and validation is recommended and further work is needed to examine if the proposed signal functions can serve as a useful monitoring and evaluation tool.
Trial registration
The systematic review protocol was registered: PROSPERO 2018 CRD42018107054 .
Supplementary Information
The online version contains supplementary material available at 10.1186/s12884-022-04752-6.
Postnatal Care (PNC) is one of the care packages that make up the continuum of care for mothers and babies globally [ 1 , 2 ]. A significant number of maternal deaths still occur during the postnatal period and an estimated 2.8 million babies die in the first month of life (neonatal death) [ 3 , 4 ]. Neonatal deaths account for up to 52% of all deaths in children under-5 years of age [ 5 ]. The majority of maternal and neonatal deaths are treatable and preventable with timely recognition and good-quality care [ 6 ].
Current guidelines advise that women should have at least eight ANC visits or contacts during pregnancy, a skilled attendant with adequate resources at the time of birth, and PNC immediately after birth and/or on at least four occasions in the subsequent six weeks [ 2 , 7 , 8 ].
Despite the critical importance of the postnatal period for both maternal and child survival and well-being, PNC consistently has the lowest coverage rates [ 9 ]. Postnatal care coverage is not a reported in the annual World Health Statistics reports and nor is it a component of the indicator to assess Universal Health Coverage (UHC). Estimates show that globally far fewer women and newborn babies receive PNC compared to antenatal care (ANC), with less than half of women receiving a postnatal care visit within two days of childbirth [ 10 , 11 ].
It is recommended that women who give birth with a skilled attendant in a healthcare facility receive immediate postnatal care and stay at the healthcare facility for at least 24 hours in case of uncomplicated birth [ 12 ]. However, it has been reported that even when women give birth in a healthcare facility, this may not include PNC as women may only stay at the healthcare facility for a few hours [ 13 ]. Of the 48% of women in sub-Saharan Africa who give birth without a skilled birth attendant only 13% receive a PNC visit [ 14 ].
The importance of PNC for reducing neonatal mortality has been documented with an estimation that if PNC rates were to reach 90% in sub-Saharan Africa, then 10–27% of all neonatal deaths could be averted [ 15 ]. Research has similarly outlined the considerable extent of maternal psychological and physiological morbidity following childbirth especially among vulnerable populations [ 16 , 17 ]. These include maternal anaemia, hypertension, puerperal and other infections as well as the need for increased psychosocial support. Timely identification and management during and after pregnancy can reduce the burden of disease and prevent complications particularly where morbidity and mortality levels among women of reproductive age are high [ 18 ].
In addition to the screening, identification, and management of pregnancy- and birth-related morbidity, the postnatal period and postnatal care package is an opportunity for the promotion and implementation of other components of public health, including the commencing of childhood immunisations, exclusive breastfeeding and uptake of modern contraceptive methods [ 1 ]. Care in the first 1000 days of life is crucially important to ensure that children survive and thrive. Children who are exclusively breastfed are 14 times more likely to survive the first six months of life than non-breastfed children [ 19 ]. Receiving PNC is significantly associated with modern contraception use [ 2 , 20 ].
PNC is also an important platform for programmes that aim to tackle the inequities in HIV, tuberculosis and malaria prevention and treatment [ 21 ]. For example, mother-to-child transmission of HIV (PMTCT) programmes provide treatment and education to HIV positive mothers and treatment for HIV-exposed infants with the aim of preventing newborn infections [ 22 ]. In high-burden settings, nearly half of all new HIV infections among children occur during the postnatal period. However, this is also when many women who are HIV positive fail to attend for ongoing care and treatment and drop out of such programmes. This means that comparatively more infant HIV infections occur during the postnatal period than during pregnancy and labour [ 23 ].
It is important that all components of PNC are provided to the mother and her baby in an integrated holistic manner. Given the low coverage rates and uptake of PNC globally, the attention internationally has been largely on supporting the implementation and uptake of at least the minimum number of PNC visits that are considered effective, and, on where and who can provide PNC at the healthcare facility level as well as in the community [ 24 ]. There has been less emphasis on the essential components or minimum content of the PNC care package required to meet the needs of both mothers and/or babies. Without the right content PNC will largely remain a ‘missed opportunity’. For other care packages that make up the continuum of care including for Emergency Obstetric Care and Antenatal Care ‘signal functions’ have been developed which reflect the essential components of a care package [ 25 , 26 ]. These have however not yet been developed for PNC.
We therefore conducted a systematic review of the literature and consensus-building workshops with a range of key stakeholders to identify the essential components of PNC and develop signal functions to assist in the monitoring and evaluation of availability and quality of PNC.
The PRISMA guidelines were followed for this systematic review and a narrative summary of results is provided [ 27 ]. The World Health Organisation (WHO) definition of postnatal period is ‘postnatal period begins immediately after the birth of the baby and extends up to six weeks (42 days) after birth’. When describing care provision, the postnatal period consists of immediate, early and late periods. The period from days 2 through 7 is defined as the early postnatal period and the period from days 8 through 42 as the late postnatal period [ 2 ].
The review protocol was registered (PROSPERO 2018 CRD42018107054).
Search strategy
A systematic search strategy was developed. Six databases including Cinahl, Cochrane (Cochrane Database of Systematic Reviews and the Cochrane Central Register of Controlled Trials), Global Health, Medline, PubMed, and Web of Science were searched using MeSH Headings, subheadings, thesaurus, and key word searches. A librarian was involved in developing MeSH terms and selecting relevant databases. Bibliographies from the articles selected for full text retrieval were reviewed to identify additional relevant studies. Key word searches were also conducted in Google Scholar. (Table S 1 - Search Terms).
Inclusion criteria
Articles from indexed journals describing one or more components of the content of PNC were included. As the researchers were English and French speaking, articles were limited to those published in English and French published between January 2000 (to coincide with the development of the postnatal care guidance from WHO) and September 2020.
Exclusion criteria
Studies that did not describe at least one content component of PNC were excluded. Studies were also excluded if they were case studies or research protocols. Finally, studies with no research methods such as journalistic style articles, editorials and individual volunteer accounts including personal reflection accounts were excluded.
Terminology
For this review, we used the term ‘component’ to denote individual interventions or actions that are considered part of the PNC care package. The terms ‘core’, ‘key’, ‘vital’ and ‘essential’ are used interchangeably in the literature. For the purpose of this review, we use the term ‘essential’ to denote a requirement for the PNC care package. In obstetrics ‘signal functions’ are used to denote a representative shortlist of key interventions and activities that address major causes of maternal and perinatal morbidity or mortality [ 25 , 26 ]. These were first used in obstetrics to define Emergency Obstetric Care with nine identified signal functions describing this care package. A list of signal functions does not include every service that may need to be provided but are considered as representative of a minimum essential care package that needs to be in place. The equipment, medication and/or vaccines required to implement each signal function can be identified and must be in place to be able to provide each relevant component of care.
Both the words ‘postpartum’ and ‘postnatal’ are used in the literature and in policy documents sometimes interchangeably. The WHO recommends the adoption of just a single term ‘postnatal’ to be used for all issues pertaining to the mother and the baby after birth up to 6 weeks (42 days) [ 28 ]. A distinction is made between ‘immediate postnatal care’ which is given immediately after birth and in the first 24-h after birth before discharge home (if birth is in a healthcare facility). Subsequent PNC is also referred to as ‘routine’ PNC visits and is recommended on at least three further occasions; day-3, days 7–14 and 6-weeks after birth [ 12 ]. This systematic review and developed signal functions pertain to routine PNC visits.
Study selection
Papers identified from the electronic searches were imported into Endnote and duplicates were removed. Three independent researchers reviewed all titles and abstracts to determine if papers met the inclusion criteria. Where inclusion/exclusion criteria could not be determined from the titles and abstracts alone and/or for papers without an abstract, full articles were retrieved and reviewed for relevance. In case of uncertainty or discordance between reviewers the full text was reviewed again by all three and consensus reached to include or exclude.
Quality assessment was undertaken on all included papers using The Hawker et al. Critical Appraisal Tool. The checklist is used to assess nine areas of the research article. The maximum score an article can score is 36 for fulfilling all the items on the checklist while a minimum score of 9 can be scored for a very poor article.
Data extraction
Using a pre-designed data extraction form, information for each study was extracted by two independent researchers to include type of study, population, and the individual components of PNC recommended or assessed. Any disagreement was resolved by discussion with a third researcher. Information obtained from studies that reported on more than one component of PNC was recorded in a central summary table. Studies that reported on only one component of PNC were summarised in separate tables by themes which were identified during review.
Data synthesis
A narrative synthesis was used to summarise findings. All identified individual components of PNC were listed and were categorised to develop a draft list of 25 signal functions with identification of the equipment, medication and consumables required to deliver each. A series of consensus-building workshops were held (3 international and 4 national) with a range of stakeholders (184 in total) including researchers, clinicians, health service managers from low- and middle-income countries (Afghanistan, Chad, Ghana, Togo, Nigeria) as well as high income settings (Europe, USA, UK) and key representatives from UN partners (UNFPA, WHO, UNICEF, and the Global Fund). Workshops were organised to allow for examination of each recommendation for content of PNC in small working groups followed by plenary discussion, consensus agreement leading to adoption or not of proposed content, signal function, equipment, medication and consumables required for each. Consensus-building workshops were conducted alongside and during the ongoing systematic review with evidence obtained from review of documents (policy, guidelines) and peer reviewed papers presented at time of the workshops. Adaptation or not of any component as discussed during any workshop was based on evidence where available with practices for which there was evidence of non-effectiveness or harmful practices agreed as needing to be discarded. After synthesis of all workshop feedback and the literature review a comprehensive list of 15 proposed signal functions were developed.
Description of studies
Database searches revealed 1213 potentially applicable publications. Duplicates were removed and abstracts reviewed. Exclusion and inclusion criteria was applied and 92 papers were included for full text review. After review 44 papers were excluded and 48 studies included in this review (Fig. 1 – Prisma Diagram). The main exclusion reasons were the policy or study papers were not reporting on content of PNC or were case studies.

Study selection- PRISMA Flow Diagram (Moher et al., 2009)
Of the 48 included papers 14 reported on multiple components of PNC. This included a systematic review [ 29 ], 6 sets of guidelines or policy papers [ 1 , 2 , 4 , 30 – 32 ] and 7 studies or non-systematic reviews [ 33 – 39 ]. (Supplementary Table 2 – Summary of Included studies reporting on multiple components of PNC).
All other papers included (34 papers) reported on only one single component of PNC and were subsequently grouped by 6 themes identified following review including (in order of number of papers included) mental health- postnatal depression (10) [ 40 – 49 ] breastfeeding [ 8 ], preventing mother to child transmission of HIV (PMTCT) (4) [ 50 – 57 ], family planning (3) [ 58 – 61 ], care of the pre-term newborn (2) [ 62 – 64 ] and Kangaroo Mother Care (KMC) (2) [ 67 , 68 ], maternal anaemia (2) [ 69 , 70 ] and Miscellaneous (3) [ 71 – 73 ] including screening for congenital hip dysplasia, and newborn hip screening and pelvic floor exercises. (Summary Tables available on request).
Quality assessment was performed on the 14 papers (Supplementary table 2 ), nine were graded as good quality and five assessed to be fair quality. The studies rated fair reported detailed study design methods but not the sampling methods and implications of the study, which compromised their quality. However, all included studies had areas of good quality making them suitable for data extraction.
Synthesis for papers reporting on single components of PNC
Mental health.
The largest number of included papers pertained to screening and management of maternal mental health and focused on Postnatal Depression (PND). Several papers report on the effectiveness and/or feasibility of introducing screening for PND. The introduction of screening in India (using the Edinburgh Postnatal Depression Screening- EPDS tool) immediately postpartum and at 6–8 weeks was found to be beneficial in identifying women at risk [ 40 ] as did a study in Ethiopia using the WHO self-reporting questionnaire [ 41 ]. Similarly, a study in Nepal reported highlighted the need for routine screening for PPD and reported that pregnancy complications and health problems in the baby were risk factors for PND [ 42 ].
A systematic review on the effectiveness of psychosocial assessment for the detection and management of PND concluded that assessment helps detect risk factors but those who screen positive and received prevention care for PND did not do better than those who screened positive and received no additional care [ 43 ].
A self-care programme consisting of two sessions covering physical and psychosocial wellbeing based on the teach-back method resulted in improved in quality of life during the postnatal period including with regard to improved positive feelings of the mother towards herself and towards her child as well as improved physical health [ 44 ]. Women in Australia who had received a short motivational interviewing intervention (including discussion of risk factors for PND, anxiety, low self-esteem) in the postnatal period were four times more likely to seek help for PND in the 12 months after birth [ 45 ].
In Iran, weekly support sessions provided by telephone over a period of eight weeks did not result in fewer women screening positive for PND using the EPDS [ 46 ] whereas in an RCT lifestyle-based education reduced anxiety and EPDS scores at six weeks postnatally [ 47 ]. Educational counselling in additional to routine care (debriefing) for women with adverse birth events did not result in better scores for quality of life, anxiety or depression at six weeks to six months postnatally [ 48 ]. Therapist-supported iCBT significantly improves stress, anxiety, and depressive symptoms among postpartum women with small to large effects [ 49 ].
Breastfeeding
Eight included papers reported on a range of approaches to support breastfeeding. An RCT in the UK examined the effect of skin-to-skin contact care versus none. Although initiation and duration of breastfeeding at four months was not improved, concerns regarding a drop in temp with skin-to-skin care were negated with good maintenance of temperature for the neonate. Both groups got breastfeeding education and support [ 50 ]. In a controlled intervention study in Turkey one-to one demonstration using models on how to breastfeed was more effective in preventing cracked nipples than providing an information brochure only [ 51 ]. Similarly, in Sweden midwives offered training and support to women at three days, three and nine months postpartum which was reported to result in women enjoying breastfeeding as well as a strengthened maternal relationship with the baby [ 52 ]. A one-hour workshop and one-hour counselling session in the first 24 h after birth was reported as effective and beneficial when breast feeding was assessed at four and eight weeks postpartum [ 53 ]. In the Gambia women who reported having received counselling, a supportive partner, from a more educated and wealthier background were more likely to intend to practice exclusive breastfeeding [ 54 ].
In contrast in another study in the UK support and education counselling after teaching the mother to position the baby herself there was no difference regarding whether the midwife provided further support or was ‘hands-off’ when breastfeeding was assessed at 17 weeks [ 55 ]. Evaluation of the effect of peer-to-peer counselling per telephone on breastfeeding duration showed no difference [ 56 ]. In an exploratory qualitative study, supporting mother-infant bonding increased the duration of breastfeeding in mothers with babies admitted to a neonatal intensive care unit in Malawi [ 57 ].
Diagnosis and management of HIV
A study from South Africa [ 58 ] highlighted missed opportunities for PMTCT with failure to attend for HIV treatment and FP, lack of TB screening, and women not receiving consistent messages and highlighted the need to address this. In Malawi the need for continued follow -up and care was highlighted through a cohort study with adherence to HIV treatment adequate for 73% or women during pregnancy, 66% in the first 3 months postnatally and 75% during months 4–21 postnatal [ 59 ]. The importance of early diagnosis and management of HIV infection in the neonate was demonstrated in Malawi and Thailand [ 60 , 61 ].
Family Planning (FP)
Offering FP as part of immediate PNC was associated with high rates of uptake in a study by Duncan et al. among HIV positive women [ 62 ]. In a large study from India women who had received a postpartum Intra uterine contraceptive device (IUCD) reported a high level of satisfaction and low level of expulsion (4% at 6 weeks) [ 63 ]. In an RCT in the USA contraceptive education by phone, insurance coverage and appointment scheduling did not influence the uptake or not of LARC [ 64 ].
Preterm and/or LBW babies
A Cochrane review by Mc Call et al. looking at thermo-regulation for preterm or low birth weight (LBW) babies reports that using plastic wraps or bags and/or thermo mattresses leads to higher temperature on admission to neonatal units (25 studies included) but that skin-to- skin care remains effective when compared to traditional incubator care [ 65 ]. Sun et al. recommend the use of a screening algorithm for the prediction of retinopathy of prematurity [ 66 ].
Prevention of hypothermia
An RCT demonstrated that helping mothers via one-on-one teaching and demonstration of skin-to-skin contact and Kangaroo Mother Care (KMC) improved mother to infant attachment and reduced maternal anxiety [ 67 ]. Nahidi et al. developed a mother to infant skin to skin contact questionnaire to improve implementation and factors associated [ 68 ].
Maternal anaemia
The importance of having guidelines for the management of anaemia was reported in a paper from New Zealand with a wide range of approaches noted among midwives especially regarding assessment of iron status [ 69 ]. Although two thirds (64.4%) of postnatal women had anaemia in a study from Uganda, the healthcare system had missed the opportunities to effectively address it, such as through the implementation of the policy recommendation for iron and folic acid supplementation [ 70 ].
Miscellaneous
A systematic review recommends the use of pulse-oximetry screening (POS) to check blood flow in the feet and hands during examination of the newborn baby in the immediate postpartum period for early detection of congenital cardiac heart disease. The reduction in neonatal morbidity and mortality is likely to be more pronounced in low-resource settings where most of these babies are born without a prenatal diagnosis. [ 71 ]. A systematic review to examine early dynamic ultrasound (eDUS) screening for hip instability in the first 6 weeks after birth suggests that this could be more effective than clinical examination alone [ 72 ]. A systematic review on the effect of pelvic floor muscle exercise reported that this improved sexual desire, arousal, orgasm, and satisfaction in the postpartum period [ 73 ].
Synthesis for papers reporting on multiple components of PNC [ 14 ]
Lassi et al. included 148 Cochrane and other systematic reviews which identified 61 RMNCH interventions which included eight for routine PNC including: prevention and management of anaemia in the mother, hygienic cord care, prevention of hypothermia with KMC for Low-Birth-Weight babies, newborn immunisation, breastfeeding, family planning, bed nets (ITN) for prevention of malaria, PMTCT for women who are HIV positive. Prevention and management of eclampsia was mentioned as part of ANC only. Home care was mentioned as an approach to delivery of PNC [ 29 ].
In a cross-sectional survey among 320 HIV positive postnatal women in Zambia, uptake of infant testing for HIV in the first six weeks was positively associated with maternal uptake of ARVs and, HIV status disclosure to the male partner. Women who reported intimate partner violence (IPV, 40% of the women included in the study) were less likely to have infants tested. Overall, 73% of infants had a test for HIV by 6 weeks. The paper highlights the importance of integration and linking of HIV prevention and management in both the mother and baby and the importance of screening for IPV during PNC [ 38 ].
A cluster RCT conducted in Ghana to assess effect of postnatal home visits vs routine PNC available at a healthcare facility and assessed breastfeeding (initiation and exclusive BF), thermoregulation (skin to skin contact, first bath delayed), sleeping under ITN, weighing of the baby and awareness of danger signs to identify the sick baby. Home visits were associated with improved coverage with increased care seeking at the facility in case the baby showed signs of illness (77% in intervention vs 55% in control) [ 33 ] .
A WHO Technical Working Group reviewed the evidence and reached consensus regarding indicators to assess coverage of key newborn interventions—on two additional indicators for care of the newborn in the immediate postpartum period including regarding; i) thermoregulation recommending drying, delayed bathing, skin-to-skin contact and checking temperature, and ii) cord care—keeping the cord dry versus application of 4% chlorhexidine -with the consensus being the latter needed further research. Additionally, weighing of the baby, breastfeeding and counselling on danger signs in the newborn were agreed as being essential components of PNC [ 34 ].
Several studies assessed the availability of quality of PNC. For a comprehensive healthcare facility assessment in Ghana components of (mainly immediate) PNC focused on the newborn and assessed- drying the baby after birth, delaying bathing the baby, prophylactic eye ointment for the baby, initiation of breast feeding, skin to skin contact and KMC for preterm and/or LBW babies [ 35 ]. In a before-after study to improve the uptake of intra-partum and postnatal care in Uganda components assessed for PNC included thermo-regulation for the newborn (immediate drying, external warming, skin to skin contact) promotion and provision of hygienic cord care early initiation of breastfeeding and KMC [ 39 ].
Two studies looked specifically at care provided in the community or home setting. A study in Iran reported on the effectiveness of community-based PNC which included uptake of PNC in the first week, weight gain during the first 3–7 days, hospitalization rate and management of the sick neonate mainly highlighting the importance of awareness of the danger signs and recognition of the sick baby [ 37 ]. Interviews exploring routine practices of home delivery and immediate PNC with women in Ethiopia assessed PNC components including tying the cord immediately after birth, dry cord care, bathing and cleaning the baby birth, and giving the baby water and sugar before initiation of breastfeeding (as non-recommended practice) [ 36 ].
Interventions identified to be essential in the postnatal period for the mother were described in 2011 by the Partnership for Maternal, Newborn and Child Health (PMNCH) and included family planning, prevention and treatment of maternal anaemia, detection and management of postpartum sepsis, PMTCT, immediate thermal care of the baby, initiation of exclusive breastfeeding, hygienic cord and skin care, KMC for preterm and LBW newborns and management of newborns with jaundice. These guidelines also highlighted the level and organisation of care required to provide PNC to women and their newborns [ 1 ].
In preparation for the Every Newborn Action Plan (ENAP) 70 indicators were assessed resulting in 10 core and 10 additional indicators being adopted; core indicators were considered those that impact the maternal and/or neonatal morality rate and/or stillbirth rate and include intrapartum skilled birth attendance, early PNC and essential Newborn Care. For PNC treatment of neonatal infections, chlorhexidine for cord care for babies at risk of complications and KMC were identified as essential [ 31 ].
The latest WHO Guidelines specifically for PNC [ 2 , 12 ] address the timing frequency place and content for PNC during the 6 weeks after to birth for mothers and babies and were developed on all available evidence focused on LMICs. Recommended content includes newborn examination, exclusive BF, cord care, delay in bathing, mother and baby staying together, immunisations, examination of the mother (general wellbeing micturition – urinary incontinence, bowel function, perineal care, headache, fatigue, back pain, uterine tenderness and lochia), iron and folic acid supplementation to prevent or manage anaemia in the mother.
Global guidelines for pregnancy, childbirth, postpartum and newborn care include recommendations regarding screening and management of pre-eclampsia and eclampsia; prevention of mother-to-child transmission of HIV; HIV and infant feeding; post-partum depression, and post-partum family planning [ 12 ]. The guidelines provide evidence-based recommendations including for the management of endemic diseases like malaria, HIV/AIDS, TB and anaemia. The PNC guidelines recommend administration of Vit K to the newborn and thermal regulation.
The main objective of Salam et al.’s paper was to review the evidence-base for interventions that have a proven positive impact on newborn and maternal health outcomes. In this non-systematic review, for PNC interventions that impacted positively on maternal and neonatal morbidity and mortality included education and provision of family planning, early initiation of and support for exclusive breastfeeding; thermal care or KMC for preterm and/or LBW babies, and hygienic skin and umbilical cord care after birth [ 30 ].
In the UK, NICE guidelines [ 32 ] outline the care that should be given to women and their babies up to eight weeks after birth. Individual components of clinical care include (but are not limited to) monitoring of blood pressure in the mother, cord care in the baby, administration of Vit K, breastfeeding support. These guidelines also highlight the need to listen to women, be responsive to their needs, taking into consideration the individual needs and preferences of each woman and debriefing after birth.
Essential Components of PNC and development of signal functions.
From the included papers a total of 22 components of PNC identified as essential were extracted. Results are presented in Table Table1 1 – Components of PNC identified and number of papers supporting each component.
Components of PNC identified and number of papers supporting each component
Peer review and consensus building workshops validated, detailed, and grouped the components which were then developed as developed as proposed signal functions of PNC (Table 2 - Proposed signal functions for PNC with components and outline of required equipment, medication and consumables). Screening for and management of tuberculosis although not identified by the systematic review of the literature was considered a vital and essential component of PNC across all consensus-building workshops along with screening for and management of HIV.
Proposed signal functions for PNC with essential content and components to be assessed and outline of required equipment drugs and consumables
a Assumes availability of essential consumables such as non-sterile gloves, needles, syringes or capillary tubes, skin swabs, tourniquet and cotton wool.
b All drugs as per national protocol – can vary and needs to be specified for each country.
Throughout the workshops it was highlighted that drug regimens for treatment and prevention of malaria, tuberculosis and HIV should be setting specific and dependent on country practice and policy. Hepatitis B vaccination of the newborn baby is now almost universally recommended but may depend on a country’s national policy and incidence or disease and/or identification of at-risk population. Workshop participants agreed that the proposed PNC signal functions could be used as an important monitoring and evaluation tool including for healthcare facility assessments e.g., to identify the number of healthcare facilities across all levels of care that can provide each of these components and also identify barriers to implementation e.g. lack of human resources, drugs, consumables and equipment The signal functions can also be used as an assessment of service delivery e.g., identification of the proportion of women who received each component during an PNC visit or contact.
Main findings
As a result of a systematic review of the literature 22 essential components of postnatal care (PNC) were identified of which 12 relate directly to the mother and 10 to the baby. These were synthesised and, following consensus-building with a wide range of stakeholders, were developed into 14 proposed signal functions with the identification of the required equipment, drugs vaccines and consumables to implement each component. As for other care packages in the continuum of care for mothers and children, signal functions of PNC can be used to guide monitoring and evaluation of PNC availability and quality.
We note that in the peer-reviewed literature, guidelines and policy documents the focus has frequently been on components related specifically to neonatal rather than maternal health care. This may be in response to the comparatively high burden of global perinatal and neonatal mortality. However, the health of the baby is directly linked to that of the mother. PNC seeks to address the well-being and health needs of both the mother and her baby during one combined visit or consultation. The proposed signal functions highlight this and do not make a distinction between those that are for the baby and those that are more specifically for the mother. The identified essential components and signal functions include prevention recognition and management of general wellbeing, obstetric complications, medical and infectious diseases that are prevalent as well as social and mental health. Postnatal care is also an important platform to promote exclusive breastfeeding and family planning. It is expected that these essential components of PNC are provided as ‘routine’ for women and babies in the postnatal period to support an optimum recovery for the mother, growth and development of the newborn baby and promote health seeking behaviour for the family. Adaptations can be made where needed depending on the burden of disease in any particular setting and emphasis of focus e.g., for the signal functions pertaining to malaria, TB and HIV. Guidelines for practice will depend on the estimated overall incidence in the population served.
Strengths and limitations
Postnatal Care is provided as two separate care packages 1) immediate postnatal care at the time of birth and 2) subsequent postnatal care. Postnatal care immediately after birth (in the first few hours) could more logically be considered part of the skilled birth attendance care package or part of intra-partum care and has been described as including prevention of postpartum haemorrhage through active management of the third stage and resuscitation of the newborn if required. Secondly, the care a woman and her baby require at the time of birth and/or immediately after this is very much dependent on the type of birth (vaginal or operative) and whether there are any complications for either the mother or her baby, making it more difficult to define a ‘standard’ or routine care package that would be applicable to all women and babies during the subsequent postnatal period which is commonly defined as the first 42 days after birth.
To the best of our knowledge this is the first systematic review examining specifically what should be considered as the essential content of PNC for the mother and baby to be provided in the first six weeks following birth. The included components are those that are considered part of a comprehensive care package for all women and babies i.e. as part of ‘routine’ PNC. For women and babies with specific complications or underlying morbidity additional PNC components will be required.
Context in relation to other studies
There is still relatively scant epidemiological information on the specific pregnancy-related burden of disease in the postnatal period. However, this is recognised as a period of risk as well as opportunity for screening, prevention, and management of health problems and to support the wellbeing of the mother and baby. There is emerging evidence that in low-and middle- income settings the burden of morbidity is significant [ 16 , 17 ]. In high-income settings where the burden of disease is smaller, the emphasis of PNC provision has more recently been on ensuring general well-being of the woman and her baby. This includes and emphasis on social and mental health and debriefing after either complicated or uncomplicated birth, rather than on prevention and management of pregnancy complications or infectious diseases.
For the purpose of developing globally relevant signal functions and, based on the results of our systematic review of the literature, the signal functions proposed in this study seek to be comprehensive and recognise the need to address three major infectious diseases (HIV, tuberculosis and malaria) as well as obstetric conditions, medical conditions, mental and social health. For those populations with a low prevalence of HIV, tuberculosis and/or malaria country adaptations can be made. It would be helpful to have agreed international cut-off points of prevalence above which screening for, and management of certain infectious diseases should be included as essential components of PNC. A useful comparison is the recommendations regarding whether or not to screen for tuberculosis as part of antenatal care which is guided by estimated country level prevalence of tuberculosis [ 8 ]. Screening for HIV is almost universally recommended as part of ANC and may not have to be repeated as part of PNC in countries with a low prevalence.
Examination of the baby to check for any congenital abnormalities and/or illness is an important part of PNC. In many settings an anomaly ultrasound scan is routinely offered as part of ANC. Whether or not this is provided, it remains important to ensure a full body examination of the baby as part of PNC. In high income settings additionally laboratory testing is carried out (e.g. a Guthrie or ‘heel prick’ test to check for phenylketonuria) and a routine hearing test is carried out on all newborn babies to identify deafness.
Discussion regarding the need for and/or effectiveness of de-briefing after traumatic birth as well as general de-briefing and information sharing after uncomplicated birth have informed the development of the relevant proposed signal function and was recognised by stakeholders during consultation to be a new and emerging component of PNC which requires further attention [ 74 , 75 ].
We conducted an earlier and separate systematic review and consensus-building to identify the essential components of ANC with the development of 15 proposed signal functions [ 26 ]. We note that there is an overlap in content and therefore the signal functions developed for both ANC and PNC and we recommend these are combined for the purposes of monitoring and evaluation as well as training of healthcare providers. In most setting ANC and PNC are provided in similar settings and by the same cadres of healthcare providers including for the main part community- and/or facility-based nurse-midwives.
Implications for policy and practice
It is recognised that PNC is being delivered by a wide range of healthcare providers, including those at facility- and community-level. For a full content of effective PNC to be delivered these healthcare providers need to have the necessary equipment, dugs, consumables as well as up-to-date knowledge and skills in all aspects of PNC. As it can be expected that many women are home-bound especially in the early postnatal period, there is a need to provide care at home or very close to home and models for this may require further development [ 76 ]. Recently there have been suggestions that community-based healthcare workers and/or volunteers may be better placed to provide PNC. However, an initial mapping shows that few of such cadres are adequately trained for, competent in, legislated and supported to provide all of the essential components of either ANC or PNC [ 77 ]. Other forms of community support are effective such as mother to mother support for continuation of exclusive breastfeeding, practical and emotional support from partners, family and the wider community to enhance wellbeing and promote a positive experience of the postnatal period [ 78 , 79 ].
The importance of screening for social (including gender-based violence) as well as mental health problems (including depression) during the antenatal as well as postnatal period is recognised globally [ 17 , 80 ]. A variety of screening tools is available currently to assess wellbeing and mental health and it will be important to establish which is most effective and feasible to use in each specific setting. In some cases, translation into a local language and/or socio-cultural adaptation of tools is still needed. However, our systematic review highlighted several studies from countries where such screening has now been successfully introduced. Screening for GBV and/or intimate partner violence (IPV) is problematic in many settings and not accepted practice either for the healthcare provider or the woman attending for care [ 81 , 82 ]. WHO guidelines for ANC recommend screening for GBV/IPV in settings where women can receive care and a referral pathway is established [ 8 ]. However, although recommended practice, we note that the current WHO guidelines for PNC make no specific recommendation regarding GBV [ 12 ].
Future research and unanswered questions
PNC coverage is defined as the number of women aged 15–49 years with a live birth who have postnatal contact with a health-care provider within two days of birth as a proportion of the total number of women aged 15–49 with a live birth. This information is collected from Demographic Health Surveys (DHS), Reproductive Health Surveys (RHS), Multiple Indicator Cluster Surveys (MICS), or other types of household surveys that collect data using nationally representative population samples and standardised questionnaires. Population-based household surveys are the preferred data source in settings that have a low utilization of healthcare facility services. However, such surveys are generally expensive and may be difficult to conduct.
The availability and uptake of essential health services coverage (SDG indicator 3.8.1) is an important measurement [ 83 ]. Thus, the Universal Health Coverage (UHC) index includes 16 essential health services as indicators of the equity and level of UHC. For reproductive, maternal, neonatal and child health (RMNCH) these are: family planning, antenatal care, delivery care, full child immunisation, and care for pneumonia in children [ 83 ]. We note that unlike ANC coverage, PNC coverage is not reported as an indicator in the annual World Health Statistics reports.
The available indicators for PNC are obtained for populations through a variety of different data sources, the most important of which are household surveys. Regarding PNC coverage, in both the MICS and DHS what is measured is; 1) the proportion of women who recall having received PNC within 2 days of giving birth and 2) who (which type of healthcare provider) provided PNC. Since 2013, in DHS (phase 7) what is asked is: did the woman receive PNC in the 2 days after birth, who provided this and where. For content what is included is: if the healthcare provider examined the cord, measured the baby’s temp, counselled on danger signs and observed breastfeeding [ 84 ] .
Given the importance of PNC as a key healthcare package for the prevention and management of morbidity and mortality in women of reproductive age and in the newborn, it will be important to reach global consensus on more effective routine monitoring of PNC coverage and content. The signal functions developed could be used: 1) for health facility assessment; 2) to identify health system barriers to implementation; 3) as a component of the service delivery assessment and, 4) for assessment of quality of care. Further research regarding the acceptability and feasibility of the application of the signal functions proposed in this study for the effective monitoring and evaluation of availability and quality of PNC is needed.
Globally the proportion of mothers and babies who receive PNC is significantly lower than those who receive ANC and this constitutes a missed opportunity. Reasons for this could be that PNC is not accessible, not available and/or not of good quality. The focus has to date been mainly on the number and timing of PNC visits rather than what is provided to the mother and baby during these visits or contacts. More attention should be given to content if PNC is to have the required impact on maternal and neonatal morbidity and mortality. We propose a set of signal functions that could be used to monitor and evaluate content of PNC. There is ample evidence for the urgent need to address aspects of care that are disrespectful and of poor quality and that are likely to contribute significantly to the current low uptake of postnatal care globally. Similarly, without the required essential content for the mother and her baby quality of care cannot be provided.
Acknowledgements
We would like to thank all the participants of the workshops for their considered inputs. In addition thanks to Dr A Miller and Dr A Traore for support with screening of papers.
Abbreviations
Authors’ contributions.
HMcC, KL and NvdB conducted the systematic review. HMcC, VM, NF and NvdB facilitated consensus building workshops. All authors (VM, NF, HMcC, Kl, NvdB) contributed to the analysis of the data and writing of the paper. The author(s) read and approved the final manuscript.
The Global Fund for Aids Tuberculosis and Malaria (GFATM).
Availability of data and materials
Declarations.
None declared.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Hannah McCauley, Email: [email protected] .
Kirsty Lowe, Email: moc.liamtoh@ewoL_ytsriK .
Nicholas Furtado, Email: [email protected] .
Viviana Mangiaterra, Email: [email protected] .
Nynke van den Broek, Email: moc.tenretnitb@keorbdvn .
Language selection
- Français fr
Chapter 5: Postpartum Care
- Previous Chapter
- Table of Contents
- Next Chapter
Download in PDF format (5.54 MB, 85 pages)
Organization: Public Health Agency of Canada
Date published: 2020-12-16
Related Topics
- Chapter 5 Fact sheet: Family-Centred Postpartum Experience
- Chapter 5 Infographic: Postpartum Health in Canada
- Family-Centred Maternity and Newborn Care: National Guidelines
- Fact sheets and infographics: Maternity and newborn care
Acknowledgements
Introduction, 1.1 cultural considerations, 1.2 caring for indigenous women, newborns and their families, 1.3 caring for lgbtq 2 families, 2.1 integrated care of the mother and baby, 2.2 care of the mother, 2.3 care of the newborn, 3.1 hospital births: length of hospital stay, 3.2 care of the mother, 3.3 care of the newborn, 4.1 postpartum mental health, 4.2 late postpartum hemorrhage, 4.3 infections, 4.4 cardiovascular and hypertensive disorders of pregnancy, 4.5 extensive perineal tears, 4.6 female genital mutilation/cutting (fgm/c), 4.7 diastasis of the rectus abdominis muscle, 4.8 gestational diabetes mellitus (gdm), 4.9 thyroid conditions, 4.10 symphysis pubic dysfunction, pelvic girdle pain and diastasis symphysis pubis, 4.11 assisted vaginal birth, 4.12 urinary/fecal incontinence, 4.13 prolonged stay in hospital, 5.1 infections, 5.2 cardiorespiratory distress and cardiac concerns, 5.3 hypoglycemia, 5.4 prenatal antidepressant use, 5.5 small-for-gestational-age babies and macrosomia, 5.6 substance use – neonatal abstinence syndrome/neonatal adaptations syndrome, 5.7 late preterm babies, 5.8 assisted vaginal birth, 5.9 anomalies or rare conditions, 5.10 prolonged stay in hospital/neonatal intensive care unit (nicu), 6.1 systems to follow families postpartum, 6.2 ongoing postpartum care of the mother and baby, 6.3 intimate partner violence and child abuse, 6.4 mother's nutrition and healthy weight, 6.5 sexuality and contraception, 6.6 immunization, lead author, georgia hunt, md.
Assistant Head, Quality Department of Family Practice BC Women’s Hospital Vancouver, British Columbia
Contributing Authors
Angela bowen, rn, phd.
Professor College of Nursing University of Saskatchewan Saskatoon, Saskatchewan
Christina M. Cantin, RN, BScN, MScN, PNC(C)
Perinatal Consultant Champlain Maternal Newborn Regional Program Ottawa, Ontario
Beverley Chalmers, DSc(Med), PhD
International Perinatal Health Consultant Kingston, Ontario
Kimberly Dow, MD, FRCPC
Professor Department of Pediatrics Queens University Kingston, Ontario
Louise Hanvey, RN, BScN, MHA
Senior Policy Analyst Maternal and Child Health Public Health Agency of Canada Ottawa, Ontario
Faiza Khurshid, MBBS, FCPS, MSc(HQ)
Assistant Professor, Department of Pediatrics Queen's University Medical Director, Division of Neonatal-Perinatal Medicine Kingston Health Sciences Centre Kingston, Ontario
Céline Lemay, SF, PhD
Senior lecturer Bac en pratique sage-femme Université du Québec à Trois-Rivières Trois-Rivières, Québec
Tracy Lovett, RN, BScN, MN, IBCLC
Maternal Child Health Nurse Coordinator First Nations and Inuit Health Branch, Atlantic Region Indigenous Services Canada Halifax, Nova Scotia
Lynn M. Menard, RN, BScN, MA
Team Leader Maternal and Child Health Public Health Agency of Canada Ottawa, Ontario
Simone Vigod, MD, MSc, FRCPC
Chief, Department of Psychiatry, Women’s College Hospital Associate Professor and Director, Department of Psychiatry, Faculty of Medicine, University of Toronto Shirley A. Brown Memorial Chair in Women’s Mental Health Research, Women’s College Hospital Toronto, Ontario
Carley Nicholson, RD, MPH
Policy Analyst Maternal and Child Health Public Health Agency of Canada Ottawa, Ontario
Lori E. Ross, PhD
Associate Professor and PhD Program Director Division of Social and Behavioural Health Sciences Dalla Lana School of Public Health, University of Toronto Toronto, Ontario
Roberta Stout
Research Associate National Collaborating Centre for Indigenous Health Prince George, British Columbia
The postpartum period is a significant time for the mother, baby, partner, and family. It is a time of transition and adaptation and is formative for everyone. There are physiological adjustments for both mother and baby, and significant social and emotional adjustments for the entire family.
Complex and finely tuned adjustments have physical and psychological benefits for the mother and her baby. It is important that everyone involved in the care of mothers and babies knows and acknowledges these benefits so that systems are planned and organized around the mother/baby unit and not around health care providers (HCPs).
The goals of care during the postpartum period are to:
- Support and promote the physical well-being of mother and baby and enable the mother to restand recover from the physical demands of pregnancy and birth;
- Support the developing relationship between the baby and their mother as well as the mother’s partner and family;
- Support the mother’s and her partner’s emotional and mental health needs;
- Support infant feeding;
- Support the mother’s confidence in herself and in her baby’s health and well-being, enabling her to fulfill her mothering role within her particular family and culture; and
- Support partners and other family members to enable them to develop confidence in their new role.
According to the principles of family-centred care, it is incumbent on HCPs to:
- Treat families with respect, dignity, and kindness, and learn about and respect their values and beliefs, using them to guide their care;
- Maintain open and ongoing communication with the woman and her partner/family;
- Plan the timing and purpose of each postpartum contact in partnership with the woman and her partner/family based on their individual needs;
- Provide culturally competent and safe care with cultural humility;
- Provide information and support in a timely fashion, according to the needs of the woman, her partner, and family. Ensure that information is evidence-based and accessible according to their culture, language, and abilities so that they can promote their own and their baby’s health and make informed decisions about their care and any necessary treatment.
Additional resources on postpartum care see Appendix A
1. Families with Special Considerations
Canadians are ethnoculturally diverse. Women from different cultures, whether Canadian-born or newcomers, may be influenced to a greater or lesser extent by their background.
HCPs will want to assess each woman’s background—if they are newcomers, their place of birth, how long they have been in Canada—and their support networks. Footnote 1 It is important to understand how the woman’s culture influences her unique needs, hopes, and postpartum expectations. Even when the necessary services are available and they are made aware of them, immigrant women may face language barriers and difficulties in access because of differences in cultural practices and expectations. Footnote 2
Most women who are newcomers to Canada face challenges of some sort: Footnote 2
- The Canadian health care system may feel foreign and strange, and they may have different expectations from those of their HCPs.
- They may not know about the available supports in the health care system.
- They may not share a common language with available HCPs, and their communities may not have access to culturally sensitive health care or translation services.
Each family is unique; they adapt their cultural traditions and practices to their own experience and needs, and they will interpret the parameters of the Canadian health care system within this context. As such, it is important to assess each situation individually. While HCPs may not always agree with certain cultural practices, respecting families’ needs and decisions is paramount. Listening to the women’s and families’ stories about their own culture, childbearing practices, and needs helps accomplish this approach. Footnote 1 Giving Birth in a New Land: Strategies for service providers working with newcomers suggests specific strategies that promote family-centred, culturally competent postpartum care. Footnote 3 HCPs can use these to engage in a dialogue with women and families and learn about their values and beliefs and how these apply to their situation.
Questions to Facilitate Communication about Values and Beliefs Footnote 1 Footnote 3
If families are newcomers to Canada, ask about their place of birth, how long they have been in Canada, and their support systems. To ensure that women have an opportunity to express their needs, helpful questions include:
- How is health care different in your homeland or culture?
- What do you and your family believe you should do to remain healthy postpartum?
- What are the things you do to improve your health and the health of your baby? What can’t you do?
- Do you have beliefs about caring for your baby and yourself that I need to know about?
- Do you have any practices and faith rituals to do with your role as a mother?
- Are there any specific foods that you might eat/drink (or prefer to avoid)?
- Are there any home remedies that you may use during the postpartum period?
- Who do you want involved in decision-making?
Adapted from Giving Birth in a New Land: Strategies for service providers working with newcomers (2014), and Maternal Child Nursing Care Canada (2017).
HCPs need to consider the personal values they bring to their relationship with families. Cultural competence includes working collaboratively with families and communicating effectively.
Communication with families from different cultural backgrounds involves not only translating words, but also understanding subtle variations in meaning, style, volume, and gestures. Footnote 1 As such, it is important to find the best possible interpreter for the specific situation. Interpreters must be trustworthy regarding access to private information and, ideally, have specific health-related language skills. Using children or other family members as interpreters is not recommended.
The history of residential schools and colonization, which caused the loss of traditional values and practices, languages, and family/community kinship, continues to affect Indigenous women, families, and communities. Indigenous Peoples have poorer health outcomes and higher rates of poverty, food insecurity, and unsafe and overcrowded housing. These social determinants of health take a toll on the physical, emotional, mental, and spiritual health of Indigenous women in Canada.
The health and well-being of many Indigenous women and families have been further undermined by racism, sexism, and culturally inappropriate or inaccessible health services—which also affect Indigenous women and their babies during the postpartum period. Footnote 4 Footnote 5 Footnote 6
Indigenous women in Canada are diverse in their culture, ancestry, beliefs, and practices. Each Indigenous community has its own traditions, values, language, and communication styles. Many Indigenous women want to incorporate their cultural and societal values and beliefs into their lives and parenting. Integrating cultural safety in the care of Indigenous women during the postpartum period involves providing an environment of respect and open communication, which is consistent with the principles of family-centred care. Indigenous women, as all women, need to feel safe in order to build a trusting relationship with their HCPs.
HCPs should engage with, and familiarize themselves with, the community and work with women to understand their individual values, beliefs, and needs. Footnote 7
An Indigenous doula can assist in honouring traditional and spiritual practices and beliefs associated with postpartum care and support the woman and her family’s language and cultural needs while providing emotional and physical assistance during pregnancy, labour, and the postpartum period. Footnote 8
Indigenous women may have to leave their communities to give birth in larger centres. Being away from their families and support systems affects their postpartum experience, including breastfeeding, and recovery. It is important to consider their needs and re-connect them with families and communities as quickly as possible.
Indigenous-specific postpartum and parenting programs are ideal—particularly group formats that allow Indigenous women to meet each other and develop supportive friendships during their pregnancies. Programs that support Indigenous fathers so that they feel equipped to help their partners and children are also necessary. Better systems of referrals and communication between different services and organizations would ensure continuity and comprehensiveness in care. Footnote 9
Training and Education of Healthcare Providers
There is a need for better training of HCPs on how to create culturally safe, stigma-free, and respectful care for Indigenous mothers, babies, and families during the postpartum period. Footnote 9 A nationwide survey of residents and program directors of all accredited obstetrics and gynecology residency programs in Canada demonstrated a lack of curriculum and a significant deficit in knowledge in Indigenous women’s health. Footnote 10 As a result, a nationwide curriculum initiative is underway for residents and other health care practitioners. This will facilitate the provision of education in Indigenous women’s health while decreasing the burden on individual programs.
Family-centred maternity and newborn care is based on individual needs and a mutually respectful and trusting relationship. While progress has been made in providing equitable health care to the LGBTQ 2 community Footnote * , these families often continue to face barriers in health care.
People in the LGBTQ 2 community identify 3 major barriers when dealing with the health care system—invisibility, lack of information, and negative beliefs. Invisibility refers to the fact that they do not see themselves in the institutions/programs—for example, the posters on the walls, the forms they complete—or in conversations with HCPs. The HCPs they encounter often do not understand their experiences as an LGBTQ 2 family, their unique and diverse needs, and may have negative beliefs about them. Footnote 11
Sexual minority women (including lesbian, bisexual, and other non-heterosexual women) have a greater prevalence of depression and depressive symptoms compared with heterosexual women, likely because of the impact of sexual orientation-based discrimination, stigma, lack of social support and exposure to additional stress due to heterosexism from their families and some HCPs. Footnote 12 Footnote 13 Footnote 14 Footnote 15 Footnote 16 Invisible sexual minority women (i.e., women who have a history of sexual relationships with women but are currently partnered with men) are at higher risk for postpartum depression than both visible sexual minority women (women partnered with women) and heterosexual women. Footnote 14 Footnote 17
Ongoing education for HCPs on the unique needs of LGTBQ2 families is essential to improving the health care LGTBQ2 families receive. Footnote 18 HCPs caring for LGBTQ 2 families will want to confront any negative beliefs they may have and aim for ease in approaching the topics of gender, sexuality, and families. It is important that HCPs reflect on their beliefs about LGBTQ 2 people and be willing to challenge these beliefs to develop their practice. Footnote 11
HCPs can facilitate inclusivity when caring for LGBTQ 2 families, including during the postpartum period, by: Footnote 11
- Paying attention to words and language. Words can empower people and they can hurt.
- Being aware of non-verbal communication and tone of voice—these express emotions and attitudes.
- Using non-biased, inclusive language and open-ended questions.
- Asking questions that express openness to all families—and not making assumptions about gender identity, sexual orientation, or behaviour.
- Making sure forms and questionnaires are inclusive.
- Ensuring that visuals, such as posters, in a clinic or program area signal acceptance of diversity.
- Posting a non-discrimination policy and communicating an environment of respect.
2. Postpartum Care Immediately After Childbirth (Birth to 2 Hours)
The mother and newborn should be considered a unit during the immediate postpartum period (0–2 hours). It is important to avoid disrupting this close relationship during these crucial few hours and to encourage skin-to-skin contact between the baby and the mother (or partner if the mother is unable). The International MotherBaby Childbirth Organization refers to this as motherbaby care to emphasize the importance of recognizing that mothers and babies are a unit.
The parent–baby bond—the first step in the baby’s subsequent attachments—is formative to a child’s sense of security and has long-lasting effects. Footnote 19 Having early physical contact with the baby can affirm parents’ sense of accomplishment and promote their self-confidence as parents. Keeping babies and parents together is of the highest priority. Institutional policies should only disrupt this contact in the event of a necessary, evidence-based medical reason.
All major organizations concerned with newborn health, including the Society of Obstetricians and Gynaecologists of Canada (SOGC), the Breastfeeding Committee for Canada, the Canadian Paediatric Society (CPS), the Canadian Association of Midwives, the American Academy of Pediatrics, the World Health Organization (WHO), and the United Nations Children’s Fund (UNICEF), recommend that healthy babies have direct skin-to-skin contact with their mothers immediately following birth. Skin-to-skin contact involves placing the newborn babies on their mothers’ bare chest immediately after she gives birth, covering the baby with a blanket, and ensuring that contact is uninterrupted for at least an hour or at least until the first feeding is completed or the mother wishes. Footnote 20 It is essential to prepare mothers for skin-to-skin contact before birth. Since some cultures may not practise this contact, information, encouragement and support are called for.
Being held by their mother helps the baby normalize his or her temperature, breathing, heart rate, and blood sugar and reduces the pain of medical procedures. Babies who have skin-to-skin contact interact more with their mothers and cry less than those who do not have this contact. Footnote 21 Footnote 22 Footnote 23 The vast majority of babies go to the breast within an hour of birth if they are kept skin-to-skin with their mother. Mothers are more likely to breastfeed in the 4 months postpartum and tend to breastfeed for longer if they have early skin-to-skin contact with their babies. Footnote 22 Nevertheless, skin-to-skin contact is important for all mothers and babies regardless of the mother’s decision about feeding. If the mother herself is unable to have skin-to-skin contact with her baby, she should choose another person to hold, warm, and comfort the baby, for example, her partner or another family member.
HCPs can demonstrate respect for the family by interfering as little as possible during interactions between the mother and baby. Observations, assessments, and interventions can be completed with minimal intrusion, while skin-to-skin contact is maintained. Anything that is not essential to the immediate well-being of the baby or mother can wait for 2 hours or after the first breastfeeding. Even medically necessary procedures can be done while the baby remains in skin-to-skin contact as long as it is medically safe to do so. Footnote 23 Footnote 24
Skin-to-skin contact should continue during transfer from the birthing unit to the postpartum unit or neonatal intensive care unit (NICU). Footnote 25 At this time, babies should be observed for abnormal respiratory effort, colour, activity or tone—signs of instability that call for urgent evaluation. Separating a mother from a baby requiring special care can make adjustment to motherhood more difficult, and HCPs are called upon to provide even more intensive support at such times. There are continued benefits to skin-to-skin contact past the immediate first few hours of birth, as well as benefits to initiating skin-to-skin contact later, if this was not possible immediately following birth. Footnote 23 Footnote 24 Footnote 26
In some Canadian and European centres, preterm babies stay with their parents during assessments, and couplet care is practised within the NICU. Footnote 27 Many centres are advocating for skin-to-skin contact, even of very preterm, ventilated, and low birth-weight babies, because of the clinical and psychological benefits to both baby and parents. Footnote 28
Family-Integrated Care in the Neonatal Intensive Care Unit
Recent Canadian research has found that a family-integrated care (FICare) model of care for preterm babies in neonatal intensive care units (NICU) is feasible and safe in the Canadian health care setting and results in improved weight gain by these babies. The FICare model of care, which is based on the original work of Dr. Adik Levin in Estonia, also has the potential to improve other short- and long-term outcomes for babies and families. Footnote 29
In this model, parents provide most of the care for their baby, while nurses and other HCPs guide and counsel parents. Footnote 29 Footnote 30 FICare is more than just the physical setting; the model recognizes that parents are the primary caregivers and decision-makers for their babies. FICare can be accomplished even in older units, and HCP teams are expected to adapt to that reality whenever possible.
Innovative examples of this model of care in Canada include the following:
- BC Women's hospital offers intensive care for newborns and postpartum care for mothers in the same room. Mothers are able to recover from vaginal or caesarean births and pump breast milk without leaving their babies. All newborn babies have their own sound-proofed rooms, and 12 of the 70 rooms are spacious mom-and-babyrooms equipped with a breast-pumping station, reclining chair, and hospital bed for the mother as well as an incubator and infant-monitoring machines. The mom-and-baby rooms are for babies born at 33 weeks or later at low risk of complications.
- In Nova Scotia, the IWK Health Centre is caring for mothers and babies together in their NICU. Each room has a full setup to care for a baby as well as a suite for the family to stay in. The family is given a double bed, a closet with a safe, and a private washroom with a shower. Babies are continuously monitored and, if an alarm is triggered, a signal is sent to a nurse’s smartphone. The rooms are also equipped with everything from milk fridges to special sinks that help families bathe their babies. Rooms without windows have skylights that mimic clouds in the sky, and every room has artwork.
In the event of a caesarean birth, it is important to provide all possible opportunities for immediate (defined as within 5 minutes) and uninterrupted skin-to-skin contact as well as breastfeeding when babies cue to feed. This can be done in the operating and recovery rooms. In fact, skin-to-skin care should be considered the norm for caesarean births in the operating room, decreasing the need for early supplemental feedings. Footnote 31
It is important to provide time alone for the family in those critical first hours, with opportunities for both parents to interact with the baby in the birth and recovery rooms. Parents should be encouraged to spend as much time as possible with their baby, including in the NICU, ideally while rooming-in together. If the woman’s partner chooses not to be present for the caesarean birth, the family should be re-united as soon as possible. Footnote 32
The immediate postpartum period is a time of joyful celebration for the vast majority of families, but it is also a time of considerable physiological adaptation for the mother—and for the baby. As such, careful observation and, at times, intervention is required.
Women have different responses on giving birth. Some feel excited, uplifted, and energetic. Others are exhausted and want to sleep. A woman’s response may depend on the length, difficulty, and pain during labour, blood loss, anesthesia/analgesia, complications, and whether she had an operative vaginal birth or caesarean birth. Another determining factor is the woman’s experience of labour and birth compared with her expectations of these events.
Physical adjustments in the immediate postpartum period—including blood loss, weight loss, and displacement of internal organs—require a significant expenditure of energy. Immediate postpartum care centers on the need for hydration, nutrition, and rest. It is a time to replenish energy.
Begin each postpartum contact by asking the woman how she feels, physically and emotionally, and identifying any concerns that she may have. The physical observation of the mother at each postpartum contact should be individualized and guided by her unique history and situation. The assessment can include the following, depending on the mother’s feelings, sensations, and expressed needs: Footnote 24
- Vital signs (temperature, pulse, respiratory rate, blood pressure);
- Uterine tone and condition of perineum;
- Bladder and bowel function;
- Breasts and nipples;
- Physical comfort;
- Emotional and psychological response to labour and birth, for the woman and her partner. Starting this conversation is particularly important in certain circumstances (e.g., when the baby is sick, the mother had complications, or the birth did not go as planned);
- Skin-to-skin contact with baby; and
- Learning needs.
Document the findings according to the institution’s policy.
Postpartum Hemorrhage
Postpartum hemorrhage is the most common complication in the immediate postpartum period. It affects approximately 6% of women globally and is the leading cause of maternal mortality worldwide. Footnote 33 In Canada, a diagnosis of postpartum hemorrhage was associated with 1.6 maternal deaths per 100,000 hospital births from 2002 to 2010. Footnote 34 From 2006 to 2010, it was the second most common severe maternal morbidity, at a rate of 465.4 per 100 000 hospital births. Footnote 34
Postpartum hemorrhage is defined as blood loss of more than 500 mL during vaginal birth or more than 1000 mL during caesarean birth. The primary cause of immediate postpartum hemorrhage is uterine atony. Other causes include uterine rupture, morbidly adherent placenta, and uterine artery extension/laceration during caesarean birth.
Refer to the Society of Obstetricians and Gynaecologists of Canada (SOGC) guideline Active Management of the Third Stage of Labour: Prevention and treatment of postpartum hemorrhage . Footnote 35
Postpartum hemorrhage has many implications for the woman, including orthostatic hypotension, anemia, fatigue, and fear—all of which affect her ability to care for herself and her baby. It may also result in a lack of immediate skin-to-skin contact with her infant and an increase in the risk of postpartum depression. A blood transfusion may be necessary, which has risks. Footnote 36 Footnote 37 Delayed, or secondary, postpartum hemorrhage (between 24 hours and 6 weeks postpartum), may occur after the woman and baby have been transferred to a postpartum unit or at home.
It is important to educate women of the signs and symptoms of concern relating to delayed postpartum hemorrhage before discharge and after a homebirth.
The baby’s transition to life outside the uterus involves:
- Establishment of effective respiration and circulation;
- Maintenance of an adequate body temperature;
- Contact with his/her mother and family; and
- Initiation of feeding.
The postpartum period is a critical transition time for the baby. This period requires thorough and ongoing assessment and monitoring. An initial, head-to-toe examination of the baby in the birthing area ensures that he or she is adapting to the extrauterine environment. This examination would also identify any abnormal clinical findings. These observations can be completed when the baby is skin-to-skin, which promotes intimacy while helping to maintain a calm environment.
Neonatal Resuscitation
The Neonatal Resuscitation Program (NRP) acknowledges that at least 90% of newborns are vigorous, term babies who do not need to be separated from their mothers for the initial steps of resuscitation. Care for these babies includes:
- Managing the umbilical cord (i.e., avoidance, where possible, of immediate clamping);
- Providing warmth by encouraging direct skin-to-skin contact, ideally with the mother;
- Drying the baby’s skin with a warm, dry towel, stimulating breathing, and repositioning the head to open the airway;
- Clearing mucus from the upper airway, if necessary, by wiping the baby’s mouth and nose; and
- Ongoing observation of breathing, heart rate, activity, and colour. Footnote 38
Refer to NRP guidelines for the management of specific clinical situations. Footnote 23 Footnote 39
HCPs obtain skills in neonatal resuscitation through NRP training coordinated by the CPS, which has set the educational standards for Canadian practice. The Society recommends that an individual trained in neonatal resuscitation be assigned to this role at every birth. The CPS also recommends that all personnel likely to care for babies at birth have training and registration at the Provider or Instructor level and undergo periodic re-registration. Footnote 39
While the primary care provider at the birth is responsible for the woman’s care, a second HCP should have the primary role of assisting the baby through transition – one able to provide positive pressure ventilation and perform chest compressions, if necessary. Footnote 38 Another person with the skills to perform a complete resuscitation (including intubation and chest compressions) should be readily available to assist. Footnote 38 Footnote 40
The CPS also advises that local/regional health authorities have in place a program that supports the implementation of current neonatal resuscitation guidelines, educational programs for HCPs involved in care during labour and birth, and policies that take into account the educational needs, roles, and responsibilities of professionals involved in care during labour and birth/care of the newborn.
Neonatal Stabilization
A proportion of newly born babies are identified as at risk or unwell during the minutes or hours following birth, often due to prematurity or poor cardiorespiratory transition. All delivering facilities and practitioners should have a plan that addresses these babies’ clinical needs (such as respiratory support or glucose management), communication with referral centres, and support of the family.
The CPS’s Acute-Care of at-Risk Newborns (ACoRN) program specifically addresses the needs of babies who are challenged by the transition to extrauterine life. Facilities may find this program useful in preparing for the possibility that a newborn is unwell or at risk.
3. Early Postpartum Care (After 2 Hours)
The key goals of early postpartum care are to:
- maintain and promote the health and well-being of mother and baby;
- support the mother in caring for herself and her baby;
- foster attachment between the baby and the mother, her partner, and other significant family members;
- support the physical and psychological adjustment of the mother and her partner, the baby, and the family; and
- promote effective feeding.
Every postpartum interaction should be carried out in accordance with the principles of family-centred care, basing care and support on evidence of individual needs and not routines.
The benefits of skin-to-skin contact continue through the early postpartum period, facilitating attachment, increasing the duration of breastfeeding, and decreased crying and expression of pain during procedures such as heel prick blood sampling. Footnote 23 Although no national guidelines on labour, birthing, and postpartum rooms exist, the Provincial Council for Maternal and Child Health (PCMCH) recommends that mothers who give birth in hospital have a spacious room, preferably a private one, where they can labour, give birth, and stay with their babies until discharged. Rooming-in 24 hours a day should be the norm for all mother–baby dyads unless there is a justifiable reason for separation. Footnote 20 As many interventions as possible should occur in the mother’s room to avoid separation. Admissions to nurseries should be based on established criteria and guidelines—and be the exception rather than the rule. Footnote 23
A personalized postpartum care plan should be developed in partnership with the mother and her family as soon as possible following the birth. It includes: Footnote 24
- the mother’s concerns and needs;
- important factors in the pregnancy, birth, and immediate postpartum period;
- assessment of infant feeding;
- the names and contact information of the professionals involved in the mother’s and baby’s care; and
- planned follow-ups/appointments with HCPs for mother and baby during the postpartum period.
The plan needs to be reviewed and adjusted with the mother and family after every postpartum interaction.
Each mother should be assigned an HCP who is responsible for coordinating the care of the family and their transition into the community. This HCP consults with others, as necessary, as the needs of the mother and baby evolve. When birth takes place in hospital or a birthing centre, it is critical that systems, policies, and protocols ensure families are discharged only after follow-up care in the community is established. Footnote 41 Footnote 42
Optimal family-centred care during the early postpartum period requires seamless continuity of care and information-sharing between HCPs. How this is accomplished depends on the type of provider and the jurisdiction. Successful coordination of early postpartum care depends upon clear communication between institutions, community HCPs, and families. Hospitals, birth centres, physicians, nurse practitioners, and midwives need a strategy to facilitate effective communication of health information as mothers and babies transition into the community. A comprehensive discharge summary or maternal–newborn passport program may be useful. Secure electronic communication facilitates this process. Footnote 43
The Breastfeeding Committee of Canada and WHO recommend assessing newborn babies for breastfeeding issues within 24 to 48 hours of discharge from a hospital/birthing centre with routine follow-up of all mothers within 48 hours of discharge; Footnote 20 Footnote 44 this care may be provided by the hospital, community health centre, a breastfeeding clinic, midwife, etc.
Most newborn care guidelines recommend that an HCP assess the mother and baby during the first week of life. Footnote 45 The American Academy of Pediatrics specifies that this assessment takes place 48 to 72 hours after discharge if discharge occurs less than 48 hours following birth. Footnote 46 The CPS states:
At time of discharge, infants must have an appropriate follow-up plan in place that includes: contact information for a primary health care provider; a scheduled follow-up visit 24 h to 72 h post discharge—in hospital, clinic or at home—with a qualified health care provider. Hearing and newborn screens have been scheduled (if they were not conducted in-hospital); appropriate follow-up for jaundice; vitamin D supplementation if breast-fed; other follow-up, as required. Footnote 45
Even though the same principles and philosophy of care underpin all postpartum care, postpartum services should be organized locally to maximize effectiveness and efficiency for women and their babies.
In 1993, the average length of stay after a vaginal birth was 3.2 days, decreasing to 2.0 days by 2012. Footnote 5 During the same period, the length of hospital stay following Caesarean birth decreased from 5.0 days to 3.4 days. The safety of a shortened hospital stay (averaging 2.2 days in 2017/2018 Footnote 47 ) has been debated with regards to the needs of the mother and particularly the newborn. What research says about shorter hospital stays can differ from various organizations’ guidelines for both mother and baby. Footnote 48 Footnote 49
Each family needs to discuss with their HCP the risks and benefits of a stay that is shorter than the institutional standard. Base this discussion on the baby’s and the mother’s needs and not on routine policies. From the perspective of family-centred care, leaving the hospital as early as possible has a number of potential benefits: the opportunity for the entire family to get to know the baby together, resulting in greater attachment; more involvement for the partner and less sibling rivalry; better rest and sleep for the mother in her own environment, without constant interruptions from hospital staff; reduced exposure of mother and baby to hospital-acquired infections; and greater confidence on the mother’s part in her ability to care for her baby. Footnote 49
A shortened hospital or birthing centre stay is favoured by: the physiological stability of the mother and baby; family readiness to care for the baby at home; and a greater level of community, family, and institutional support upon discharge. In all situations, including those where mothers and babies are discharged early, mothers need to understand the signs of potential problems. In addition, it is important that the family knows where and when the mother and baby will next see an HCP and who they can contact with any questions.
The Canadian Medical Protective Association (CMPA) recommends reviewing test results and looking for signs of postpartum complications (e.g., infection, hemorrhage, excessive pain, bladder distention, difficulty walking) before discharging the mother and baby. The family should receive clear written or verbal instructions describing the steps and precautions to take when there are concerns, as well as the symptoms or signs that indicate that further medical attention is necessary. Footnote 50
Women and families should be told about community programs for postpartum care and peer supports for themselves and their babies—what they are, where they are located, and how to access them. These may include home-visiting programs, clinics, community-based programs and telephone support. Since it may be difficult for new mothers to remember all of the information shared with them, it is best to provide written information and also make it available on the facility’s website.
Regularly reviewing communication and coordination mechanisms will help to ensure a consistent and effective transition into the community and follow-up for the mother, baby, and family. The question of how best to arrange mother and baby’s discharge is an opportunity to revisit institutional and community resources for new families.
Refer to the following CPS guidelines related to infant discharge:
- Facilitating Discharge from Hospital of the Healthy Term Infant
- Safe Discharge of the Late Preterm Infant
- Going Home: Facilitating discharge of the preterm infant
At-risk babies, including those born late preterm babies, or those who are low birth-weight, are at risk for multiple complications including poor feeding and weight gain, hypoglycemia, and jaundice. Discharge should only be considered once the baby is stable.
Care and support during the early postpartum period should enable the mother to take charge of her own health and that of her baby—and to become confident in her ability to care for herself and her baby. This assumes that she is an autonomous adult and that HCPs have confidence in her ability to be a partner in her own care. Her values, situation, and needs are unique.
The Mother’s Well-being and Needs
Begin each postpartum contact with the mother and family by asking the woman how she feels, physically and emotionally, and identify any concerns she may have. Topics to explore include her experiences with her baby, breastfeeding/feeding, how much rest she is getting, and any pain or discomfort she may be experiencing. A physical examination may be performed as needed. The mother’s care is aimed at maintaining her health and helping her adapt to her new role as a mother.
Women need information, advice, and reassurance about postpartum physiological adaptations—such as normal lochia, perineal healing, incision healing (following caesarean birth), and changes to the breasts and nipples. They also need information on any potential issues, such as infection, hemorrhoids, cramping, constipation, urinary incontinence, painful urination, perineal pain and hygiene, headaches, back pain, pain medication, anemia, late postpartum hemorrhage, separation of the abdominal muscles, and breastfeeding challenges. The emotional and social changes she is likely to experience as a result of becoming a parent also require discussion.
HCPs will want to provide clear and consistent information and advice that is tailored to the woman’s individual needs and concerns. If the woman has a partner, he or she is a central figure in the family and should take part in conversations with consideration given to his or her needs. The psychosocial context of some situations may require particular attention, for example, support for single mothers, mothers in difficult socioeconomic situations, mothers who are new to Canada or who are refugees, mothers with psychosocial concerns identified during pregnancy, or teen mothers.
Mother’s Adjustment and Emotional Health
Research shows that the mother’s emotional adjustment affects her well-being as well as that of the baby and the family. Footnote 51 Mothers may experience a range of emotions postpartum, including baby blues, depression, anxiety disorders, obsessive–compulsive disorders, trauma and stressor-related disorders, and postpartum psychosis.
Compassion and vigilance are the key approaches to effective support for the new mother and family during this period of transition. HCPs will want to attune themselves to the thoughts and experiences of new mothers and their partners in order to help them explore their feelings and emotional health, rather than rely on tasks or checklists. As always, the goal is to empower the mother in her own capacity to adjust and adapt.
The Canadian Task Force on Preventive Health Care guideline Recommendations on Screening for Depression in Adults does not recommend screening of adults by population subgroup, including perinatal and postpartum women, who may be at increased risk of depression. They recommend that clinicians remain alert to the possibility of depression, especially in individuals with characteristics that may increase the risk for depression, and be attentive when there are clinical clues. The Task Force does not have guidelines on screening for other areas of emotional health and mental illness. Footnote 52
Other organizations, such as the Registered Nurses’ Association of Ontario (RNAO), the Ontario Provincial Council for Maternal and Child Health, Perinatal Services BC, and the US Preventative Task Force, do recommend screening pregnant and postpartum women for depression. Footnote 42 Footnote 53 Footnote 54 Footnote 55
It is important that HCPs develop assessment skills to monitor symptoms for mental disorders and stay alert for signs of concern so they can provide appropriate information and support. need to be aware of the various types of responses and sufficiently knowledgeable about emotional health to identify psychiatric disorders in the immediate postpartum phase and beyond (as these disorders do not always present in early postpartum).
Caesarean Birth
Caesarean births are common—in 2016/17, 28% of all births in Canada were by caesarean births. These rates range from 18.5% to 35.3% across the provinces and territories. Footnote 56 Footnote 57
Mothers and families who have an emergency caesarean birth after a long and difficult labour have special needs. They may be experiencing depression, anxiety, guilt, sense of loss of control, less satisfaction with the birth experience, and loss of self-esteem. Footnote 58 Mothers and families who undergo planned, scheduled caesarean births can use coping mechanisms to prepare for the surgery; women undergoing an unplanned caesarean birth do not have this preparation time. Footnote 32 If a woman has an unplanned caesarean birth but feels respect and compassion and that her caregivers are collaborating with her during her labour, her outcomes will likely be optimized. If a woman has an unanticipated caesarean birth and is not supported, she could develop posttraumatic stress disorder (PTSD). Footnote 51 HCPs are well-positioned to help mothers and their families resolve their feelings about the caesarean birth, and connect families to support and services in the community, if needed.
Women who have a caesarean birth need more care and support in their postpartum recovery and greater support caring for themselves and their babies. They experience higher levels of fatigue, constipation, depression, anemia, headache, difficulty voiding, abnormal bleeding, urinary tract infection, abdominal pain, and vaginal discharge than women who have a spontaneous vaginal birth. Primarily because of pain, mothers may need extra help with breastfeeding, especially during the first few days, and they have increased difficulties caring for their babies due to painful or reduced mobility. Footnote 59 It is vital that women and their partners/families understand what to expect during the recovery period, such as the importance of rest, fluids, support for mobility, and adequate diet for recovery. They also need to plan for support with lifting, driving, and household chores.
The average length of hospital stay is longer for women who have caesarean births than for those who have vaginal births. Family support is imperative after a caesarean birth. Mothers and babies should be cared for as a unit, with her partner, if available, including in the NICU.
During the early postpartum period, care of the newborn usually involves celebrating and rejoicing with the family and respecting and supporting their needs. The care is based on nurturing the developing mother–baby–family relationship and caring for mother and baby as a unit. It includes asking the mother and her partner about their concerns and feelings, observing the baby, and supporting his or her health and well-being.
HCPs will want to ensure that the information and advice they share is clear, consistent and tailored to the mother’s specific needs. By focusing on the expressed concerns of the family, rather than on predetermined teaching lists, HCPs will avoid overwhelming them with information. Opportunities to share information about the health and care of babies, including signs of concern, are maximized by caring for mother, baby, and the family together. The mother or partner should be present any time the newborn is being examined, and then made aware of the findings.
There are no Canadian guidelines on the development of newborn care plans. The National Institute for Health and Care Excellence (NICE) and the American College of Obstetricians and Gynecologists (ACOG) recommend developing a documented, individualized postnatal care plan with the woman, ideally in the antenatal period or as soon as possible after the birth. The plan would list the HCPs involved in her and her baby’s care, including their roles and contact details. NICE and ACOG recommend that parents be offered information and advice to enable them to assess their baby’s general condition, identify signs and symptoms of common health problems in babies, and contact an HCP or emergency service if required. Footnote 24 Footnote 60
For babies born in hospitals or birthing centres, the length of their stay varies from a few hours to about 72 hours. Appropriate postpartum follow-up, including a physical examination by a skilled HCP is essential. This physical examination should include observing feeding. The CPS guideline Facilitating Discharge from Hospital of the Healthy Term Infant provides recommendations for discharge and newborn follow-up. Footnote 45
Midwives carry their own caseload and follow their clients regardless of place of birth. They commonly provide three home visits during the first weeks of life.
Baby-friendly Environment and Exclusive Breastfeeding
Breastfeeding is recognized as the unequalled way to provide optimal nutritional, immunological, and emotional nurturing of infants. Footnote 61 Footnote 62 Footnote 63 Footnote 64 Footnote 65 Consistent with WHO global recommendations, Health Canada recommends exclusive breastfeeding for the first 6 months that is sustained for up to 2 years or longer with appropriate complementary feeding. This is important for the nutrition, immunologic protection, growth, and development of infants and toddlers. Footnote 66
It is also important that hospitals, birthing centres, and community health facilities protect, promote, and support breastfeeding, strive for Baby-Friendly status, and achieve the Ten Steps to Successful Breastfeeding.
Infant Mental Health
Infant and early childhood mental health has been defined as “the infant’s/young child’s capacity to experience, regulate, and express emotions, form close and secure relationships, and explore the environment and learn. Footnote 19 ”
Infants form attachments, learn about social interactions and relationships, take in information from the world around them through their five senses, and as they grow, explore their world. Infant mental health is impacted by a number of factors – biology, genetics, brain development, temperament, the prenatal environment, illness or disability, relationships, attachment, their parents’ mental health, parenting, their environment, the social determinants of health, violence, stress and trauma and resiliency. Footnote 67
The basis for mental health starts early in life. Early experiences, including infants’ relationships with parents and caregivers, affect the architecture of their developing brains. Footnote 68 The infant’s brain is growing very fast – and nurturing and responsive caregiving is the key to supporting healthy brain development. Footnote 67 Disruptions in this process can influence stress regulation, emotional health and immune system development throughout life. Footnote 68 Infants are totally dependent on their parents and other caregivers, and when parents and caregivers are responsive, consistent, and nurturing, and they live in safe and economically secure environments, their infants are more likely to have strong emotional health. Footnote 67 Footnote 68 Footnote 69
Parenting and caregiving affect the infant’s/young child’s brain development and mental health through a number of mechanisms. One is attachment. When infants are nurtured and looked after responsively by their parents and other caregivers, their physical and mental health is affected for life through the formation of strong, positive bonds with adults – or attachment. Babies who are securely attached demonstrate less anxiety and more positive emotion in young childhood and are more capable of forming relationships with peers and adults. Footnote 67 Footnote 69
Consistent, high quality and timely daily routines also shape the baby’s developing regulatory system. The predictability and quality of routines influence the biological rhythms related to waking, eating, eliminating, and sleeping. Footnote 67 Footnote 69
On the other hand, if babies experience persistent, toxic stress, the architecture of their brains is weakened. This can lead to mental health issues and physical, learning and behaviour problems throughout life. While stress is an important part of healthy development, when babies without supportive relationships experience high levels of stress for long periods of time, the result is toxic stress. Footnote 70
If parents (or other caregivers) struggle with depression or problematic substance use, for example, they may have difficulty being responsive to their infants. Footnote 71 Footnote 72 Furthermore, if parents have high levels of stress themselves due to precarious economic, housing, or safety conditions, they may struggle to respond to their infants as needed. Footnote 73 Parents in these situations need particular support.
Optimal growth and development requires a continuum of services for infants, toddlers, and their families, delivered by trained professionals. Early investment can support infant mental health and prevent the need for more expensive interventions down the road. Footnote 67 Developing a strong system of informal and formal services is necessary in order to support parents who are struggling to care for their children. In addition, infants/children who are experiencing abnormal stress need assessment and treatment, along with expert support, before this stress has long-lasting effects. Footnote 73
Breastfeeding supports neurodevelopment. This may be due to the breastmilk nutrients or the mother–baby interaction – or both. Neuroscientific evidence strongly supports that infants be exclusively breastfed for 6 months and that hospitalized preterm infants either be breastfed or receive breast milk. Footnote 74 Footnote 75 Consistent with the WHO global recommendation for public health, Health Canada recommends exclusive breastfeeding for the first 6 months that is sustained for up to 2 years or longer, with appropriate complementary feeding to support nutrition needs, for immunological protection and growth and development of infants and toddlers. Footnote 66 Mothers and their families need breastfeeding information and support to encourage exclusive breastfeeding.
Programs that are offered before, during, and after pregnancy as well as during early childhood, have shown benefits for supporting positive infant and child mental health. Footnote 76 These include home-visiting and other family support strategies.
Nobody’s Perfect is a facilitated, community-based parenting program for parents of children from birth to age 5. The program is designed to meet the needs of parents who are young, single, socially or geographically isolated, or who have low income or limited formal education. Several studies have shown that participants in the Nobody's Perfect parenting program experience increased: Footnote 77
- Confidence in their parenting skills;
- Ability to cope with stress;
- Ability to problem solve;
- Resiliency;
- Self-sufficiency and independence;
- Frequency of positive parent–child interactions;
- Use of positive discipline techniques; and
- Access to peer/social/community support.
While there are no national Canadian guidelines on infant mental health, the CPS position statement Relationships Matter: How Clinicians Can Support Positive Parenting in The Early Years offers advice on how physicians can positively affect family health and well-being, support parents, and connect families with community resources. Footnote 78 The Infant Mental Health Promotion coalition from the Hospital for Sick Children has developed best practice guidelines, Competencies for Practice in the Field of Infant Mental Health . These outline the knowledge and skills needed to provide competent care. Footnote 79 Best Start has ready-to-use workshop resources for service providers, Healthy Baby Healthy Brain , that help parents and expectant parents support their baby’s brain development. Footnote 80
Ophthalmia Neonatorum
Prophylaxis for neonatal gonococcal ophthalmia remains mandatory in some provinces and territories. The CPS states that “erythromycin, the only ophthalmic antibiotic eye ointment currently available for use in newborns, is of questionable efficacy. Footnote 81 ” Furthermore, the Society considers that eye prophylaxis is not effective in preventing chlamydial conjunctivitis, and that applying medication to the eyes of newborns may result in mild eye irritation. Footnote 81 They no longer recommend prophylaxis for ophthalmia neonatorum but recommend screening all pregnant women for gonorrhea and chlamydia infection, with treatment and follow-up of those found to be infected. The CPS suggests that mothers who were not screened should be tested at birth, and babies of mothers with untreated gonococcal infection should receive ceftriaxone. Footnote 81
The Public Health Agency of Canada (PHAC) states that “all pregnant women at risk should be screened at the first prenatal visit or at the time of delivery if not previously screened,” and provides guidance for the management of ophthalmia neonatorum. Footnote 82
Mothers look at their baby’s skin regularly, and HCPs can help them understand transient benign skin conditions such as acrocyanosis, baby acne, cutis marmorata (mottling), milia, erythema toxicum neonatorum, and dermal melanocytosis (Mongolian spots). Footnote 83 Footnote 84
For detailed information on valid and reliable skin assessment tools for babies at risk of impaired skin integrity, refer to the Association of Women’s Health, Obstetric and Neonatal Nurses (AWHONN) guideline Neonatal Skin Care . Footnote 83
It is important to share information about skin creams or barriers with parents. While routine application of skin creams or lotions is not necessary for newborns, petroleum emollients have been demonstrated to prevent dermatitis and skin breakdown without increasing the risk of infection. Footnote 24 Footnote 83 Barrier creams or ointments can be applied to the diaper area if reddening is noted.
Parents of both newborn boys and girls need to be made aware of how to properly clean and care for their child’s genitals. For example, in the case of uncircumcised newborn boys, normal foreskin can remain nonretractile until puberty. Footnote 84
Newborn babies are often bathed for aesthetic and hygiene reasons, as opposed to medical indications (i.e., to prevent transmitting certain infectious diseases). Footnote 83 Footnote 85 Vernix caseosa, the waxy white substance found coating the skin of newborn babies, moisturizes the baby’s skin and prevents bacterial cutaneous infections. It should not be washed off, but should be allowed to dry naturally.
The priorities at birth and in the early postpartum period are skin-to-skin contact, breastfeeding, and promoting attachment; the first bath can be postponed. Some families bathe their baby for the first time at home, when the baby is a few days old. Ultimately, “decisions about the frequency of bathing and time of day should be based on the individual baby’s need and consideration of family values and beliefs of the local culture. Footnote 83 ”
Newborns do not require daily bathing. Encourage parents to wash their baby with a warm wet cloth between baths, and to wipe the baby’s face and hands frequently. Footnote 83 Footnote 84
Umbilical Cord Care
Parents need to be informed about care of the umbilical cord. Natural drying is recommended, that is, putting nothing on the cord. Topical drying agents (including isopropyl alcohol) and antibiotics do not reduce cord separation time or frequency of cord infections, and in some cases, they can harm the newborn. Footnote 24 Footnote 83 Footnote 85 Newborns can be bathed with the umbilical cord intact so long as the cord is dried thoroughly afterwards.
Fold down diapers to provide maximum exposure to air and prevent contamination with stool or urine. If the umbilical cord or stump is soiled with urine or stool, the area should be washed with water and dried. Parents need to recognize that fever (38 °C or higher), redness, swelling, drainage (yellow pus), foul-smelling discharge, and bleeding (more than a few spots on the diaper shirt or sleeper) are abnormal findings that they should report to their HCP. Footnote 83 Footnote 84
Circumcision
Parents require accurate, up-to-date, evidence-based information about circumcision so they can make an informed choice for their baby. There is considerable controversy in medical communities regarding circumcision. In their position paper, the CPS outlines the benefits and risks, and does not recommend routine circumcision. Footnote 86 According to the American Academy of Pediatrics, the health benefits of newborn male circumcision outweigh the risks. However, the health benefits are not great enough to recommend universal newborn circumcision. Footnote 87 The Journal of Medical Ethics has an exclusive edition exploring the medical, religious, and social reasons for and against circumcision. Footnote 88 Religious, cultural, and social factors play an important part in the decision to circumcise male babies – these should be considered and respected.
Early Immunization
In most parts of Canada, routine immunizations are not given to newborns. As of 2014, only New Brunswick, the Northwest Territories, and Nunavut include hepatitis B vaccine as part of the immunization schedule at birth. Footnote 89 PHAC recommends that hepatitis B vaccine be given at months 0, 1, and 6 with at least 4 weeks between the first and second dose, at least 2 months between the second and third dose, and at least 4 months between the first and third dose. Alternatively, it can be given as DTaP-HB-IPV-Hib vaccine, which protects against diphtheria, tetanus, pertussis (whooping cough), hepatitis B, polio, and Haemophilus influenzae type b, with the first dose at 2 months of age. Footnote 89
It is recommended that a baby whose mother has tested positive for the hepatitis B surface antigen (HBsAg) receive hepatitis B immunoglobulin and a vaccine within 12 hours of birth. If the mother’s hepatitis B status is not known, and will not be known within 12 hours of birth, HCPs might consider administering the vaccine and the immunoglobulin based on risk factors, erring on the side of caution and administering both when uncertain. If the mother is HBsAg negative, it is reasonable to administer the vaccine to babies who may be at increased risk of exposure to HbsAg-positive household members or those at high risk of being positive. Footnote 89
Parents, grandparents, family, and friends who are in regular contact with a baby should have all their recommended immunizations and these should be up-to-date. Anyone requiring a booster vaccine should get it at least 2 weeks before contact with the baby. Footnote 89 This is particularly important for diphtheria, tetanus, and acellular pertussis adult vaccine, as well as for influenza vaccine.
Cases of vitamin D deficiency still occur in babies in Canada who do not receive vitamin D as a supplement. Footnote 90 Without supplementation, a baby's vitamin D stores will be depleted, particularly if the mother's vitamin D stores are low. Footnote 91 Footnote 92
Nutrition for Healthy Term Infants , a joint statement by Health Canada, CPS, Dietitians of Canada, and the Breastfeeding Committee for Canada, recommends a daily vitamin D supplement of 10 µg (400 IU) for exclusively and partially breastfed babies, from birth to 1 year of age. Children aged 12 to 24 months of age who are breastfed or receive breastmilk should continue to receive this daily vitamin D supplement of 10 µg (400 IU). Footnote 66 Footnote 93 Breastfed babies living in northern latitudes require special attention. In this situation, the CPS suggests that vitamin D supplementation within a range of 400 IU/day to 800 IU/day appears to be safe. Footnote 94
Continuing this supplement is a conservative approach to achieving adequate vitamin D intakes. It also provides a consistent and straightforward public health message. In individual practice, the decision to discontinue the supplement beyond 12 months of age can be informed by a dietary assessment of other contributors of vitamin D, such as cow milk. Footnote 93
Newborn Screening
Newborn screening has been one of the most successful public health programs of this century. It has achieved the goal of detecting hereditary disorders that can result in death or severe long-term disability if not identified prior to the onset of signs. Footnote 95
Current Canadian standards are set at the provincial and territorial level, resulting in variations in the number of screening tests performed in the general categories of endocrine disorders, hemoglobinopathies, fatty acid, amino acid and organic acid disorders, cystic fibrosis, galactosemia, and other disorders. Footnote 96 HCPs would be expected to discuss screening the newborn with parents before and soon after the birth, emphasizing that this is a routine part of their baby’s care that can prevent serious health problems. The newborn screening blood specimen card is completed between 1 and 7 days of age — and ideally between 2 and 3 days of age. If testing is conducted earlier, before 24 hours, repeat the test within 5 days. In Quebec, in addition to blood sampling, a urine sample is obtained at 3 weeks for screening of a number of hereditary conditions.
According to the CPS, all newborns should be screened for hyperbilirubinemia, using a predictive nomogram. The Society recommends measuring bilirubin at the same time as having the metabolic screening test, unless it is required earlier, or at discharge or within 72 hours of birth, whichever comes earlier. This is particularly important if babies go home early, since bilirubin levels will peak at home. Footnote 97
The incidence of critical congenital heart disease (CCHD) in Canada is 3/1000 live births. CCHD accounts for more deaths than any other congenital malformation. Between 10% and 30% of CCHD diagnoses are not made prior to discharge from hospital although early diagnosis and follow-up are essential first steps in preventing infant mortality and morbidity. Footnote 98 Some centres now perform routine pulse oximetry screening to identify babies with CCHD. Used in conjunction with prenatal ultrasound and a physical examination, pulse oximetry screening is the best approach to detecting CCHD in newborns. Footnote 99 The CPS recommends that pulse oximetry screening be performed between 24 and 36 hours after the birth, using the baby’s right hand and either foot to minimize false-positive results. The Society recommends that newborns with abnormal results undergo a thorough evaluation by the most responsible HCP. If a cardiac diagnosis cannot be excluded, newborns with abnormal results would be referred to a pediatric cardiologist. Footnote 100
Hearing Screening
Hearing loss is not a common disorder in the newborn. Profound hearing loss (>70 dB) occurs in approximately 1 to 3 infants per 1000 live births. Together with moderate loss (>40 dB), the prevalence increases to 6 per 1000. Footnote 101 Universal screening for hearing results in earlier diagnosis and intervention and improved language outcomes for children. Footnote 102 The CPS and Speech-Language and Audiology Canada recommend universal screening for all newborns. Footnote 102 Footnote 103
Speech-Language and Audiology Canada recommends that screening be conducted by 1 month of age, in either a hospital or community-based setting. Any suspected hearing loss should be confirmed by 3 months of age, and an intervention implemented by 6 months of age. Footnote 104 Screening policies, however, vary between provinces, with some offering universal screening and others screening only high-risk populations. Footnote 96
HCPs will want to discuss the hearing tests with parents and explain the rationale, how they are performed, and the implications of test results that show possible hearing loss. It is also important to explain the efficacy of the test and the occurrence and meaning of false positives.
Newborns, both preterm and term, have a hypersensitivity to stimuli and are more prone to pain and the consequences of pain. It is critical that they receive effective pain relief. As newborns cannot verbalize, it is up to their caregivers to assess and alleviate their pain. Always keep the number of painful procedures to a minimum; those that are conducted should be evidence-based.
Some effective pain management strategies have been identified for newborns during bedside procedures. Footnote 105 Breastfeeding and skin-to-skin contact together are effective at reducing pain, and this is the first line of pain reduction for procedures such as injections, heel lancing, or venipuncture. Footnote 106
- Skin-to-skin contact reduces pain responses in preterm and term babies. Footnote 107 Skin-to-skin contact should be started approximately 10 to 15 minutes prior to the procedure. Footnote 105
- Breastfeeding should be started approximately 5 minutes before the procedure. Ensure that the baby achieves an effective latch with sustained sucking and swallowing. Footnote 105 Sweet solutions, including breast milk, have analgesic effects on babies. Footnote 108
Refer to the CPS guideline Prevention and Management of Pain in the Neonate on bedside procedure pain management as well as surgery and major procedures. Footnote 109
An optimal amount of sleep for both babies and parents is a priority for parents. Deciding where a baby sleeps is personal and highly variable. The decision may be based on cultural or personal values or the desire to facilitate breastfeeding. Alternatively, it may reflect socioeconomic realities such as unstable housing or poverty resulting in a lack of resources such as a crib. Footnote 110
It is incumbent on all HCPs to work closely with the families to promote safe sleep for their babies. HCPs and parents should discuss the following modifiable risk factors, which reduce the risk of Sudden Infant Death Syndrome (SIDS): Footnote 111
- Breastfeeding of any duration, which provides a protective effect, with exclusive breastfeeding offering greater protection;
- Placing infants to sleep in a crib, cradle, or bassinet—one that meets current Canadian regulations—in the same room and near the parent or caregiver's bed;
- Providing a smoke-free environment—both before and after the birth; and
- Placing infants on their backs to sleep, for every sleep.
PHAC recognizes SIDS and other infant deaths that occur during sleep as major public health concerns. Footnote 111 According to Statistics Canada, 10 babies aged less than 1 year died from SIDS in 2018. Footnote 112 While it is important to differentiate between SIDS and accidental suffocation and strangulation in bed, the American Academy of Pediatrics notes that many of the modifiable and non-modifiable risk factors for SIDS and other sleep-related infant deaths are similar. Footnote 113
There is some confusion around the meaning of the term “co-sleeping.” Sometimes it refers to sleeping in the same bed and sometimes to sleeping in the same room. Room sharing occurs when the baby and adult caregiver sleep on separate surfaces in the same room—a practice that is recommended. Footnote 111 Footnote 113 Bed sharing, when the baby and caregiver share the same sleep surface, is not recommended by either CPS or PHAC.
Parental fatigue can play a significant role in creating unsafe sleep environments for babies and, infrequently, extreme parental fatigue can contribute to accidental suffocation. Footnote 110 A more likely scenario is that parents become so tired that they are less capable of making evidence-based decisions about sleep for either themselves or their babies. HCPs should take a proactive approach when it comes to discussing sleep strategies with parents.
Some parents may be hesitant to reveal their actual sleeping environments to HCPs for fear of reprimand. However, they should be able to make informed decisions about where they intend to place their baby to sleep. The prenatal period is an opportune time for HCPs to bring up safe sleep practices, to inquire about where the parents plan to place their baby to sleep, and to explore factors such as socioeconomic circumstances, cultural practices, and beliefs that may influence safe sleep decisions. Footnote 114 However, this should not be a one-time event – plan on having multiple discussions with parents on the topic of safe sleep.
Effective care requires a coordinated approach that involves ongoing communication between HCPs, parents, families, and other caregivers. The unique beliefs and needs of each family, and their personal and environmental resources, influence their decisions. Footnote 115
Refer to the CPS, Canadian Foundation for the Study of Infant Deaths, Canadian Institute of Child Health, Health Canada, and PHAC Joint Statement on Safe Sleep for more information. Footnote 111
Growth Monitoring
Monitoring a baby’s growth helps identify health or nutrition problems early enough for corrective action to be effective. Footnote 66 Footnote 93 Measurement of growth over time should be combined with clinical, developmental, and behavioural assessments. The WHO Child Growth Standards are based on the growth of breastfed babies. Footnote 116 Standard growth charts show the gradual change in growth velocity.
Babies who are feeding well typically regain their birth weight by 10 to 14 days, double their weight by about 5 months, triple it by 12 months and quadruple it by 2 years of age. Footnote 117 Babies grow quickly during the first 3 months, gaining 20 to 30 g per day in the first 4 weeks, or an average of 0.6 to 1.4 kg per month. Footnote 118
At-risk or Unwell Babies
Routine monitoring of newborns should include evaluation and documentation of vital signs, weight, and feeding in addition to routine screening practices. HCPs responsible for newborn babies should be trained to identify abnormal findings and initiate interventions such as glucose monitoring, saturation monitoring, and positive pressure ventilation. The ACoRN program trains HCPs in a primary survey of at-risk or unwell babies to identify areas of concern that require attention. Footnote 119
4. Complications Related to the Mother
Transition to parenthood is normally a time of intense emotional adjustment that is compounded by sleep disruptions, fatigue, and anxiety about caring for and parenting a baby. It can also be a period of high risk for the development or recurrence of mental illness in new mothers. During this time, any from the entire spectrum of psychiatric disorders may occur. Concerns about women’s mental health are some of the most prevalent problems of the perinatal period. Psychiatric disorders often begin in pregnancy, but onset may also be late into the first postpartum year.
Women with a history of psychiatric disorders are particularly vulnerable, although new onset disorders can occur in any postpartum woman due to the complex interplay of biological, psychological, and social determinants of mental health. Women who have a traumatic birth experience, or women who have ill and/or hospitalized newborns, may be at increased risk of mental health problems. Footnote 51 Inadequate support during the postpartum period can also contribute to or exacerbate mental health problems.
The onset or worsening of depression, anxiety, or other mental illnesses can have serious, long-lasting effects on the mother’s developing relationship with her baby. Postpartum depression—especially when left untreated, resulting in chronic maternal depression—can lead to social, emotional, and behavioural development problems in children, including issues with conduct, emotion regulation, insecure attachment, and poor cognitive outcomes. The effects also depend on factors such as social and material support. Footnote 120 Identifying postpartum mental illnesses and providing appropriate psychological support and possible psychiatric care is important. At the same time, ensure that other medical conditions, such as anemia or thyroid abnormalities or substance use, are not causing or contributing to the symptoms.
Ideally, an interprofessional team cares for a new mother with postpartum mental illness. This requires integrating and, especially, coordinating care and services where interventions and objectives are chosen with and accepted by the mother. Footnote 121 Since postpartum women can experience mental health problems for a long time (more than a year in some cases), having one person coordinate integrated care can help ensure that the care is consistent and ongoing. If the mother agrees, her partner and family may also be involved in decisions regarding her care.
Supporting Women with Postpartum Mental Illness Footnote 51
Supporting women with postpartum mental illness requires a multifaceted, family-centred approach based on the individual needs and experiences of the woman and her family. Effective treatments for postpartum mental health disorders may require referral to a mental health professional. HCPs can support new mothers and families by:
- Knowing how to differentiate between postpartum depression and other anxiety disorders or mental illnesses, including post-traumatic stress disorder (PTSD);
- Being familiar with risk factors associated with postpartum depression and mental illnesses;
- Being able to identify women at risk of developing postpartum emotional disorders and those in difficulty;
- Recognizing the symptoms of mental disorders, from baby blues to postpartum psychosis;
- Knowing about the range of treatment options available for the various postpartum mood disorders, and providing women and their families ways to access the appropriate resources;
- Helping to debunk the “motherhood equals joy and complete fulfillment” myth; and
- Encouraging women to talk about their negative emotions to do with motherhood.
Postpartum Blues
The most common type of postpartum mood change is the postpartum blues, or baby blues . Estimates of prevalence range dramatically, from 15% to 84%. Footnote 122 The postpartum blues are thought to be an effect of the rapid post-childbirth hormonal drop on the neurotransmitter systems involved in mood disorders. Footnote 123 Footnote 124 Footnote 125 Footnote 126 Footnote 127 The challenges of caring for the baby and interrupted sleep are also likely to contribute to the blues. Footnote 128 Footnote 129
Common symptoms of postpartum blues are low mood, emotional lability, tearfulness, fatigue, and irritability. These symptoms are usually transient, beginning shortly after childbirth and resolving on their own within the first few weeks postpartum. Footnote 123 The transient nature of the symptoms helps distinguish postpartum blues from a major depressive episode. Other features that distinguish postpartum blues from a major depressive episode are the lack of severe symptoms, such as persistent insomnia, thoughts of guilt or worthlessness, or suicidal ideation. The reason some women have postpartum blues, while others develop major depression is unknown, but research suggests that genetic predisposition is a factor. Footnote 130 Footnote 131 Postpartum blues are self-limiting and require no treatment other than reassurance and support. Footnote 132 However, early onset, severe, or prolonged blues is associated with postpartum depression, and requires medical attention. Footnote 133
Postpartum Depression
Postpartum depression can affect a woman at any age or socioeconomic status and from any culture. Biological risk factors may include history of depression or untreated depression in pregnancy, while psychosocial risk factors may include poor social support and stressful life events, including issues related to the health of the baby. Footnote 134 Some women are at a higher risk of postpartum depression such as Indigenous women, younger mothers, sexual minority women, and women who are recent immigrants to Canada.
The Diagnostic and Statistical Manual of Mental Disorders, version 5 (DSM-5) qualifies a major depressive episode with peripartum onset when symptoms start in late pregnancy or within the first 4 weeks postpartum. Footnote 135 However, most clinicians define postpartum depression as depression during the first year postpartum. Footnote 136 Footnote 137 Footnote 138
According to 2019 Canadian data, almost one-quarter (23%) of mothers who recently gave birth reported depressive and anxiety symptoms that might or might not be postpartum depression or anxiety because these were just very general screening scales. Prevalence of such feelings was higher among mothers aged under 25 years (30%) than all other age groups. Of the mothers who had these feelings, 31% had been told by an HCP that they had depression or a mood disorder before pregnancy. Almost one-third (32%) of mothers who had these feelings reported that they received mental health treatment since the birth of their baby—39% had counselling, 38% medication (such as anti-depressants), and 23% counselling plus medication. Footnote 139 Women with bipolar disorder are at particularly high risk of developing a depressive episode postpartum. Footnote 140
Recent Canadian research indicates that First Nations mothers had a 20% increase in the mean scores of depressive symptoms compared to White Caucasian mothers in Canada. Footnote 141 A systematic review of the evidence on the prevalence of postpartum mental health disorders in Indigenous women confirmed this finding. Footnote 142 Chronic life stress and trauma are considered key causes of prenatal and postpartum depression among Indigenous women. This life stress is influenced by racism, sexism, domestic and sexual violence, and intergenerational trauma from residential schools and other legacies of colonization. Footnote 9
Symptoms of a Major Depressive Episode Footnote 135
- Persistently low mood and/or loss of interest
- Accompanying low energy
- Sleep and appetite disturbances
- Negative thinking patterns
- In more severe cases, thoughts of self-harm and suicide.
While the symptoms of postpartum depression are similar to those of a major depressive episode outside of the postpartum year, the negative thoughts and images associated with postpartum depression can focus on feelings of failure as a mother, anxiety about the baby’s health and well-being, and guilt about having difficulty with the transition to parenthood. While perinatal suicide is extremely rare, as many as 20% of women report thoughts of self-harm or suicide. Footnote 143
The Canadian Task Force on Preventive Health Care guideline Recommendations on Screening for Depression in Adults does not recommend screening for depression in perinatal and postpartum women. Footnote 52 However, there are tools that can be used to help detect anxiety and depression in the postpartum period.
Tools to Detect Anxiety and Depression Postpartum
The Edinburgh Postnatal Depression Scale (EPDS) Footnote 144 Footnote 145 Footnote 146
This 10-item depression scale:
- Can be used in clinical care or for women at risk of, or showing, symptoms of postpartum depression;
- Can be used any time postpartum, including at regular maternal or baby checks;
- Has an anxiety subscale (items 3, 4, and 5);
- Asks about self-harm thoughts (item 10).
Women with a score higher than 12 (out of 30) have 10 times the likelihood of being diagnosed with postpartum depression than women with a lower score.
Whooley Questions for Depression Screening Footnote 121
There are two Whooley questions for depression:
- During the past month, have you often been bothered by feeling down, depressed, or hopeless?
- During the past month, have you often been bothered by little interest or pleasure in doing things?
If a woman answers yes to either of these questions, it signifies need for further follow-up to determine whether she has depression.
Refer to the Registered Nurses’ Association of Ontario best practice guidelines for effective interventions when caring for mothers with postpartum depression. Footnote 53
Anxiety and Related Disorders
Anxiety is a primary feature of perinatal depression, with the prevalence of anxiety symptoms ranging from 14% to 20% in the postpartum period. Footnote 147 Footnote 148 Footnote 149 Parents often feel anxious about the welfare of the baby, insecure about their parenting abilities, or worry about being alone. However, women can also have anxiety and related disorders, including generalized anxiety disorder, panic disorder, obsessive–compulsive disorder and PTSD. Footnote 134
The Generalized Anxiety Disorder 2-item (GAD-2) questionnaire is a useful tool for identifying generalized anxiety disorder. Footnote 150 The tool has just 2 questions with four possible answers per question: Footnote 151
Over the last 2 weeks, how often have you been bothered by the following problems? Feeling nervous, anxious or on edge? Not at all/Several days/More than half the days/Nearly every day Not being able to stop or control worrying Not at all/Several days/More than half the days/Nearly every day
New parents are naturally nervous when they are beginning to care for their newborn baby. Generalized anxiety disorder, however, is characterized by excessive worry about anticipated events or activities in a way that is difficult to control or interferes with daily functioning. The anxiety can be clustered worries about finances, appearances, maintenance of household duties, and the well-being of the baby, for example. Footnote 152
Panic disorder, affecting about 1% to 3% of new mothers, may cause significant impairment. It can result in the mother experiencing isolation due to her difficulty in leaving the home or being in groups of people. Footnote 152 Footnote 153
Obsessive–compulsive symptoms occur in 4% to 9% of new mothers. These most often include obsessions about contamination, compulsions about checking and ordering, and in some cases, thoughts about the baby being harmed. Footnote 154 Footnote 155 Footnote 156 Footnote 157 The latter can be distinguished from psychosis because women with obsessive–compulsive symptoms have no intention of harming their child and are significantly distressed by these types of thoughts. Obsessive–compulsive symptoms commonly co-exist with a depressive episode. Footnote 155
Trauma- and stressor-related disorders, including PTSD, affect about 3% of postpartum women and up to 15% of high-risk women. Footnote 158 Important risk factors included a history of psychopathology, current depression, and complications during pregnancy, labor and delivery. While it is rare that a stressful birth experience leads to PTSD, risk factors do include having a birth experience different from what was expected and ineffective communication where HCPs do not listen to the woman. Footnote 158
Severe Postpartum Mental Disorders
Bipolar disorder and schizophrenia.
About 2% of pregnant women have a pre-existing bipolar disorder, and less than 1% have a pre-existing psychotic disorder such as schizophrenia. Footnote 159 Women with severe mental disorders are at particularly high risk of relapse in the postpartum period and usually require special mental health care. They are also at high risk of developing postpartum depression. Footnote 140
Evidence suggests that there is a relationship between bipolar disorder and postpartum psychosis, with the majority of cases thought to be variants of bipolar disorder. The risk of relapse in women with primary psychotic disorders increases during the postpartum period. Footnote 160 Footnote 161 Sometimes postpartum psychosis is preceded by hypomanic or manic symptoms. Footnote 162
Women with severe mental disorders and their families require support from professionals and family/friends as well as appropriate treatment to promote optimal health and parenting.
Postpartum Psychosis
Postpartum psychosis, the most severe postpartum psychiatric disorder, is a medical emergency. Postpartum psychosis occurs in approximately 1 in every 600 postpartum women. Footnote 161 It most often occurs during the first week or the first month postpartum, but it can occur later in the postpartum period or at weaning, although the latter is rare.
The primary symptoms of postpartum psychosis reflect a significant change from the woman’s usual personality, with confusion and clouding of consciousness considered classic symptoms. These symptoms may be accompanied by an inability to distinguish thoughts from reality and delusions about herself, her baby, or others. Footnote 163 Footnote 164
Women with a history of bipolar and psychotic illnesses are at increased risk for postpartum psychosis, particularly if they stopped taking medication during pregnancy or in the early postpartum period. Other risk factors include a family history of psychiatric illness (particularly bipolar affective disorder) and sleep deprivation among women with a previous bipolar mood disorder diagnosis. Footnote 140
Women with postpartum psychosis require urgent psychiatric consultation, pharmacological treatment, ongoing support to facilitate the recovery process, and usually hospitalization. Footnote 165 They should not be left to care for their babies alone until the psychosis has resolved. Assess and support safety of the mother and her baby on an individual basis, as delusions may increase the risk of harm to either or both. Family members should be educated and engaged, and ongoing support provided by professionals, community organizations, and family/friends. Footnote 166 Footnote 167
Women who develop postpartum psychosis are at increased risk for reoccurrence during subsequent pregnancies. Footnote 168 Footnote 169
Late postpartum hemorrhage, also called secondary postpartum hemorrhage, can occur 24 hours to 12 weeks after childbirth. The potential causes of late postpartum hemorrhage include retained fragments of the placenta or membranes, sub-involution of the placental site, uterine infection, and coagulation defects. Treatment involves controlling bleeding with medications such as oxytocin, as well as possible blood replacement or surgical intervention.
As most cases of late postpartum hemorrhage occur after women leave birthing facilities, focus the discharge information on expected changes, what amount of bleeding is normal and what amount of bleeding is not normal, causes for concern, and when to contact an HCP or emergency department. If a mother needs to be re-admitted to hospital for late postpartum hemorrhage, it is very important not to separate the mother and baby and to provide support for breastfeeding.
Endometritis
Endometritis is an infection of the reproductive tract. It can occur at any time from birth to 6 weeks postpartum. Endometritis occurs after 1% to 3% of vaginal births and up to 27% of caesarean births. Footnote 170 Endometritis is limited to the uterine cavity but can spread.
A woman with mild endometritis has discharge that is scant or profuse, bloody, and foul smelling. In more severe situations, she has fever, chills, lower abdominal pain or uterine tenderness, anorexia, lethargy, and rapid pulse. Treatment includes administration of antibiotics and can also include rest, a high fluid intake, analgesia as needed, and administration of oxytocics to keep the uterus contracted. Comfort measures are important to relieve the symptoms. Footnote 170 Footnote 171
Women need to be informed about what to expect with regard to normal lochia and vaginal discharge, and should call their HCP if they develop symptoms of endometritis.
Mastitis is an inflammation of the breast that may involve an infection. It is characterized by localized tenderness, redness, and heat, and systemic symptoms of fever, malaise, and occasionally nausea and vomiting. Footnote 172 Mastitis commonly occurs within the first 6 weeks postpartum, but can occur at any point during lactation. It can start as engorgement, develop into non-infective mastitis, and then become infective mastitis. Footnote 172 While the breast is congested/engorged, the most effective treatment is breast emptying—by an electric pump if necessary—and increased water intake.
Mastitis occurs in 10% of breastfeeding women, but some studies have reported the incidence to be as high as 33%. Footnote 173
Encourage mothers to continue breastfeeding. It is important that mothers know their milk is safe for their baby even if they require antibiotics. Frequent feeding and good positioning and latching, with effective milk flow from breast to baby, are preventive factors for mastitis.
Hypertension affects 6% to 10% of pregnant women, but few studies have reported the incidence of postpartum hypertension. Women who have had chronic hypertension, gestational hypertension, preeclampsia, and eclampsia may have preeclampsia postpartum—and may develop preeclampsia for the first time postpartum. Footnote 174 As such, if a mother has hypertensive disorder of pregnancy (HPD), postpartum monitoring is important.
Refer to the SOGC guideline Diagnosis, Evaluation, and Management of the Hypertensive Disorders of Pregnancy for information on care in the first 6 weeks postpartum and beyond. The Working Group recommends checking blood pressure 3 to 6 days following birth, especially if the woman has had a pregnancy complicated by high blood pressure. Footnote 175
During pregnancy, women may develop conditions such as preeclampsia and gestational diabetes mellitus (GDM) that put them at higher risk of heart disease and stroke. Pregnancy-related stroke can happen at any stage of pregnancy, but the greatest risk is during birth and the first few months postpartum. It is usually the result of a pre-existing blood vessel malformation or eclampsia. Peripartum cardiomyopathy (PPCM) is a rare—and often misdiagnosed—form of cardiomyopathy that occurs in the last month of pregnancy and up to 5 months postpartum.
There are a number of risk factors for peripartum cardiomyopathy: multiple pregnancies, twins, preeclampsia and eclampsia, a history of heart problems, excessive alcohol consumption, smoking, diabetes, obesity, unhealthy diet, and African heritage. Footnote 176
It is important to describe the signs and symptoms of heart disease and stroke to women and their families and explain when to talk to an HCP or seek emergency care.
Approximately 53% to 79% of women experience some form of laceration during vaginal birth—most often in the perineal body and commonly first- and second-degree lacerations. The more severe third- and fourth-degree lacerations that result in obstetrical anal sphincter injuries (OASIS) may occur in up to 11% of women who have vaginal births. Footnote 177 OASIS may result in significant problems, including anal incontinence, rectovaginal fistula, and pain, along with increased risk of postpartum urinary retention.
Women who have lacerations during birth need to be made comfortable and helped to recover—and be supported in their confidence in caring for their baby. Provide information so that the woman understands what happened during the birth and the extent of the laceration/injury. Focus on what can help recuperation and healing; that is, rest, hygiene, prevention of constipation, and pain management, as needed, so that they can be actively involved in caring for their babies. Helpful measures include sitz baths, using the side-lying breastfeeding position, avoiding sitting or standing for long periods of time, and seeking and accepting support from family and friends.
The SOGC recommends that HCPs carefully examine all women for perineal or vaginal tears and that anyone with a tear that is more than superficial has a systematic rectal exam for OASIS. Footnote 178 The SOGC guidelines provide recommendations on prophylactic antibiotic administration, the use of laxatives, as well as analgesics for pain, in the case of OASIS. Footnote 178
Refer women who have OASIS to a physiotherapist skilled in helping with this condition. Footnote 178 Footnote 179 The benefits relate to wound healing as well as rehabilitation to restore local and integrated muscle function following the muscle trauma. Scar management may be required to help the woman have intercourse without fear and pain. These considerations may also be relevant for first- and second-degree tears, although in this case referral to physiotherapy is not always necessary.
Women who have experienced female genital mutilation/cutting (FGM/C), also known as circumcision, need particularly sensitive postpartum care. Learning about the cultural, social, psychological, and physical implications of this centuries-old traditional practice will help HCPs talk to mothers appropriately and provide care that is culturally aware and respectful. The perineal area may be extremely painful due to repeated cutting and laceration throughout life compounded by a recent vaginal birth, making even walking difficult. This all makes caring for their baby more problematic. Footnote 180
Following birth, women need additional advice on perineal hygiene. Perineal infections may occur if culturally acceptable methods of cleanliness are not understood by HCPs. For example, using water may be considered impure on religious grounds. Instead, a diluted antiseptic wash may be used for cleaning after voiding.
HCPs will want to address birth control methods, as choice may be limited for women with FGM/C. They may have been taught that touching their genitals is forbidden, and because the vaginal area is sensitive, the use of diaphragms, cervical caps, and sponges is usually not suitable. The most acceptable and reliable method of birth control for women with FGM/C may be intrauterine contraception (IUC, also known as an intrauterine device or IUD). Hormonal contraceptives, either oral or implanted, are also possible. As for all women, the different contraceptive options should be explained carefully and clearly.
HCPs also need to discuss FGM/C with parents and inform them that performing FGM/C is illegal in Canada.
Diastasis recti abdominis (DRA) is defined as a separation of the two sides of the rectus abdominis muscles. Footnote 181 The onset of DRA occurs during pregnancy and the first weeks following birth. Footnote 182 The literature on the prevalence and risk factors for development of this condition is limited. Footnote 181 Footnote 182
A prospective cohort study of 300 first-time pregnant women found the prevalence of mild DRA to be high both during pregnancy and after childbirth: 33% at 21 weeks gestation; 60% at 6 weeks postpartum; 45% at 6 months postpartum; and 33% at 12 months postpartum. There was no difference in reported lumbopelvic pain in women with and without DRA. Footnote 181 In another prospective study of 84 first-time pregnant women, the prevalence of DRA decreased from 100% at gestational week 35 to 39% at 6 months postpartum. Women with DRA at 6 months postpartum were equally likely to report lumbopelvic pain as women without DRA. Footnote 182
A widening of greater than 2.7 cm at the level of the umbilicus is considered to be pathological diastasis of the rectus abdominis muscle. Footnote 183 It can have negative health consequences for women during pregnancy and the postpartum period and beyond, including altered body mechanics and posture, injury of the lumbar spine and pelvis, and impaired pelvic stability. Footnote 184 Footnote 185
Exercise is a protective factor in the development of DRA. Footnote 186 Exercise may reduce the risk of developing DRA as it helps to maintain tone, strength, and control of the abdominal muscle. In addition, women who exercise during and after pregnancy most likely exercised before pregnancy and have better-conditioned abdominal muscles than women who do not exercise. The type of exercise also affects DRA width and recovery time. Footnote 186
It is important to refer women with DRA to pelvic floor physiotherapy. Footnote 187 Physiotherapy or exercises for diastasis recti should not only address the separation but retrain the pelvic floor muscles. More than 70% of women with rectus diastasis cannot do a pelvic floor contraction and therefore are more likely to experience incontinence, prolapse, and pelvic pain. Footnote 188 Consider as well physiotherapy or exercises that address posture, body mechanics, and restricted tissues that may be causing poor movement. A corset or binder is often recommended for separations of 4 finger widths or more. Neuromuscular electrical stimulation also helps to reduce DRA, and if combined with abdominal exercises, can augment the effects. Footnote 189 Some women may meet the criteria for surgery (abdominoplasty) if they have unresolved symptoms that have not responded to exercise. Footnote 187
It is important to encourage women who have had gestational diabetes mellitus (GDM) to breastfeed immediately after childbirth. Breastfeeding helps to lower the risk of neonatal hypoglycemia. Footnote 190
Women with GDM require information about the associated health risks:
- Between 16% and 30% of women with GDM develop type 2 diabetes by 5 to 10 years postpartum, and some women develop type 1 diabetes. Footnote 191
- Metabolic syndrome is more common in women with GDM. Women should be counselled about lifestyle modifications to prevent diabetes and cardiovascular disease. Lifestyle changes can prevent the onset of type 2 diabetes. Footnote 191
- The recurrence rate of GDM in subsequent pregnancies is about 30% to 84%. Footnote 192
For most women with GDM, diabetes goes away soon after childbirth. However, only 50% of women return for postpartum testing due to time pressures, lack of childcare, lack of awareness of the importance of postpartum screening, the unpleasantness of the test, and other factors. Footnote 191 Footnote 192 Footnote 193 The SOGC guideline Diabetes in Pregnancy recommends that women with GDM be screened with a 75 g oral glucose tolerance test (OGTT) between 6 weeks and 6 months postpartum to detect prediabetes and diabetes. Footnote 194 Women with GDM may benefit from the support of a lactation consultant or specialist in case of delayed onset of breastmilk secretion. Footnote 195 Footnote 196
The Canadian Diabetes Association Clinical Practice Guideline Expert Committee recommends that after childbirth women with pregestational diabetes: Footnote 197
- Breastfeed for the many benefits it offers;
- Be carefully monitored as they have a high risk of hypoglycemia postpartum;
- Use metformin and glyburide, if needed, as they can be used during breastfeeding; and
- Have their triglycerides assessed late postpartum.
In addition, women with type 1 diabetes in pregnancy should be screened for postpartum thyroiditis with a thyroid-stimulating hormone (TSH) test at 6 to 8 weeks postpartum.
Postpartum thyroid dysfunction is common and includes hypothyroidism, hyperthyroidism, and postpartum thyroiditis. It is important to observe postpartum women who have thyroid dysfunction in pregnancy. Women who have thyroid disorders can usually breastfeed. Footnote 117
There are no Canadian national guidelines on thyroid disorders in pregnancy or postpartum. The Guidelines of the American Thyroid Association for the Diagnosis and Management of Thyroid Disease During Pregnancy and the Postpartum offers advice on diagnosing and managing thyroid conditions during the postpartum period and breastfeeding. Footnote 198
Symphysis pubic dysfunction (SPD) has been described as a collection of signs and symptoms of discomfort and pain in the pelvic area, including pelvic pain radiating to the upper thighs and perineum. Footnote 199 Footnote 200 Footnote 201 While this term has been used to describe pregnancy-associated pain and instability and dysfunction of the symphysis pubis joint (SPJ) or sacroiliac joint (SIJ), the European Guidelines recommend pelvic girdle pain (PGP) as the accepted umbrella term. Footnote 201 PGP symptoms occur due to pelvic ligament relaxation and increased joint mobility in pregnancy, and can vary from mild discomfort to severely debilitating pain. Footnote 202
About 20% of pregnant women experience PGP. Footnote 201 Footnote 203 Risk factors for developing PGP during pregnancy include a history of previous low back pain and previous trauma to the pelvis. Footnote 201 Prolonged and difficult births, often with larger babies, with the women’s legs widely abducted, and possibly assisted by forceps, can also be contributing factors. The reported incidence of clinically persistent PGP from the postpartum stage to 2 years after childbirth ranges from 5% to 8.5%. Footnote 204
In severe cases, the symphysis pubis may partially or completely rupture. Diastasis of the symphysis pubis (DSP), where the gap in the symphysis pubis increases to more than 10 mm, can only be confirmed by diagnostic imaging. Footnote 205 Footnote 206 DSP can occur during pregnancy, childbirth, or the postpartum period. Footnote 206 Although specific recurrences are difficult to predict, women need to be made aware of the high recurrence rate (68–85%) in subsequent pregnancies. Footnote 207 A small subgroup of patients with PGP can develop chronic pain leading to high disability with resistance to physical interventions. These women should receive multidisciplinary care involving medical and psychological intervention.
There are no Canadian guidelines on diagnosing and managing PGP. Guidelines from Ireland and the United Kingdom are consistent in their message that symptoms of pelvic girdle pain are often mild but can be seriously disabling. Footnote 206 Footnote 208 Women should be asked at every postpartum contact whether they are experiencing pelvic girdle or lower back pain. Footnote 206 Footnote 209 Indications of pain and difficulty with walking after giving birth may indicate pubic symphysis diastasis and should not be discounted as a “minor discomfort of childbearing,” but investigated. Do not discount any level of pain—rather, undertake a careful clinical assessment to determine the extent of the pain and any symphysis pubis dysfunction. Assessments should include determining what occurred during pregnancy and childbirth, and running diagnostics and making timely referrals, including to physiotherapy, to avoid long-term and potentially permanent disability. Footnote 201 Footnote 209
In 2016/2017, 13% of women who gave birth in Canada had an assisted vaginal birth, 9% had a vacuum birth, and 4% had a forceps-assisted birth. Footnote 210 Recent evidence reviews have shown that women who had an assisted vaginal birth were more likely than those who had a spontaneous birth to have at least one health problem during the early postpartum period, for example, painful perineum, constipation, hemorrhoids, breakdown of stitches, and urinary or fecal incontinence. They were also more likely to have a painful perineum at 8 weeks postpartum, regardless of whether they had an episiotomy. Footnote 59 Footnote 177
Forceps-assisted and vacuum-assisted births are associated with an increased risk of injury to the vagina, perineum, and anus. Tears are more severe, which may require prolonged healing. Footnote 211 Women who have a forceps-assisted birth have a significantly greater decrease in intra-anal pressure and a greater incidence of a weak pelvic floor. Footnote 212
It is important to focus on the woman’s comfort during the postpartum period, determining if she has any concerns about perineal comfort or healing, as well as pain, discomfort or stinging, odour, incontinence, or dyspareunia. Footnote 24 The integrity and progress in healing of the perineum needs to be assessed, with pain relief or comfort measures offered and their effectiveness assessed. Women need information on the use of ice packs to decrease swelling, care of the perineum, self-inspection, warm water sitz baths, and Kegel exercises to improve perineal tone. Footnote 41
A significant number of women experience urinary and fecal incontinence following childbirth. The condition is both physically and psychologically challenging, and can influence many aspects of women’s lives and recovery.
Urinary Incontinence
During pregnancy and childbirth, the pelvic floor muscles are stretched and weakened, placing women at risk for the development of urinary incontinence. Footnote 213 While urinary incontinence can happen during pregnancy, stress urinary incontinence results from pelvic floor trauma during vaginal birth, especially the first birth. Although antenatal urinary incontinence, obesity, and significant perineal trauma are risk factors, clinical studies have not identified any single responsible event, suggesting that the problem is multifactoral. Footnote 212 Footnote 213 Footnote 214
Some women have temporary urinary incontinence, but others have long-term problems. Footnote 213 According to the Maternity Experiences Survey, 3.4% of all women who gave birth reported urinary incontinence as “a great deal of a problem” in the first 3 months postpartum. Footnote 215 Women who had vaginal births were more likely to report this problem (4.2%) than women who had caesarean births (1.1%). First-time mothers were also more likely to report this problem (4.0%) than multiparous women (2.9%). Footnote 215
Research indicates that women who had a forceps-assisted birth (with or without an episiotomy) were 10 times more likely to have significant perineal trauma than women who delivered by vacuum extraction without an episiotomy. Moreover, 5 years later, almost half of the women who had assisted vaginal births had some degree of urinary incontinence. Footnote 59
When talking with women about urinary incontinence, focus on prevention, muscle toning techniques, and other interventions. Pelvic floor muscle training can prevent urinary incontinence for up to 6 months after first-time mothers have given birth. Footnote 216 There is also evidence that pelvic floor muscle training is appropriate for women with persistent postpartum urinary incontinence. Footnote 216 The effectiveness might be increased with targeted approaches.
The SOGC recommends Kegel exercises for incontinence with follow-up to assess their effectiveness. Combining any necessary lifestyle changes with bladder training plus pelvic muscle exercises is highly effective. Refer to the SOGC guidelines Conservative Management of Urinary Incontinence . Footnote 217
Urinary Retention
Urinary retention is a sudden inability to spontaneously void the bladder or where a woman passes small amounts of urine but is unable to fully empty her bladder. Footnote 218 Footnote 219 Footnote 220 Symptoms of urinary retention include urinary frequency, voiding small amounts, bladder discomfort or pain, straining to void, reduced sensation to void, incomplete emptying of the bladder and urinary incontinence. Footnote 221
Postpartum voiding dysfunction is defined as failure to pass urine spontaneously within 6 hours of vaginal delivery or the removal of a catheter. Footnote 218 If urinary retention is not detected and managed, it can lead to bladder distention or underactivity and longer-term problems such as incontinence and urinary tract infections. Footnote 222 Footnote 223
The causes of urinary retention are not well understood, but likely mechanical, physiological, and neurological factors are involved. Footnote 220
There are no national Canadian guidelines on postpartum urinary retention, but NICE guidelines recommend that if a woman has not passed urine within 6 hours of childbirth, she has warm baths or showers to assist urination. If these actions are not successful, bladder volume should be assessed and catheterization considered. Footnote 24
Fecal Incontinence
According to the Maternity Experiences Survey, 1.8% of all women who gave birth reported that loss of bowel control was most pronounced in the first 3 months postpartum. Footnote 215 First-time mothers were more likely to report this problem (2.2%) than multiparous women (1.4%). Footnote 215 Anal incontinence after childbirth is more prevalent among women who have had a forceps-assisted birth and laceration of the anal sphincter. Footnote 224 Footnote 225 In addition, women who have anal sphincter tears are more than twice as likely to report postpartum fecal incontinence than women without sphincter tears. Footnote 224 Footnote 225
For women who had an OASIS repair, the SOGC recommends prescribing laxatives and non-steroidal anti-inflammatories and acetaminophen as first-line agents, and a single dose of an intravenous antibiotic. HCPs will want to discuss the degree of injury and arrange for appropriate follow-up. The SOGC also recommends that women with anal incontinence be referred for pelvic floor physiotherapy. Footnote 178
Having to remain in hospital for a prolonged period after childbirth can be extremely stressful for families. Mothers may be distanced from their support circle of friends and family. Concerns regarding contact with and care of other children may be a source of stress. Families may be worrying about the mother’s health and the care of siblings; contact with other children and grandparents; travelling logistics to and from the hospital; and work obligations of partners. It is important that HCPs explore these issues with the family and support them as much as possible. Consider referrals to social services if needed and innovative technology-based programs and resources to help keep families connected. When women are sole-parenting, prolonged stay situations can escalate their stress and anxiety and interfere with their recovery.
A prolonged hospital stay requires compassionate and individualized care. Policies should focus on enabling skin-to-skin contact, supporting breastfeeding, and allowing mothers and babies to be together (rooming-in/mother–baby care). Footnote 23
Mothers who are breastfeeding should have the opportunity to feed frequently and on cue for as long as they want and receive help with breastmilk expression, if needed. Footnote 226 If the baby cannot be given their mother’s breastmilk, pasteurized human donor milk is the next best choice. Footnote 20 Footnote 93 Footnote 227 It is incumbent upon HCPs to consult expert resources to determine the effects on the breastfeeding mother and breastfed baby of any medications the mothers is taking. Only a small number of medications are contraindicated while breastfeeding. Footnote 228
5. Complications Related to the Newborn
According to findings from the ACoRN program, complications related to the newborn fall into eight areas of concern:
- Cardiovascular
- Respiratory
- Neurological
- Gastrointestinal or surgical
- Glucose and electrolytes
- Thermoregulation
Refer to the CPS ACoRN program for guidance on neonatal stabilization, support for multidisciplinary teams, and identifying and caring for babies who are unwell or at risk of becoming unwell in the first few hours or days after childbirth. Footnote 119
If the baby has an infection, supportive care with adequate time to share information is essential. The mother and baby should be considered a unit—with non-separation the goal at all times.
Refer to the CPS guidelines for the diagnosis and treatment of infectious disease in newborns.
With the introduction of guidelines for systematic maternal screening and increased use of intrapartum antibiotics, the incidence of group B streptococcal (GBS) sepsis has decreased from 1.7 cases per 1000 live births in 1993 to 0.22 cases per 1000 live births in 2016. Footnote 229 Footnote 230 Despite this, GBS remains the leading cause of neonatal infection in Canada. In 2012, 48% of the cases of early onset neonatal sepsis were due to GBS, while Escherichia coli accounted for 31%. Footnote 231
Evaluating the risk of sepsis is an important part of the newborn assessment. Prompt treatment prevents the progression to severe disease. Babies at risk for sepsis are those where the mother has maternal GBS colonization in the current pregnancy or GBS bacteriuria; a previous baby with invasive GBS disease; prolonged rupture of membranes (≥18 hours); and maternal fever (temperature ≥38 °C).
The CPS guideline Management of Term Infants at Increased Risk of Early Onset Bacterial Sepsis recommends that any newborn with clinical signs suggestive of sepsis immediately undergo diagnostic evaluation and receive antibiotic therapy. The initial signs of sepsis may be subtle; they include respiratory distress, temperature instability, tachycardia, seizures, hypotonia, lethargy, poor peripheral perfusion, hypotension, and acidosis. Refer to this CPS guideline for diagnosis and management of sepsis.
The care of apparently healthy babies who have risk factors should be individualized. The care will depend on the number of risk factors and whether maternal intrapartum antibiotic prophylaxis for GBS was used. The CPS guideline Management of Term Infants at Increased Risk of Early Onset Bacterial Sepsis has recommendations for various clinical situations and the care of infants who appear healthy but nevertheless have risk factors.
Cardiorespiratory distress in the newborn may occur immediately after childbirth or later in the postpartum period. All HCPs caring for newborns must be able to assess respiratory distress, cyanosis, and perfusion. The CPS recommends that all centres in which babies are born have personnel capable of initiating assisted ventilation. Footnote 232 They also recommend following Neonatal Resuscitation Program guidelines for specific resuscitation procedures immediately after the birth and having a written policy regarding the initial care of a baby with respiratory distress outside of each birthing room in each facility. Footnote 232 Regular simulation sessions or other forms of practice scenarios are useful opportunities for continuing education and maintenance of skills.
Heart murmurs are common in the first few days of life and do not normally indicate a significant problem. In the first 24 hours, murmurs are often indicative of flow through the patent ductus arteriosus and disappear following the closure of the ductus. However, any murmur, even within the first 24 hours, must be assessed in the context of the entire physical examination. If a murmur persists or is symptomatic, a more complete evaluation is recommended. Footnote 233 Footnote 234
The incidence of CCHD in Canada is 3/1,000 live births and accounts for more deaths than any other congenital malformation. Between 10% and 30% of CCHD diagnoses are not made prior to discharge from hospital. Early diagnosis and follow-up are essential first steps in preventing infant mortality and morbidity. Footnote 98 Pulse oximetry screening, used in conjunction with prenatal ultrasound and physical examination, is the best approach to detecting CCHD in newborns. Footnote 99
The definition of hypoglycemia in the newborn is controversial. Multiple reviews have concluded that no specific glucose concentration can be linked to clinical signs or neurological injury. Footnote 235 Approximately 12% to 14% of healthy, appropriate-for-gestational-age (AGA), breastfed, term newborns have blood glucose levels of less than 2.6 mmol/L in the first 72 hours of life. Footnote 236
The CPS does not recommend routine blood glucose monitoring in healthy term babies. Footnote 237 Footnote 238 However, it is important to routinely screen babies at risk for hypoglycemia, including babies of mothers with diabetes (gestational and preconception), preterm babies, and both small-for-gestational-age (SGA) (weight < 10th percentile) and large-for-gestational-age (LGA) babies (weight > 90th percentile). The general recommendation for this population is that glucose levels be maintained at 2.6 mmol/L or higher after the first 2 hours of age.
Blood glucose screening of asymptomatic at-risk babies should begin at 2 hours of age and continue at a frequency and duration that depends upon the specific risk factors and until pre-feeding glucose levels have been consistently documented. Footnote 235 Footnote 238 Babies who are unwell or show signs of hypoglycemia, such as jitteriness, lethargy, poor feeding, apnea, or tachypnea, require immediate testing.
Approaches to the management of hypoglycemia depend upon whether it is asymptomatic or symptomatic. Early and frequent skin-to-skin contact and breastfeeding is encouraged in asymptomatic babies, with supplementation with expressed breast milk the next best approach. A breast milk substitute may be considered, if essential. Footnote 238
Refer to the CPS guideline Screening and Management of Newborns At Risk for Low Blood Glucose for information on diagnosis, monitoring, and management of hypoglycemia. Footnote 238
Selective serotonin reuptake inhibitors (SSRIs) are the antidepressant medications most frequently prescribed for the general population and pregnant women. Footnote 239 When considering prescribing or discontinuing SSRIs, HCPs are expected to weigh the potential harms of untreated depression or anxiety against potential risks to the fetus or newborn. SSRIs as a group have not been found to increase risk of major congenital malformations when used in the first trimester. However, paroxetine use in the first trimester may increase the risk of cardiovascular malformation, and other SSRIs may increase the risk of specific birth defects. Footnote 240
Third trimester use of SSRIs has been linked to a constellation of neonatal signs including prolonged crying, jitteriness, increased tone, tachypnea, cyanosis and feeding difficulty. Footnote 241 These signs occur in 10% to 30% of babies exposed to SSRIs in utero, usually within several hours of birth. The signs are usually mild—sometimes so mild they are difficult to identify—and resolve over several weeks. Footnote 242 Footnote 243 The mother is the best person to settle her baby with skin-to-skin contact, breastfeeding, and holding and comforting – the HCP’s role is to support her in caring for her baby and to provide a calm, quiet environment.
The CPS recommends observing the baby in hospital for 48 hours when SSRIs have been used during the third trimester. Footnote 240 However, since the majority of babies exposed to SSRIs are born healthy, Perinatal Services BC recommends considering discharge after 24 hours for babies who show no adverse signs or symptoms and who meet the following criteria:
- normal vital signs and oxygen saturation levels for the first 24 hours and at discharge;
- a normal physical exam;
- established feeding;
- well-regulating temperature; and
- no signs or symptoms of neonatal abstinence syndrome (NAS). Footnote 244
It is important to inform families about the possible effects of SSRIs on their baby and about strategies to support babies with symptoms. Postpartum use of SSRIs is not a contraindication to breastfeeding. Footnote 240 While information about long-term neurodevelopmental outcomes after prenatal SSRI exposure is largely reassuring, evidence in this area is limited.
Refer to the CPS guideline Selective Serotonin Reuptake Inhibitors in pregnancy and infant outcomes on caring for babies with SSRI exposure. Footnote 240
Small for Gestational Age
Babies who are born small for gestational age (SGA) have a birth weight below the 10th percentile of the age- and gestation-specific birth weight. The rate of SGA births has increased steadily between 2008 and 2014, from 8.2 to 9.1 per 100 singleton live births in Canada. Footnote 245
Intrauterine growth restriction (IUGR) describes genetic or environmental factors preventing a fetus reaching its growth potential. Low birth-weight is defined as weight at birth of less than 2500 grams (5.5 pounds) irrespective of gestational age. Footnote 246
Babies with SGA have physical characteristics (behaviour, alertness, spontaneous activity, and feeding ability) similar to those of normal-sized babies of like gestational age. They may look small and thin because they have decreased subcutaneous fat tissue and muscle mass, but they do not have the complications related to organ system immaturity that preterm babies of similar size have. Any complications are usually a function of the underlying cause of the SGA. Footnote 247
Parents and families of babies who are born SGA are anxious about their baby’s well-being and require supportive care, counselling, and reassurance. Caring for the mother–baby unit, non-separation, and supporting breastfeeding are all essential aspects of care.
There is no consensus on the definition of fetal macrosomia, which some define as birth weight of more than 4000, 4500, or 5000 g, regardless of the baby’s gestational age. Others define macrosomia as a baby above the 90th birth-weight percentile for gestational age of a reference population—also known as large-for-gestational-age (LGA) babies. Footnote 248 The description normal birth weight depends on the population of reference.
In Canada, the LGA birth rate among singleton babies decreased from 11.6 to 10.2 per 100 singleton live births between 2005 and 2014. Footnote 245 Babies born with macrosomia are at higher risk of perinatal mortality (stillbirth and early neonatal, late neonatal, and post-neonatal mortality) and have a higher risk of shoulder dystocia, asphyxia, congenital anomalies, infection, and SIDS. Footnote 248
In addition, these babies are more likely to be born with a lower than normal blood sugar level, have a higher risk of childhood obesity, and a higher risk of metabolic syndrome during childhood. Footnote 249 Babies with macrosomia should be assessed for low blood sugar and jaundice and be encouraged to feed soon after the birth to prevent low blood sugar. Footnote 250
Neonatal opioid withdrawal symptoms are a group of possible symptoms experienced by babies whose mothers used opioids during pregnancy. From 48% to 94% of babies exposed to opioids in utero have opioid withdrawal symptoms. Footnote 251
While their symptoms vary, babies who have been exposed to opioids in utero may feed poorly and have diarrhea and weight loss. They may demonstrate tremors, tight muscle tone, excessive crying, hyperactive Moro reflex (sometimes called the startle reflex), irritability, vomiting and convulsions, hyperthermia and tachypnea. Footnote 252 Footnote 253 If these signs become sufficiently severe, and depending on the drug that the baby was exposed to, the baby may require pharmacotherapy.
The CPS recommends that all babies exposed to opioids be assessed using a scoring system that measures the severity of withdrawal symptoms and helps determine the need for additional monitoring, nursing, medical intervention, or pharmacological therapy.
Refer to the CPS practice point Managing Infants Born to Mothers Who Have Used Opioids During Pregnancy for details. Footnote 253
The CPS also notes that the length of stay in hospital varies depending on exposure to opioids prenatally, severity of withdrawal, symptoms, treatment, and social factors. The Society recommends observing babies for a minimum of 72 to 120 hours, depending on their exposure to opioids. If the treatment threshold is not reached within that time, the baby can be discharged. The key to a successful transition home is to ensure continuity of care by an interprofessional team, with anticipatory planning for when the baby meets criteria for discharge. Footnote 253
It is important that babies be cared for in their mothers’ rooms. Having in place a protocol for rooming-in and use of morphine (if required) for opioid-exposed babies helps to reassure staff about the safety of this treatment modality and supports them in caring jointly for the mothers and their babies. The BC Perinatal Services and British Columbia Centre on Substance Use guideline Treatment of Opioid Use Disorder During Pregnancy Guideline Supplement offers a sample rooming-in protocol for opioid-exposed neonates. Footnote 252
Encourage mothers to hold and cuddle their baby as much as possible, as this helps to settle the baby and minimize withdrawal. In addition, if the mother is relaxed, the baby is more likely to relax. Also encourage breastfeeding, as this can delay the onset and decrease the severity of withdrawal symptoms as well as decrease the need for pharmacological treatment. Footnote 253 Footnote 254 Consider that even babies who do not have in utero exposure to opioids usually take at least 36 to 72 hours to settle until the mother’s breast milk comes in and breastfeeding is established.
If the baby requires pharmacotherapy, the mother and baby may be subject to a prolonged hospital stay. It is important to inform the mother during her pregnancy that she and her baby may need to stay longer at the hospital so that she has a realistic understanding of the early postnatal period and be better prepared for any additional care her baby may require. Note that rooming-in and non-pharmacological care often reduce withdrawal signs to the extent that pharmacotherapy treatment is not required. Footnote 252 Footnote 253
Mothers who used opioids during pregnancy may experience a range of emotions; for example, anxiety over the well-being of their baby, concerns about withdrawal signs the baby is showing, and worries about maintaining custody, or they may be confident and relaxed. It is essential to individualize care to support the mother and other caregivers.
The CPS practice point Managing Infants Born to Mothers Who Have Used Opioids During Pregnancy discusses discharge criteria relating to the newborn and referral to support services and family services be considered. Footnote 253 In the Treatment of Opioid Use Disorder During Pregnancy Guideline Supplement , the BC Perinatal Services and British Columbia Centre on Substance Use advise that maternal opioid use alone is not grounds for the apprehension of a baby by authorities or referral to child protection. Make the decision to report on a case-by-case basis, in consultation with the entire health care team, although HCPs should be aware of their legal obligations in this regard. Footnote 252
Late preterm babies (34 +0 to 36 +6 weeks of gestation) vary widely in physiological maturity. The late preterm baby may have inadequate thermoregulation, immature and weak suck and swallow patterns, incomplete adaptation of certain enzyme systems, and poor immunological and respiratory defence systems. Footnote 255 These factors contribute to increased risk of death and morbidity compared to full-term babies. Common problems are hypoglycemia, hypothermia, respiratory distress, infections, increased risk and delayed onset of hyperbilirubinemia, feeding issues, increased hospital readmission rates, and growth failure. Footnote 256 Early term babies (37 +0 to 38 +6 weeks of gestation) are at increased risk for the same problems as late preterm babies, with increased likelihood of admission to NICU. Footnote 257
An assessment at birth to confirm the baby’s gestational age and ongoing monitoring are important to determine the treatment plan. Delay in adaptation might require admission to NICU, while mature late preterm babies can be cared for in regular postpartum care. In both situations, it is important to avoid separating the mother and baby. Footnote 255
Screen for hypoglycemia and hyperbilirubinemia according to the CPS Screening Guidelines for Newborns at Risk for Low Blood Glucose and Guidelines for Detection, Management and Prevention of Hyperbilirubinemia in Term and Late Preterm Newborn Infants . Continued breastfeeding support is necessary to establish feeding and prevent readmission.
The CPS guideline Safe Discharge of the Late Preterm Infant provides detailed criteria for hospital discharge and post-discharge follow-up. Footnote 255 Some key criteria include stable vital signs for at least 12 hours prior to discharge, 24 hours of successful feeding, and avoidance of mother–baby separation before discharge by providing flexible accommodation arrangements for parents. Arrange for a follow-up appointment within 24 to 48 hours of discharge with a community-based HCP, prior to the baby being discharged home.
Instrumental birth involves use of a vacuum extractor or obstetrical forceps. Trauma is the major complication of instrument-assisted birth in the newborn. Trauma may be caused by head compression and traction on the fetal intracranial structures, face, and scalp or by suboptimal instrument placement. Footnote 258 The most serious sequelae of trauma is intracranial hemorrhage, which occurs in 16 to 17 per 10 000 births. Footnote 259 Footnote 260
The overall risk to the newborn from assisted vaginal birth is low. The risks that could occur include bumps, bruises, or marks on the baby’s head or face that heal in a few days or weeks; cone-shaping of the head, which returns to normal within a day or two; injuries to the baby’s scalp, head, and eye; injuries to the nerves in the arm or face—the baby’s face muscles may droop if the nerves are injured but go back to normal when the nerves heal. Footnote 177 Footnote 211 Subgaleal hemorrhage is a very rare but serious outcome. Footnote 177 Footnote 211 If the baby has any trauma from an assisted birth, it is important that the mother and family understand the cause, the care required, and the anticipated outcome.
Refer to the SOGC Advances in Labour and Risk Management (ALARM) course for assessment, monitoring, and care of the newborn with subgaleal hemorrhage.
Along with the joy of birth and the delight of welcoming a baby into the family, parents whose babies are born with congenital anomalies or rare conditions have special needs and may feel a sense of loss. Many factors influence parents’ experience of having a baby with an anomaly: their personal beliefs, culture, and support network; their HCPs’ knowledge and attitude; how the diagnosis is communicated; the information that they are given about their baby’s diagnosis and what they can expect; and their connection to appropriate services and support groups. Footnote 261
In these situations, base all communication on compassion, using clear and simple terms. Footnote 262 Parents require access to the most current information about their baby’s condition in a form they can understand. Footnote 263 They need to understand the immediate care plan and know what to expect in the future. Footnote 261 They should also be told about the necessary resources available —medical services, clinics, specialists, therapy (e.g., physical, occupational, speech, vision), breastfeeding support, dietitians, mental health services, recreation services, and support groups.
When babies are born with anomalies or rare conditions, a team approach to the family’s care is always required. Parents will often be referred to genetics services to help in the diagnosis of their baby. They could also be referred to genetics counselling if they have concerns about future pregnancies.
HCPs are encouraged to take extra time to communicate with the parents and family—including significant family members such as grandparents and siblings. Show compassion, listen carefully as the parents and family express their concerns and feelings, and communicate in a way that everyone can understand. It is also important to ensure privacy when discussing the baby with the parents or family.
It is critical to remind parents and family (often repeatedly) about what to expect when they are caring for their baby. When parents are first told about their baby’s diagnosis, they are often overwhelmed to the point that they are unable to retain information. A designated HCP should follow up with parents through the postpartum period and to repeat information in subsequent meetings, to assess their ability to cope, and to refer them to appropriate services. Footnote 261
Referrals to peer support can be helpful to provide parents with a shared social identity and contribute to feelings of hope. Footnote 264 Peer support can include face-to-face or online support groups relevant to the baby’s specific condition.
A baby remaining in hospital (especially in the NICU) for an extended period can create a great deal of stress for parents and families. The kind of care that the baby receives, and the approach to care, affects not only the baby’s physical well-being but also parent–baby attachment, feeding, neurodevelopmental outcomes, and the overall health and well-being of the baby, parents, and family. The parents and family may be experiencing extreme emotions such as anxiety or depression, or conflicting feelings such as the joy at the birth of their baby and the fears for the baby’s well-being and their ability to provide care.
NICU environments that facilitate shared decision-making and partnerships between parents and professionals and enable parents to be their baby’s primary caregiver, create a more consistent care for the baby. They also protect the baby from trauma associated with the NICU, such as isolation, stress, and lack of support during painful procedures, and provide parents with the opportunity to develop confidence and skill in caring for their babies. Footnote 30 Footnote 265 Footnote 266
Critical elements of family-centred care include: unrestricted presence of the parents, 24/7; parents and family as primary caregivers for their babies with the support and guidance of HCPs; and open, continuous communication. Footnote 267 The basic principles of family-centred care in this context are the same as all family-centred care—dignity and respect, shared decision-making, choice, information exchange, empowerment, and collaboration. Footnote 267 Footnote 268
Improvements in the baby’s weight gain, decreased parental stress and anxiety, and increased high frequency exclusive breastfeeding at discharge are some of the demonstrated benefits of family-centred care in the NICU. Footnote 269 Footnote 270 Others include decreased length of stay, enhanced attachment between parents and babies, and greater family satisfaction. Footnote 267 Footnote 270 Family involvement is critical to enabling all babies to reach their full physical, cognitive, and psychosocial development—including those babies in the NICU. Footnote 270 Footnote 271
The Family-Integrated Care (FICare) model is an extension of the principles of family-centred care, with parents as true partners in their baby’s care within the NICU. This model was developed by a health care team that included parents whose babies had been in the NICU and follows research in Estonia. Footnote 29 Integrating parents into the care team in FICare goes well beyond merely allowing parents to be present and observing their baby’s care. Footnote 272 Rather, parents provide most of the care for their baby while HCPs guide and counsel parents. Footnote 29 Footnote 30
Single-family NICU rooms are now in use in a few centres in Canada as well as in the USA and Europe. The single-room setting has a number of benefits: it provides optimal environmental support to parents; reduces neonatal sepsis; improves baby weight gain; improves breastfeeding rates; improves control of excessive noise and light; improves staff and parental satisfaction with care; reduces parental and staff stress and anxiety; and costs the same, or possibly less, than standard NICUs. Footnote 269 Footnote 273 Footnote 274 Footnote 275 Footnote 276 Footnote 277 Single-room care has not been associated with any increase in adverse outcomes. Footnote 275
The stressful environment of the NICU may add to the risks facing preterm or sick babies due to their physiological vulnerabilities, negatively impacting their growth, with the brain particularly affected. Developmental care refers to a range of strategies designed to reduce the stresses of the NICU and include control of external stimuli, improved clustering of care activities, and positioning or swaddling of the preterm baby. Footnote 278 Footnote 279 While more research is needed, developmental care interventions has demonstrated benefits to the outcomes of preterm babies. Footnote 279
Some families, including Indigenous families and those living in rural and remote areas, may be far from home and have to travel for the birth or if the mother and child are transferred to another facility after the baby is born. Prolonged hospital stays can be particularly stressful for these parents, as they are away from extended family members, friends, and support networks. They may have other children back home, which can cause additional stress.
Providing Family-Centred Care in the NICU Footnote 29 Footnote 268 Footnote 269 Footnote 270 Footnote 271 Footnote 280 Footnote 281
- Are full partners in decision-making and caregiving and are integrated into the NICU team;
- Have unlimited access to their babies and rooming-in, 24/7;
- Are supported by HCPs in aspects of care, such as prolonged skin-to-skin contact, breastfeeding, and providing developmentally appropriate care so that they become competent in their caregiving;
- Are supported in their baby’s care to minimize their baby’s stress and pain, to safeguard their sleep, and protect their baby’s skin;
- Participate in care planning—in rounds and having access to their baby’s records;
- Receive psychosocial support from the interprofessional team, including psychologists, and peers; and
- Are enabled to express their emotions and fears.
Health care providers: Footnote 29 Footnote 267 Footnote 269 Footnote 270 Footnote 271 Footnote 280 Footnote 281 Footnote 282 Footnote 283
- Provide care based on interprofessional collaboration and partnerships with family and other professional providers;
- Include parents as full partners in decision-making and care;
- Shift their role from skilled provider to one of guidance, supporting parents in their role as primary caregivers, 24/7;
- Focus on promoting baby–parent interactions, stressing the critical importance of parents’ presence and rooming-in, and assuring them of unlimited 24-hour information and access to their baby;
- Support parents in a compassionate, respectful way, recognizing their individual needs;
- Support parents in skin-to-skin contact with their babies;
- Support mothers in breastfeeding and feeding their babies breast milk;
- Communicate with families openly and honestly, and spend time listening to the families’ experiences, fears, and concerns;
- Communicate warmly, regularly, in an understandable fashion, and in a culturally appropriate and safe manner;
- Share information between themselves and with parents;
- Are aware of the possibility of posttraumatic stress disorder (PTSD), and screen for depression; and
- Are supported by system leadership who are committed to an integrated team approach to the needs of babies, families, and staff.
Policies: Footnote 29 Footnote 267 Footnote 269 Footnote 270 Footnote 271 Footnote 280 Footnote 284
- Are supported by a clear vision;
- Have full leadership and administrative support;
- Stipulate unlimited access and preferably rooming-in 24/7 and information for parents;
- Stipulate that parents are integral members of the care team, not visitors, and are their babies’ primary caregivers, sharing in decision-making;
- Create opportunities for the participation of parents in support systems;
- Stipulate that HCPs communicate regularly with parents and provide mechanisms to do so;
- Ensure adequate staffing for the model of care in the unit;
- Support ongoing professional development for NICU staff;
- Actively involve parent partners and advocates in the development and monitoring of policies to inform quality improvement, and develop systems to accommodate this; and
- Support early and frequent breastfeeding or breast milk expression, meetings with lactation consultants and adequate follow-up—with a written policy.
Infrastructure and supports Footnote 267 Footnote 271 Footnote 283 Footnote 285 Footnote 286
- The physical setting is supportive of the baby’s well-being and neurodevelopment, i.e., in a single room with enough space and resources to support parents’ presence (e.g., with showers, kitchen, laundry, lounge, etc.) so that the parents can stay in the room with their baby 24/7 (or sleeping rooms available).
- The interprofessional team give the parents psychological and social support, and they have access to peer support.
- The physical environment supports the breastfeeding mother, e.g., provides for intimacy and means of expressing breastmilk, etc.
- Educational materials are available in plain language in a variety of formats (e.g., in writing, video, apps, etc.).
- Mechanisms in place enable parents’ involvement in their baby’s care and inform them of their baby’s well-being, even when they are not present (e.g., by using web cameras).
- Preparation for the transition home begins at the baby’s admission to the NICU, by providing information on the criteria for discharge and baby care, supporting parents to care for their baby, assessing the parents’ social supports, and providing referrals to appropriate services.
- Care planning for the transition to home includes coordination of health and social care plans with any applicable community services, which may require multi-agency collaboration.
6. Late Postpartum
New parents have many different emotions after the birth of their baby. They may feel full of joy and wonder, anxious, overwhelmed, worried and tired. Having a baby brings a myriad of changes—and is very demanding. It takes months or even years to adapt to these changes. Becoming a parent is a deeply significant personal and social transition that involves a change of identity.
When caring for the new mother and her family, the goal of HCPs is to assist her in this transition and recognize and support her role in caring for her baby and nurturing their interdependent relationship. It is critical to spend time listening to mothers and families and to provide support based on their individual needs and experiences.
Providers should let new mothers know that they have faith in them and their ability to care for themselves and their baby. Providers can also help them listen to their intuitions and learn from their experiences so they become more and more confident in their new role. With time, the mother can discover her strengths and her own way of doing things. Footnote 287
Relationships with a partner and family are also undergoing transition. Communication is the key to nurturing these relationships. Talking about feelings, worries, and happiness during this intense period can help keep couples and/or families close. Footnote 287
Healthy early childhood development includes the physical, social/emotional, and language/cognitive domains. Footnote 288 Many health, social, and justice issues later in life have their roots in early childhood. Parents need the supports of HCPs and community programs to assist them in fostering the optimal growth and development of their baby starting from birth.
Postpartum support in the community should be planned according to a family-centred approach to care, based on women’s experiences and needs, while respecting their diversity in the social and cultural contexts of their postnatal experience. Footnote 289 The woman and her partner and newborn belong at the centre of care, with strategies planned and provided to meet their needs, respecting the woman’s preferences and decisions, while ensuring she is treated with kindness, respect, and dignity. Footnote 29 Footnote 289 Footnote 290
Women, newborns, and families have different points of access to postpartum care in the community. These often involve numerous HCPs (e.g., physicians, nurses, and midwives; lactation consultants and registered dieticians; social workers and psychologists) and community-based providers (e.g., postpartum doulas and maternal child health home visitors). They also seek and receive support from their family members and peers.
Successful postpartum support strategies in the community are holistic and comprehensive, applying an efficient and effective interdisciplinary approach to care. Footnote 289 Women should have multiple choices for the kind of supports that meet their needs. It is critical that women be provided with a first/consistent point of contact (for example, a public health nurse, midwife, or nurse practitioner) for when they need to reach out for support.
Hospitals, health centres, community-based organizations, and public health and primary care providers offer postpartum services in Canada. Some jurisdictions have centres that provide education, support, and programming for new mothers and young families. Various models are used, including phone calls, telephone triage services, clinic visits (drop-in and by appointment), and home visits. Footnote 215 With many providers and many groups providing care, and with a lack of coordination across settings, postpartum care runs the risk of fragmentation. As most women who give birth return home after a very short stay in the hospital or birthing centre, the coordination of support in the community is critical.
Planning postpartum care locally allows for the greatest efficiency and effectiveness. NICE guidelines recommend having a coordinating health care professional for each postpartum case and a documented, individualized care plan developed with the woman. Footnote 24 It is essential that mothers and families know about the specific community supports that are available to them in their area, perhaps in the form of a handout or website that lists the information.
While access to professional postpartum support within the community is essential for positive health outcomes for women, children, and families, social support networks have been identified as one of the key determinants of health. Footnote 291 It is also important that women have access to their own social support networks. Social media provides the opportunity for women to form virtual groups for support and information sharing. They can also access a variety of websites with evidence-based information, such as those of PHAC, provincial/territorial governments, and professional organizations, that can provide answers to questions on self and baby care. HCPs can help women identify the websites or social media sites that may be helpful and those that would be best to avoid because they are neither helpful nor evidence-based.
Optimally, planning for the postpartum period starts during pregnancy. Prenatal education classes may provide a source of postpartum support from other families going through the same experiences. Footnote 292
Appendix B provides descriptions of innovative international and Canadian postpartum care models and guidelines. Refer to Appendix C for an outline of the various methods used to deliver postpartum care in the community.
Continued postpartum support and care needs to be provided according to the principles of family-centred care. It is important to determine and respect the woman’s and family’s views, beliefs, and values. The mother should be fully involved in determining the timing and content of each postpartum contact with HCPs so that the care she receives meets her and her baby’s needs and is flexible. Footnote 24 Footnote 41
At each postpartum encounter, the mother and her partner should have the opportunity to express their feelings and concerns and talk about their physical and emotional well-being, breastfeeding, rest, pain or discomfort and any concerns to do with the baby. These encounters provide HCPs with the opportunity to explore how the mother is coping with her daily experiences and her family and social supports, and to encourage women and their families or partners to talk about any changes in mood, emotional state, and behaviour that are outside of the woman’s normal pattern. Footnote 24 HCPs will want to be aware of and look out for the signs of emotional health problems that occur during the weeks and months following birth.
Professionals have developed a number of methods—written standards of care, care plans, maps or paths, managed care, among others—to ensure that criteria for maternal and newborn health and adjustment are observed during the postpartum period. These criteria, also called indicators or outcomes , include specifics about the mother, the baby, and the family’s social or home support system. While these tools are useful, the focus should always be on supporting the mother and baby’s transition based on their individual needs and experiences.
HCPs are ideally positioned to recognize signs of family violence, including intimate partner violence, as well as child exposure to intimate partner violence and other types of child maltreatment. These forms of violence can negatively impact the health of mother and child, and the effects can persist over time. It is important that providers be equipped to recognize and respond safely to situations involving family violence, and to ensure that their interactions or interventions do not revictimize the mother or child.
According to the Maternity Experiences Survey, about 1 in 10 women who have given birth reported experiencing one or more acts of violence in the past 2 years, most often being pushed, grabbed, or shoved in a way that could have hurt them. Footnote 215 Over half (52%) identified their partner, husband, or boyfriend as the perpetrator of this violence. One-third (31%) experienced the violence during pregnancy, and 16% reported that the violence increased after the birth of the baby, 52% that it decreased, and 32% that it stayed the same. Of those women who experienced abuse, 61% reported discussing or receiving information about what to do if they experienced abuse. Footnote 215
Intimate partner violence has been associated with mental health disorders for women, most commonly depression and anxiety disorders, and PTSD. Other effects on mental health include poor self-esteem, sleep disorders, eating disorders, phobias and panic disorders, substance dependence, antisocial personality disorders, and psychosis. Footnote 293 Intimate partner violence is also associated with postpartum depression. Footnote 294
Child maltreatment includes physical, sexual, and emotional/psychological abuse as well as neglect. Exposure to intimate partner violence is also a form of child maltreatment. Footnote 295 Child maltreatment is a major public health issue associated with a broad range of negative health outcomes across the life course. Approximately one-third of Canadian adults (32%) report experiencing physical abuse, sexual abuse, and/or exposure to intimate partner violence before the age of 16 years. Footnote 296
Provincial/territorial child welfare legislation considers exposing a child to intimate partner violence/family violence a form of maltreatment, and HCPs are required to report it. Footnote 296
Violence in the home has a negative impact on babies, whether they experience it directly, for example, receive an injury while held during physical violence, or indirectly, due to their dependence on their primary caregivers for emotional support. Footnote 297 When the primary caregiver is involved in a stressful event, the child’s main source of comfort is a source of fear and distress. This repeated pattern can result in disorders of attachment, which may contribute to behaviour problems in later childhood. Babies and young children who experience repeated violence in the home have reduced capacity to regulate their emotions and behaviour because of their lack of emotional security. Footnote 297
Adverse Childhood Experiences (ACEs) research has shown that traumatic childhood events such as abuse, neglect, and household dysfunction are linked to an increased likelihood of developing physical, behavioural, and social problems in adulthood. Footnote 298
Canadian and WHO guidance do not recommend universal screening for intimate partner violence. Footnote 299 Footnote 300 HCPs are well-positioned to inquire about intimate partner violence when assessing conditions that may have been caused or complicated by violence. In the context of perinatal care, HCPs should consider asking about intimate partner violence during assessment and subsequently as needed. Footnote 300
Before inquiring about intimate partner violence, certain conditions of safety must be met. Safe responses to an adult’s disclosure follow the LIVES protocol: Listening; Inquiring about needs and concerns; Validating; Enhancing safety; and providing a variety of Supports. Footnote 301 The HCP will want to speak with the postpartum woman separately from her partner and any verbal children, and assess her (and any children’s) risk of immediate danger. After intimate partner violence is disclosed and immediate safety is discussed, assess the need for follow-up, considering what care and support is available, as well as the person’s strengths, needs, priorities, and preferences. Footnote 300
Postpartum nutrition and achieving a healthy weight following a pregnancy can impact maternal and child health both in the short and the long term. The SOGC states that postpartum women can achieve optimal nutrition by eating a variety of high quality foods and following the advice in Canada’s Food Guide .
Breastfeeding women have higher energy needs and should therefore eat a little more food each day than non-breastfeeding women. Canada’s Food Guide recommends regular intake of vegetables, fruit, whole grains, and protein foods. Deficiency of certain nutrients, including thiamin, riboflavin, vitamin B6, vitamin B12, choline, vitamin A, vitamin D, selenium, and iodine, can adversely affect the concentration in breastmilk. Footnote 302 Health Canada recommends that all women who could become pregnant, including breastfeeding women, take a daily multivitamin containing 400 mcg (0.4 mg) of folic acid. Footnote 302
Some women, for example those who live in low income, Indigenous women or women who are newly arrived in Canada or refugees, may be at higher risk of nutritional challenges. Footnote 303 Footnote 304 A lack of access to nutritious food, or to knowledge about nutritious food, can compromise women’s and families’ abilities to eat adequately. It is important that women receive nutritional counselling that is relevant to their specific needs and culture.
Refer to the SOGC guideline Canadian Consensus on Female Nutrition: Adolescence, reproduction, menopause, and beyond for components of the maternal diet that may affect those babies who are breastfeeding. Footnote 305
Postpartum weight
Weight loss during the postpartum period should be gradual. There is little evidence that gradual weight loss affects the volume and quality of breastmilk once lactation is established. Footnote 305 The SOGC emphasizes the need for optimal nutrition to achieve a healthy body weight postpartum. Postpartum visits can be opportunities to check on weight retention/reduction, healthy eating habits, and exercise.
Refer to the SOGC guideline Canadian Consensus on Female Nutrition: Adolescence, reproduction, menopause, and beyond for more information. Footnote 305
HCPs are well positioned to recognize circumstances that are cause for concern; for example, a sudden, rapid weight loss or, conversely, if a woman is living with obesity. The scientific knowledge about obesity and its treatment has led to the recognition that obesity is an illness and not a product of an inadequate lifestyle. It is important to avoid shaming and stigma. Footnote 306
Refer to the SOGC guideline Obesity in Pregnancy for recommendations on the counselling and care of women who have obesity.
Many factors influence a woman’s sexuality during the postpartum period: her culture, her experience before and during pregnancy, her relationship, her physiology, and her emotional and psychological state. Footnote 307 This is compounded by the experience of giving birth, fatigue, the physical recovery from labour and birth, the changes her body is undergoing postpartum, caring for her baby, and perineal pain or discomfort.
Faced with the physiological and emotional changes of becoming new parents, intimacy may be challenging for women and their partners to maintain postpartum, but it remains important for the health of their relationship. Both women and providers often find it difficult to discuss postpartum sexual changes, adjustment, and intimacy. However, sexual concerns are common among women, and they welcome their HCP raising the topic and offering support regarding any concerns that she and her partner may have. Footnote 308 Footnote 309
Low or no sexual desire is very common during the postpartum period. A lesser interest in sexual activity than before or during pregnancy is the norm during the first few months to a year after childbirth. Footnote 310 Footnote 311
Between 22% and 86% of women experience changes in sexual functioning postpartum, especially those who have had an assisted vaginal birth as opposed to a spontaneous vaginal birth or caesarean birth. Footnote 312 A number of studies have linked episiotomy or perineal lacerations and operative vaginal birth with dyspareunia, which can persist for a number of months. Footnote 313 Footnote 314 Women who have had a caesarean birth may also have discomfort with intercourse. Footnote 312 Footnote 315
Refer to the SOGC Female Sexual Health Consensus Clinical Guidelines and Sexual and Reproductive Health Counselling by Health Care Professionals for information on the assessment and sexual health care of postpartum women.
Contraception and Prevention of Sexually Transmitted Infection
Postpartum women need information about contraception and preventing sexually transmitted infections (STIs), and about what methods are compatible with breastfeeding. In this regard, the SOGC recommends the following: Footnote 316 Footnote 317
- Lactational amenorrhea method (LAM) can be used for the first 6 months if the woman’s periods have not returned and the baby is exclusively breastfed on demand day and night and is not fed other foods or liquids. Footnote 318 The woman will need to use another form of birth control once her period returns or the baby is older than 6 months, is no longer exclusively breastfeeding, is sleeping through the night, or has long intervals between breastfeeding. Footnote 318
- Postpartum women may be candidates for an IUC, which can be inserted immediately after delivery. However, women are at a higher risk for uterine perforation during insertion of the IUC in the first postpartum year.
- Hormonal contraceptives can be used by non-breastfeeding women from 3 to 4 weeks after they give birth. Some hormonal birth control methods may decrease milk production, but the progestin-only birth control pill does not appear to interfere with lactation. Currently available combined estrogen–progestin birth control pills do not interfere with the quantity or quality of breast milk once feeding is established.
- Condoms are an effective contraceptive option for breastfeeding and non-breastfeeding women. Condoms also protect both partners from STIs.
Refer to the SOGC guidelines The Canadian Contraception Consensus Guidelines for guidance on the use of contraceptive methods in postpartum and breastfeeding women to prevent pregnancy and STIs.
Immunization is a proven cost-effective public health intervention that prevents significant illness, disability, and death. Footnote 319 Vaccines work best when they are given on time, beginning in infancy. Children are immunized early in life because they are vulnerable to diseases and the consequences can be very serious. The vaccination schedule is designed to protect babies and children before they are exposed to vaccine-preventable diseases.
Periodic outbreaks of illnesses such as measles, which can cause death or disability, can result because not all Canadians are immunized. Footnote 320 PHAC reports that 23% of children have not received the full four recommended doses of the diphtheria, whooping cough (pertussis), and tetanus vaccine by the time they are 2 years old. Footnote 321 In the last 10 years, the number of measles outbreaks has increased in several provinces, with five of the outbreaks involving more than 10 cases. These outbreaks are largely a result of the importation of the virus from other countries, with vulnerable children, including those who are not immunized, contracting the illness. Footnote 322
Some parents may be hesitant or resistant to immunizing their babies. The reasons behind children not being fully immunized are complex and context-specific and often community-specific. A vocal few hold anti-vaccine views; they are not the main reason for the lack of coverage, although the number of vaccine-hesitant parents is growing. Some are complacent, taking vaccination rates and herd immunity for granted; some have doubts about the safety or necessity of vaccines, having been convinced by misinformation about adverse effects; while others do not get their children immunized because of the time and effort it can take to do so or they are concerned about the injections causing pain. Footnote 323
The CPS recommends that HCPs acquire the knowledge and skill to work with parents who are hesitant about immunization. Parents often look to HCPs for answers to their questions about immunization. HCPs will want to share evidence-based information about babies’ vaccinations in a manner that is easy for parents to understand and explore any reasons families may have for not immunizing. Footnote 324 Connecting with parents in order to maintain trust and keep the lines of communication open is critical. Each parent requires different information geared to his or her specific needs.
It is important to understand a parent’s specific concerns and to demonstrate care and compassion for both the child and the family. Telling stories about vaccine-preventable disease cases in Canada can help educate parents. Taking the time to convey information clearly, calmly, and effectively can make the difference whether a child is immunized. Footnote 325
Refer to the CPS practice point Working with vaccine-hesitant parents for more information.
The Canadian Immunization Guide, based on guidance from the National Advisory Committee on Immunization (NACI), provides guidelines for immunization of babies, children, youth, and adults, as well as specific recommendations for postpartum and breastfeeding women. The Canadian Immunization Guide includes the schedule for the following vaccinations for babies and toddlers up to 18 months:
- Diphtheria, tetanus, pertussis, polio
- Haemophilus influenza type b
- Pneumococcal disease
- Meningococcal disease
- Hepatitis B
Although NACI makes recommendations at the national level, provinces and territories determine specific programs and schedules. As such, HCPs need to refer to the immunization schedules of their respective jurisdictions.
It is critical that all siblings, parents, grandparents, other family members, and visitors have all their immunizations up-to-date when a baby comes home. This is particularly important if the baby or mother have underlying medical conditions or vulnerabilities that would increase their risk of communicable diseases like whooping cough and influenza.
The birth of a baby involves many transitions and adaptations for the woman, the baby, and the family. Parents feel many different things following the birth of their baby—joy, wonder and happiness, as well as anxiety, worry and fatigue. These are all normal feelings. Mothers adapt physically and psychologically following birth as they face lack of sleep, physical discomfort or pain and relationship changes. Caring for a baby is demanding, requiring many adaptations for parents. While the postpartum period is a normal, healthy time of life, it is also challenging for families, even as parents get comfortable with their roles.
Providing family-centred maternity and newborn care to women, their partners, and families during the postpartum period is an essential component of the care offered by all institutions, agencies, and programs. It is important that HCPs focus on the individual needs and values of the mothers, partners, newborns, and families they are working with. As women, their partners, and immediate families develop attachment and confidence in caring for their newborn babies, they will also require support from extended family and friends, in addition to providers and community programs.
Clinical Practice Guidelines Relating to Postpartum Health
- Alberta Health Services (PDF 3.54 MB)
- Canadian Paediatric Society
- Manitoba Health, Healthy Living and Seniors
- Ontario - Provincial Council for Maternal and Child Health
- Perinatal Services BC
- Reproductive Care Program of Nova Scotia
- Society of Obstetricians and Gynaecologists of Canada
Breastfeeding
- Agence de la santé et des services sociaux de la Capitale-Nationale - Guide pratique en allaitement pour les médecins
- Baby-Friendly Newfoundland & Labrador – Physician's Toolkit Breastfeeding: Quick Reference Guide (PDF 3.78 MB)
- Best Start – Breastfeeding Guidelines for Consultants - Desk Reference
- Health Canada – Nutrition for Healthy Term Infants
- Public Health Agency of Canada - Protecting, Promoting and Supporting Breastfeeding: A Practical Workbook For Community-based Programs
- Toronto Public Health – Breastfeeding Protocols for Health Care Providers (PDF 9.52 MB)
- Best Start - Giving Birth in a New Land: Strategies for Service Providers Working with Newcomers
- Canadian Nurses Association - Promoting Cultural Competence in Nursing (PDF 1.75 MB)
Environmental Health
- Best Start - Playing it Safe - Service Provider Strategies to Reduce Environmental Risks to Preconception, Prenatal & Child Health - Manual
- Health Canada - Our Health, Our Environment: A Snapshot of Environmental Health in Canada (PDF 3.91 MB)
Healthy Weight/Nutrition/Physical Activity
- Canadian Society for Exercise Physiology - Guidelines
- Health Canada - Canada's Food Guide: Canada's Dietary Guidelines
- Health Canada - Canadian Nutrient File
Indigenous Health
- Anishnawbe Health Toronto - Aboriginal Cultural Safety Initiative
- Best Start - Atuaqsijut: Following the Path Sharing Inuit Specific Ways
- Best Start - Open Hearts Open Minds
- Best Start - Pimotisiwin - A Good Path for Pregnant and Parenting Aboriginal Teens - Report
- Best Start - Supporting the Sacred Journey: From Preconception to Parenting for First Nations Families in Ontario
- Provincial Health Services Authority in British Columbia - Indigenous Cultural Safety Training
- Society of Obstetricians and Gynaecologists of Canada - Aboriginal Sexual Health
Intimate Partner Violence
- VEGA Project
- World Health Organization - Violence Info
- Best Start - Welcoming and Celebrating Sexual Orientation and Gender Diversity in Families, From Preconception to Preschool
- Gay and Lesbian Medical Association - Guidelines for Care of Lesbian, Gay, Bisexual and Transgender Patients
- The Joint Commission - Advancing Effective Communication, Cultural Competence, and Patient- and Family-Centered Care for the Lesbian, Gay, Bisexual, and Transgender (LGBT) Community: A Field Guide
Maternal and Newborn Assessment and Care
- Perinatal Services BC - Newborn & Postpartum Toolkit
- Rourke Baby Record
- The American College of Obstetricians and Gynecologists - ACOG Postpartum Toolkit (PDF 3.49 MB)
Medications
- Centers for Disease Control and Prevention - Treating for Two
- Health Canada - Drug Product Database
- Info-Médicaments en Allaitement et Grossesse
- Merck Manual - Professional Version
- MotherToBaby
Mental Health
- Best Start – Perinatal Mood Disorders: An Interdisciplinary Training Video
- Public Health Ontario - Perinatal Mental Health Toolkit
- Registered Nurses' Association of Ontario - Assessment and Interventions for Perinatal Depression
- Saskatchewan Prevention Institute – Resource Catalogue
Oral Health
- Saskatchewan Prevention Institute - Improving the Oral Health of Pregnant Women and Young Children
Substance Use
- Best Start – Prescription Opioid Use
- Perinatal Services BC & British Columbia Centre on Substance Use - Treatment of Opioid Use Disorder During Pregnancy: Guideline Supplement (PDF 467 KB)
- Portico - Primary Care Addiction Toolkit: Opioids misuse and addiction
- Saskatchewan Prevention Institute – Neonatal Abstinence Syndrome
- Best Start - Tobacco Misuse Resources
- CAN-ADAPTT- Guidelines and resources
- CAN-ADAPTT - Pregnets
- Canadian Public Health Association - Stop Smoking: A Smoking Cessation Resource for Those Who Work with Women
- Portico - Primary Care Addiction Toolkit: Smoking cessation
- Registered Nurses' Association of Ontario - Supporting Pre- and Postnatal Women and Their Families Who Use Tobacco
- Saskatchewan Prevention Institute - Environmental Tobacco Smoke: The risk to unborn babies, pregnant women and children
The Netherlands
The Netherlands has a system for postpartum care provided by kraamverzorgenden — maternity home care assistants. Trained caregivers visit the home of new parents and observe the mother and her baby, offer information in baby care and feeding, and even help in household chores, shopping, and if necessary, cooking. The service is popular and, because of a recent shortage of kraamverzorgenden , the average number of hours of maternity home care assistance over the first 8 days after normal childbirth has decreased from 64 to 44 hours. Footnote 326
As a result of guidelines developed by government, insurance companies, and professional organizations, maternity care in the Netherlands is considered “remarkable for its degree of cooperation between caregivers at different levels and locations in the system. Footnote 326 ” Pregnant women can move freely between care settings and caregivers, including midwives, general practitioners, and specialists.
Most babies are born in hospital in France. When families leave the hospital, they are given the telephone number of the nursery nurse in their area and are encouraged to call with any questions or concerns. Newborn babies are issued with a health record book that contains all their medical information—including vaccinations—up to age 16 years. The health record book is considered an essential document, and it aids the communication process between HCPs and families. Footnote 327
Compulsory medical examinations of children are carried out regularly. The first is within 8 days of birth, another is in month 9 or 10, and the last during month 24 or 25. Mothers and children can access interdisciplinary mother and baby care (“Protection maternelle et infantile”) at local maternal and child health clinics. Clinic staff conduct postnatal checks, provide nutritional and health advice, and can administer vaccinations. Footnote 327
Nova Scotia – Healthy Babies, Healthy Families: Postpartum & Postnatal Guidelines
The Government of Nova Scotia’s Healthy Babies, Healthy Families: Postpartum & Postnatal Guidelines provide guidance for the organization of postpartum services. These guidelines were developed to enhance and support the provision of high quality care to women, their babies, and their families across Nova Scotia in the first 6 weeks postpartum. They contain recommendations that focus on physiological stability, infant feeding or nutrition and growth monitoring, psychosocial/family adjustment, parent–child attachment/parenting, building on capacities and strengths, transition to home and community, family access to community support, healthy lifestyles and environments, collaborative practice, and professional competency. Footnote 328
Ontario – Standards of Postnatal Care
The Standards of Postnatal Care articulate the criteria of postnatal care for mothers and babies in Ontario in immediately postpartum. The Standards identify models, methods, or systems for improving coordination of care along with an evaluation framework to monitor their impact. To support the implementation of the Standards of Postnatal Care , another report was developed: Standards of Postnatal Care for Mothers and Newborns in Ontario (Part II): A focus on implementation and evaluation . This report provides an overview of implementation recommendations to enhance the delivery of postnatal care. It also includes a suggested evaluation framework that identifies priority standards for monitoring across the province. Footnote 42

Ontario – Monarch Centre – Ottawa
The Monarch Centre is a multidisciplinary maternal and newborn health clinic providing evidence-based comprehensive care. Following the birth and discharge from hospital, babies born at the Ottawa Hospital and their mothers can be referred to the Monarch Centre for their first 24- to 48-hour check-up. The registered nurses, board-certified lactation consultants, and family doctors at the Monarch Centre specialize in maternal and newborn care, and provide all the necessary breastfeeding support, bilirubin checks for jaundice, newborn screening and full postpartum check-ups, services and follow-up for mother and baby.
The Monarch Centre coordinates discharge directly with hospital providers to make sure that mother and baby are discharged when ready—and when it is medically appropriate. Upon coordinated discharge from hospital, Monarch supports the transition home for the new family. Footnote 329
British Columbia – The Nurse–Family Partnership
The Nurse–Family Partnership (NFP) is an intensive home-visiting program designed to help young first-time mothers and their children. A public health nurse visits women enrolled in the program throughout their pregnancy and until their child reaches 2 years of age. The goals are to improve children’s health and development while improving mothers’ life situations.
McMaster University in Ontario ran a pilot study of the NFP program, and British Columbia is conducting a randomized controlled trial evaluation. In the USA, the program has demonstrated improved parenting, reduced injuries and poisonings, and improved emotional and language development by babies. The mothers have also been found to have benefitted, with greater participation in the workforce and less reliance on social assistance. Footnote 330 Footnote 331
Drop-In Clinics: Usually staffed by nurses, midwives, and lactation consultants, postpartum clinics are geared to mother/baby drop-ins or scheduled visits. The clinic program can be structured for health assessment, health concerns, breastfeeding support, and advice.
Home Visits: A traditional follow-up component of maternal and newborn care is the home visit by either a nurse or midwife. The length and frequency of visits vary according to the needs of the family and the program specifications. Referrals for home visits are made by the hospital or community liaison staff or by the mother herself; often, they are governed by the “urgency” rating of the assessed need. In some areas, home visiting has been discontinued or replaced with community-based supports that the mother must transit to. Some hospitals have initiated home follow-up by their childbirth staff for mothers in need, as identified by risk criteria or need for additional support. Some home-visiting models use a combination of professional and paraprofessional visitors.
Online: Online resources for postpartum information include social media, websites, and blogs. Online resources enable mothers to engage with other mothers, share experiences, and attain information on caring for themselves and their newborn.
Parenting Courses: As with prenatal classes, some parents benefit from group or individual discussions on parenting during the postpartum period and learn more about their roles as parents through these.
Peer Support: Mother-to-mother support provided in various ways—in person, over the phone, via social media or texts. The supporter is or was in a similar situation to the peer. Some peer-to-peer support deals with specific topics such as breastfeeding or postpartum depression, while others provide general postpartum support.
Phone Lines: Some provinces and communities have initiated phone support and advice for new parents. Parents can ask questions, sometimes day or night, about personal, parenting, and postpartum health concerns. Questions usually relate to breastfeeding, crying, coping at home, and community resources. Phone lines can be connected to general health lines or hospital postpartum wards, or run by public health units or community-based organizations.
Physician/Midwife: Follow-up assessments by the physician, midwife, or other HCP in the community or home. Scheduling/timing of visits depends on general maternal and newborn health; complications of pregnancy, birth, and the postpartum period; and available family/community supports.
Telephone Follow-up: A phone call from public/community health nurses or midwives can ensure that the postpartum plan is in place and working well. Specific outcomes related to feeding and mother and baby well-being can be addressed. The telephone interview may result in a referral to a community agency for service, such as a home visit or other follow-up.
The Canada Prenatal Nutrition Program (CPNP) is a Government of Canada program that provides funding to community groups to help improve the health of pregnant women and new mothers and their babies who face, for example, poverty, teen pregnancy, social and geographical isolation, substance use, or family violence, which put their health at risk. CPNP aims to improve the health of women and their babies by increasing the number of babies born at a healthy weight and promoting and supporting breastfeeding. It ensures culturally sensitive prenatal support for Indigenous women and women who have recently immigrated. The program provides nutrition counselling, prenatal vitamins, food, food coupons and food preparation training, counselling in prenatal health and lifestyle, breastfeeding education and support, education and support on baby care and child development, and referrals to other agencies and services. Footnote 332
The Community Action Program for Children (CAPC) is another Government of Canada program that provides funding to community groups whose focus is the promotion of the healthy development of families (with children from birth to 6 years old) who face challenges that put their health at risk—poverty, teen parenting, social and geographical isolation, substance use, and family violence. The program aims to improve healthy child development by improving parenting skills and parent–child relationships; decreasing social isolation; increasing child self-esteem; and providing child-focused activities. Their programs may include nutritional support and collective kitchens; family resource centres; parenting classes and drop-in groups; child health and development activities; outreach and home-visiting programs; and specialized programs, such as support for mothers dealing with substance use. Footnote 333
The acronym LGBTQ 2 is commonly used to include people who identify their sexual orientation as lesbian, gay, bisexual, queer or questioning, and/or who identify their gender identity as transgender. These guidelines recognize that sexual orientation and gender identity exist along a continuum that may change over time, and that the LGBTQ 2 community is diverse. Footnote 334
Return to footnote * referrer
Perry SE, Hockenberry MJ, Lowdermilk DL, Wilson D, Keenan-Lindsay L, Sams CA. Maternal child nursing care in Canada. 2nd ed. Toronto (ON): Elsevier; 2017.
Return to footnote 1 referrer
Higginbottom GMA, Morgan M, Alexandre M, Chiu Y, Forgeron J, Kocay D, et al. Immigrant women's experiences of maternity-care services in Canada: a systematic review using a narrative synthesis. Syst Rev. 2015;4(13).
Return to footnote 2 referrer
Best Start Resource Centre. Giving birth in a new land: strategies for service providers working with newcomers [Internet]. Toronto (ON): Best Start Resource Centre; 2014 [cited 2020 June 22]. Available from: http://www.beststart.org/resources/rep_health/Newcomer_%20Guide_Final.pdf
Return to footnote 3 referrer
Reading CL, Wein F. Health inequalities and social determinants of Aboriginal peoples' health [Internet]. Prince George (BC): National Collaborating Centre for Aboriginal Health; 2009 [cited 2020 June 22]. Available from: https://www.ccnsa-nccah.ca/docs/determinants/RPT-HealthInequalities-Reading-Wien-EN.pdf
Return to footnote 4 referrer
Kolahdooz F, Launier K, Nader K, Yi KJ, Baker P, McHugh TL, et al. Canadian Indigenous women's perspectives of maternal health and health care services: A systematic review. Divers Equal Health Care. 2016;13(5):334-48.
Return to footnote 5 referrer
Best Start Resource Centre. Planning for change, facilitator guide: Workshop for First Nations women about FASD prevention and skills for change [Internet]. Toronto (ON): Best Start Resource Centre; 2019 [cited 2020 June 22]. Available from: https://resources.beststart.org/wp-content/uploads/2016/01/F19-A.pdf
Return to footnote 6 referrer
Wilson D, de la Ronde S, Brascoupé S, Apale AN, Barney L, Guthrie B, et al. Health professionals working with First Nations, Inuit, and Métis consensus guideline. SOGC clinical practice guideline no. 293. J Obstet Gynaecol Can. 2013;35(6 Suppl 2):S1-4.
Return to footnote 7 referrer
Perinatal Services BC. Doula services [Internet]. Vancouver (BC):PSBC; n.d. [cited 2019 Oct 19]. Available from: http://www.perinatalservicesbc.ca/health-professionals/professional-resources/indigenous-resources/doula-services
Return to footnote 8 referrer
Roy A, Thurston WE, Voices and PHACES Study Team. Depression and mental health in pregnant Aboriginal women: Key results and recommendations from the Voices and PHACES study. Final Report [Internet]. Calgary (AB): University of Calgary: 2015 [cited 2020 June 24]. Available from: https://www.ucalgary.ca/wethurston/files/wethurston/voices-phaces-study-finalreport.pdf
Return to footnote 9 referrer
Jumah NA, Wilson D, Shah R. A Canadian survey of postgraduate education in Aboriginal women's health in obstetrics and gynaecology. J Obstet Gynaecol Can. 2013;35(7):647-53.
Return to footnote 10 referrer
Best Start Resource Centre. Welcoming and celebrating sexual orientation and gender diversity in families [Internet]. Toronto (ON): Best Start Resource Centre; 2013 [cited 2020 June 24]. Available from: https://resources.beststart.org/product/j14e-sexual-orientation-gender-diversity-families-manual/
Return to footnote 11 referrer
Hayman B, Wilkes L, Halcomb EJ, Jackson D. Marginalised mothers: Lesbian women negotiating heteronormative healthcare services. Contemp Nurse. 2013;44(1):120-7.
Return to footnote 12 referrer
Gregg I. The health care experiences of lesbian women becoming mothers. Nurs Womens Health. 2018;22(1):40-50.
Return to footnote 13 referrer
Ross LE. Perinatal mental health in lesbian mothers: A review of potential risk and protective factors. Women Health. 2005;41(3):113-28.
Return to footnote 14 referrer
Maccio EM, PhD, Pangburn JA, MSW. The case for investigating postpartum depression in lesbians and bisexual women. Womens Health Issues. 2011;21(3):187-90.
Return to footnote 15 referrer
Ross LE, Steele L, Goldfinger C, Strike C. Perinatal depressive symptomatology among lesbian and bisexual women. Arch Womens Ment Health. 2007;10(2):53-9.
Return to footnote 16 referrer
Queering Parenthood. Postpartum wellbeing study [Internet]. Toronto (ON): University of Toronto; 2007 [cited 2020 June 23]. Available from: http://queeringparenthood.com/postpartumwellbeingstudy.php
Return to footnote 17 referrer
Renaud MT. We are mothers too: childbearing experiences of lesbian families. J Obstet Gynecol Neonatal Nurs. 2007;36(2):190-9.
Return to footnote 18 referrer
Zero to Three. Laying the foundation for early development: Infant and early childhood mental health [Internet]. Washington (DC): Zero to Three; 2009 [cited 2020 June 24]. Available from:https://www.zerotothree.org/resources/443-laying-the-foundation-for-early-development-infant-and-early-childhood-mental-health
Return to footnote 19 referrer
World Health Organization, UNICEF. Implementation guidance: protecting, promoting, and supporting breastfeeding in facilities providing maternity and newborn services: the revised Baby-friendly Hospital Initiative 2018 [Internet]. Geneva (CH): WHO; 2018 [cited 2020 July 3]. Available from: http://apps.who.int/iris/bitstream/handle/10665/272943/9789241513807-eng.pdf?ua=1
Return to footnote 20 referrer
Harrison D. Newborn pain reduction: Evidence based strategies [Internet]. Ottawa (ON): Champlain Maternal Newborn Regional Program; 2017 [cited 2020 July 3]. Available from: http://www.cmnrp.ca/uploads/documents//KT_Strategy__Newborn_Pain_Management_FINAL_revised_2017_12.pdf
Return to footnote 21 referrer
Moore ER, Bergman N, Anderson GC, Medley N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst Rev. 2016(11):CD003519.
Return to footnote 22 referrer
Provincial Council for Maternal and Child Health. Final report: Maternal-Newborn Advisory Committee, Mother Baby Dyad Work Group [Internet]. Toronto (ON): PCMCH; 2011 [cited 2020 July 3]. Available from: https://www.pcmch.on.ca/wp-content/uploads/2015/07/MBDC_Report_2011FEB06.pdf
Return to footnote 23 referrer
National Institute for Health and Care Excellence. Postnatal care up to 8 weeks after birth [Internet]. London (UK): NICE; 2006 [cited 2020 July 3]. Available from: https://www.nice.org.uk/guidance/cg37
Return to footnote 24 referrer
Dumas L, Widström A. Skin2Skin infographic FAQ's for health care providers [Internet]. Ottawa (ON): Leeds, Grenville & Lanark District Health Unit; 2015 [cited 2020 July 3]. Available from: http://www.bfiontario.ca/wp-content/uploads/2012/10/Skin-to-skin-Infographic-FAQ-Leeds-Grenville-Lanark-District-Health-Unit.pdf
Return to footnote 25 referrer
Winberg J. Mother and newborn baby: Mutual regulation of physiology and behavior - A selective review. Dev Psychobiol. 2005;47(3):217-29.
Return to footnote 26 referrer
Örtenstrand A, Westrup B, Brostrom EB, Sarman I, Akerstrom S, Brune T, et al. The Stockholm neonatal family centered care study: Effects on length of stay and infant morbidity. Pediatrics. 2010;125(2):e278-85.
Return to footnote 27 referrer
Jefferies AL, Canadian Paediatric Society, Fetus and Newborn Committee. Kangaroo care for the preterm infant and family. Paediatr Child Health. 2012;17(3):141-3.
Return to footnote 28 referrer
Chalmers B. Family-centred perinatal care: improving pregnancy, birth and postpartum care. Cambridge (UK): Cambridge University Press; 2017.
Return to footnote 29 referrer
O'Brien K, Bracht M, Macdonell K, McBride T, Robson K, O'Leary L, et al. A pilot cohort analytic study of family integrated care in a Canadian neonatal intensive care unit. BMC Pregnancy Childbirth. 2013;13(Suppl 1):S12.
Return to footnote 30 referrer
Hung KJ, Berg O. Early skin-to-skin: after cesarean to improve breastfeeding. MCN Am J Matern Child Nurs. 2011;36(5):318-24.
Return to footnote 31 referrer
Phillips C. Family-centered maternity care. 4th ed. St. Louis (MO): Mosby; 2003.
Return to footnote 32 referrer
Carroli G, Cuesta C, Abalos E, Gulmezoglu AM. Epidemiology of postpartum haemorrhage: A systematic review. Best Pract Res Clin Obstet Gynaecol. 2008;22(6):999-1012.
Return to footnote 33 referrer
Public Health Agency of Canada. Perinatal health indicators for Canada 2013. Ottawa (ON): PHAC; 2013.
Return to footnote 34 referrer
Leduc D, Senikas V, Lalonde AB, Ballerman C, Biringer A, Delaney M, et al. Active management of the third stage of labour: prevention and treatment of postpartum hemorrhage. SOGC clinical practice guideline no. 235. J Obstet Gynaecol Can. 2009;31(10):980-93.
Return to footnote 35 referrer
Anderson JM, Etches D. Prevention and management of postpartum hemorrhage. Am Fam Physician. 2007;75(6):875-82.
Return to footnote 36 referrer
Evensen A, Anderson JM, Fontaine, P. Postpartum hemorrhage: Prevention and treatment. Am Fam Physician. 2017;95(7):442-9.
Return to footnote 37 referrer
Weiner, G. Textbook of Neonatal Resuscitation. 7th ed. Evanston (IL): American Academy of Pediatrics; 2016.
Return to footnote 38 referrer
Canadian Paediatric Society. Neonatal resuscitation program [Internet]. Ottawa (ON): CPS; 2016 [cited 2020 July 6]. Available from: https://www.cps.ca/en/nrp-prn
Return to footnote 39 referrer
Perinatal Services BC. Provincial perinatal guidelines: Standards for neonatal resuscitation [Internet]. Vancouver (BC): PSBC; 2017 [cited 2020 July 3]. Available from: http://www.perinatalservicesbc.ca/Documents/Guidelines-Standards/Newborn/NeonatalResuscitationGuideline.pdf
Return to footnote 40 referrer
Perinatal Services BC. Obstetrics guideline 20: Postpartum nursing care pathway [Internet]. Vancouver (BC): PSBC; 2011 [cited 2020 July 3]. Available from: http://www.perinatalservicesbc.ca/Documents/Guidelines-Standards/Maternal/PostpartumNursingCarePathway.pdf
Return to footnote 41 referrer
Provincial Council for Maternal and Child Health. Standards of postnatal care for mothers and newborns in Ontario: A focus on implementation and evaluation [Internet]. Toronto (ON): PCMCH; 2018 [cited 2020 July 3]. Available from: https://www.pcmch.on.ca/wp-content/uploads/2018/05/Standards-of-Postnatal-Care-for-Mothers-and-Newborns-in-Ontario-Final-Report-Part-II-2018May16.pdf
Return to footnote 42 referrer
Provincial Council for Maternal and Child Health. Standards of postnatal care for mothers and newborns in Ontario: Birth to one-week postnatal period [Internet]. Toronto (ON): PCMCH; 2018 [cited 2020 July 3]. Available from: https://www.pcmch.on.ca/wp-content/uploads/2018/05/Standards-of-Postnatal-Care-for-Mothers-and-Newborns-in-Ontario-Final-Report-Part-I-2018May16.pdf
Return to footnote 43 referrer
Breastfeeding Committee of Canada. The BFI 10 steps and WHO code outcome indicators for hospital and community health services [Internet]. Drayton Valley (AB): BCC; 2017 [cited 2020 Jul 3]. Available from: http://breastfeedingcanada.ca/documents/Indicators%20-%20complete%20June%202017.pdf
Return to footnote 44 referrer
Lemyre B, Jefferies AL, O'Flaherty P, Canadian Paediatric Society: Fetus and Newborn Committee. Facilitating discharge from hospital of the healthy term infant. Paediatr Child Health. 2018;23(8):515-22.
Return to footnote 45 referrer
Benitz WE, Watterberg KL, Aucott S, Cummings JJ, Eichenwald EC, Goldsmith J, et al. Hospital stay for healthy term newborn infants. Pediatrics. 2015;135(5):948-53.
Return to footnote 46 referrer
Canadian Institute for Health Information. CIHI snapshot: Inpatient hospitalization, surgery, newborn, alternate level of care and childbirth statistics, 2017–2018 [Internet]. Ottawa (ON): CIHI; 2019 [cited 2020 July 3]. Available from: https://www.cihi.ca/sites/default/files/document/dad-hmdb-childbirth-quick-stats-2017-2018-snapshot-en-web.pdf
Return to footnote 47 referrer
Benahmed N, San Miguel L, Devos C, Fairon N, Christiaens W. Vaginal delivery: how does early hospital discharge affect mother and child outcomes? A systematic literature review. BMC Pregnancy Childbirth. 2017;17(1):289.
Return to footnote 48 referrer
Brown S, Small R, Faber B, Krastev A, Davis P. Early postnatal discharge from hospital for healthy mothers and term infants. Cochrane Database Syst Rev. 2002(3):CD002958.
Return to footnote 49 referrer
Canadian Medical Protective Association. Safe care in obstetrics – Maternal postpartum care: When things don't go as planned after delivery [Internet]. Ottawa (ON): CMPA; 2017 [cited 2020 July 3]. Available from: https://www.cmpa-acpm.ca/en/advice-publications/browse-articles/2017/safe-care-in-obstetrics-maternal-postpartum-care-when-things-don-t-go-as-planned-after-delivery
Return to footnote 50 referrer
Association of Women's Health, Obstetric and Neonatal Nurses. Mood and anxiety disorders in pregnant and postpartum women. J Obstet Gynecol Neonatal Nurs. 2015;44(5):687-9.
Return to footnote 51 referrer
Joffres M, Jaramillo A, Dickinson J, Lewin G, Pottie K, Shaw E, et al. Recommendations on screening for depression in adults. CMAJ. 2013;185(9):775-82.
Return to footnote 52 referrer
Registered Nurses Association of Ontario. Assessment and interventions for perinatal depression [Internet]. Toronto (ON): RNAO; 2018 [cited 2020 July 3]. Available from: https://rnao.ca/bpg/guidelines/assessment-and-interventions-perinatal-depression
Return to footnote 53 referrer
BC Reproductive Mental Health Program, Perinatal Services BC. Best practice guidelines for mental health disorders in the perinatal period [Internet]. Vancouver (BC): PSBC; 2014 [cited 2020 July 3]. Available from: http://www.perinatalservicesbc.ca/Documents/Guidelines-Standards/Maternal/MentalHealthDisordersGuideline.pdf
Return to footnote 54 referrer
Siu AL, Bibbins-Domingo K, Grossman DC, Baumann LC, Davidson KW, Ebell M, et al. Screening for depression in adults: US Preventive Services Task Force recommendation statement. JAMA. 2016;315(4):380-7.
Return to footnote 55 referrer
Canadian Institute of Health Information. Inpatient hospitalizations, surgeries and newborn indicators, 2016–2017 [Internet]. Ottawa (ON): CIHI; 2018 [cited 2020 July 3]. Available from: https://www.cihi.ca/sites/default/files/document/hospchild-inpatientalosdiagsurg-2016-2017-en.xlsx
Return to footnote 56 referrer
Canadian Institute of Health Information. Quick stats: Childbirth indicators by place of residence [Internet]. Ottawa (ON): CIHI; 2018 [cited 2020 July 3]. Available from: https://apps.cihi.ca/mstrapp/asp/Main.aspx?Server=apmstrextprd_i&project=Quick%20Stats&uid=pce_pub_en&pwd=&evt=2048001&visualizationMode=0&documentID=029DB170438205AEBCC75B8673CCE822
Return to footnote 57 referrer
Chalmers BE, Dzakpasu S. Interventions in labour and birth and satisfaction with care: The Canadian maternity experiences survey findings. J Reprod Infant Psychol. 2015;33(4):374-87.
Return to footnote 58 referrer
Borders N. After the afterbirth: A critical review of postpartum health relative to method of delivery. J Midwifery Womens Health. 2006;51(4):242-8.
Return to footnote 59 referrer
American College of Obstetricians and Gynecologists. ACOG committee opinion umber 736: Optimizing postpartum care. Obstet Gynecol. 2018;131(5):e140-50.
Return to footnote 60 referrer
Kramer M, Aboud F, Mironova E, Vanilovich I, Platt R, Matush L, et al. Breastfeeding and child cognitive development: new evidence from a large randomized trial. Arch Gen Psychiatry. 2008;65(5):578-84.
Return to footnote 61 referrer
Quigley M, Hockley C, Carson C, Kelly Y, Renfrew M, Sacker A. Breastfeeding is associated with improved child cognitive development: a population-based cohort study. J Pediatr. 2012;160(1):25-32.
Return to footnote 62 referrer
Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, et al. Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess. 2007(153):1-186.
Return to footnote 63 referrer
Arenz S, Rückerl R, Koletzko B, Von Kries R. Breast-feeding and childhood obesity-a systematic review. Int J Obes. 2004;28(10):1247-56.
Return to footnote 64 referrer
Hauck F, Thompson J, Tanabe K, Moon R, Vennemann M. Breastfeeding and reduced risk of sudden infant death syndrome: A meta-analysis. Pediatrics. 2011;128(1):103-110.
Return to footnote 65 referrer
Health Canada, Canadian Paediatric Society, Dietitians of Canada, Breastfeeding Committee for Canada. Nutrition for healthy term infants: recommendations from birth to six months [Internet]. Ottawa (ON): HC; 2012 [cited 2020 July 16]. Available from: https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-eating/infant-feeding/nutrition-healthy-term-infants-recommendations-birth-six-months.html
Return to footnote 66 referrer
Zero to Three. The basics of infant and early childhood mental health: A briefing paper [Internet]. Washington (DC): Zero to Three; 2017 [cited 2020 July 3]. Available from: https://www.zerotothree.org/resources/1951-the-basics-of-infant-and-early-childhood-mental-health-a-briefing-paper
Return to footnote 67 referrer
Centers for Disease Control and Prevention. Early brain development and health [Internet]. Atlanta (GA): CDC; 2019 [cited 2020 July 6]. Available from: https://www.cdc.gov/ncbddd/childdevelopment/early-brain-development.html
Return to footnote 68 referrer
Center on the Developing Child. The foundations of lifelong health are built in early childhood [Internet]. Cambridge (MA): Harvard University; 2010 [cited 2020 July 16]. Available from: https://developingchild.harvard.edu/wp-content/uploads/2010/05/Foundations-of-Lifelong-Health.pdf
Return to footnote 69 referrer
National Scientific Council on the Developing Child. Children's emotional development is built into the architecture of their brains: working paper 2 [Internet]. Cambridge (MA): Harvard University; 2004 [cited 2020 July 16]. Available from: https://46y5eh11fhgw3ve3ytpwxt9r-wpengine.netdna-ssl.com/wp-content/uploads/2004/04/Childrens-Emotional-Development-Is-Built-into-the-Architecture-of-Their-Brains.pdf
Return to footnote 70 referrer
van IJzendoorn, M. Attachment at an early age (0-5) and its impact on children's development [Internet]. Rotterdam (NL): Encyclopedia on Early Childhood Development; 2019 [cited 2020 July 16]. Available from: http://www.child-encyclopedia.com/sites/default/files/textes-experts/en/567/attachment-at-an-early-age-0-5-and-its-impact-on-childrens-development.pdf
Return to footnote 71 referrer
Saskatchewan Prevention Institute. Infant and early childhood mental health [Internet]. Saskatoon (SK): SPI; 2011 [cited 2020 July 16]. Available from: https://skprevention.ca/resource-catalogue/child-development/infant-and-early-childhood-mental-health/
Return to footnote 72 referrer
Gunnar MR, Herrera A, Hostinar CE. Stress and early brain development [Internet]. Minneapolis (MN): Encyclopedia on Early Childhood Development; 2009 [cited 2020 July 16]. Available from: http://www.child-encyclopedia.com/sites/default/files/textes-experts/en/580/stress-and-early-brain-development.pdf
Return to footnote 73 referrer
Brown Belfort M. The science of breastfeeding and brain development. Breastfeed Med. 2017;12(8):459-61.
Return to footnote 74 referrer
Krol KM, Grossmann T. Psychological effects of breastfeeding on children and mothers. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2018;61(8):977-85.
Return to footnote 75 referrer
National Collaborating Centre for Determinants of Health. Foundations: definitions and concepts to frame population mental health promotion for children and youth [Internet]. Antigonish (NS): National Collaborating Centres for Public Health; 2017 [cited 2020 July 16]. Available from: http://nccph.ca/images/uploads/general/02_Foundations_MentalHealth_NCCPH_2017_EN.pdf?utm_source=newsletter&utm_medium=email&utm_campaign=PMH_02_En
Return to footnote 76 referrer
Public Health Agency of Canada. Nobody's perfect [Internet]. Ottawa (ON): PHAC; 2019 [cited 2020 July 16]. Available from: https://www.canada.ca/en/public-health/services/health-promotion/childhood-adolescence/parent/nobody-perfect.html
Return to footnote 77 referrer
Canadian Paediatric Society. Relationships matter: How clinicians can support positive parenting in the early years [Internet]. Ottawa (ON): CPS; 2019 [cited 2020 July 16]. Available from: https://www.cps.ca/en/documents/position/positive-parenting
Return to footnote 78 referrer
Infant Mental Health Promotion. Best practice guidelines: Competencies for practice in the field of infant mental health [Internet]. Toronto (ON): IMHP; 2011 [cited 2020 July 16]. Available from: https://www.imhpromotion.ca/Resources/Best-Practice-Guidelines/Competencies.aspx
Return to footnote 79 referrer
Best Start Resource Centre. Healthy baby healthy brain [Internet]. Toronto (ON): Best Start Resource Centre; 2019 [cited 2020 July 16]. Available from: https://resources.beststart.org/product/k34e-healthy-baby-healthy-brain-workshop/
Return to footnote 80 referrer
Moore DL, MacDonald NE, Canadian Paediatric Society, Infectious Diseases and Immunization Committee. Preventing ophthalmia neonatorum. Paediatr Child Health. 2015;20(2):93-6.
Return to footnote 81 referrer
Public Health Agency of Canada. Section 5-6: Canadian guidelines on sexually transmitted infections – Management and treatment of specific infections – Gonococcal infections. Table 13: ophthalmia neonatorum [Internet]. Ottawa (ON): PHAC; 2013 [cited 2020 July 23]. Available from: https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/canadian-guidelines/sexually-transmitted-infections/canadian-guidelines-sexually-transmitted-infections-34.html#toc361210477
Return to footnote 82 referrer
Association of Women's Health, Obstetric and Neonatal Nurses. Neonatal skin care. 3rd ed. Washington (DC): 2013.
Return to footnote 83 referrer
Canadian Paediatric Society. Your baby's skin [Internet]. Ottawa (ON): CPS; 2017 [cited 2020 July 24]. Available from: https://www.caringforkids.cps.ca/handouts/your-babys-skin
Return to footnote 84 referrer
American Academy of Pediatrics, American College of Obstetricians & Gynecologists. Guidelines for perinatal care. 7 th ed. Washington, DC: 2013.
Return to footnote 85 referrer
Sorokan ST, Finlay JC, Jefferies AL, Canadian Paediatric Society. Newborn male circumcision. Paediatr Child Health. 2015;20(6):311-5.
Return to footnote 86 referrer
American Academy of Pediatrics, Task Force on Circumcision. Circumcision policy statement. Pediatrics. 2012;130(3):585-6.
Return to footnote 87 referrer
Foddy B. Medical, religious and social reasons for and against an ancient rite. J Med Ethics. 2013;39(7):415.
Return to footnote 88 referrer
Public Health Agency of Canada. Recommended immunization schedules: Canadian immunization guide [Internet]. Ottawa (ON): PHAC; 2020 [cited 2020 July 24]. Available from: https://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-part-1-key-immunization-information/page-13-recommended-immunization-schedules.html#p1c12a2
Return to footnote 89 referrer
Ward LM, Gaboury I, Ladhani M, Zlotkin S. Vitamin D-deficiency rickets among children in Canada. CMAJ. 2007;177(2):161-6.
Return to footnote 90 referrer
Butte N, Lopez-Alarcon MG, Garza C. Nutrient adequacy of exclusive breastfeeding for the term infant during the first six months of life [Internet]. Geneva (CH): WHO; 2002 [cited 2020 July 24]. Available from: https://apps.who.int/iris/handle/10665/42519
Return to footnote 91 referrer
Salle BL, Delvin EE, Lapillonne A, Bishop NJ, Glorieux FH. Perinatal metabolism of vitamin D. Am J Clin Nutr. 2000;71(5):1317-24S.
Return to footnote 92 referrer
Health Canada, Canadian Paediatric Society, Dietitians of Canada, Breastfeeding Committee for Canada. Nutrition for healthy term infants: recommendations from six to 24 months [Internet]. Ottawa (ON): HC; 2014 [cited 2020 July 24]. Available from: https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-eating/infant-feeding/nutrition-healthy-term-infants-recommendations-birth-six-months/6-24-months.html
Return to footnote 93 referrer
Godel JC, Canadian Paediatric Society, First Nations,Inuit and Métis Health Committee. Vitamin D supplementation: recommendations for Canadian mothers and infants. Paediatr Child Health. 2007;12(7):583-9.
Return to footnote 94 referrer
Adamkin DH. Metabolic screening and postnatal glucose homeostasis in the newborn. Pediatr Clin North Am. 2015;62(2):385-409.
Return to footnote 95 referrer
Canadian Organization for Rare Disorders. Newborn screening in Canada status report [Internet]. Toronto (ON): CORD; 2015 [cited 2020 July 24]. Available from: https://www.raredisorders.ca/content/uploads/Canada-NBS-status-updated-Sept.-3-2015.pdf
Return to footnote 96 referrer
Barrington K, Sankaran K, Canadian Paediatric Society, Fetus and Newborn Committee. Guidelines for detection, management and prevention of hyperbilirubinemia in term and late preterm newborn infants. Paediatr Child Health. 2007;12(Suppl B):1-12B.
Return to footnote 97 referrer
Newborn Screening Ontario. Critical congenital heart disease (CCHD) [Internet]. Ottawa (ON): NSO; 2020 [cited 2020 July 24]. Available from: https://www.newbornscreening.on.ca/en/disease/critical-congenital-heart-disease-cchd
Return to footnote 98 referrer
Newborn Screening Ontario. Critical congenital heart disease pulse oximetry screening protocol [Internet]. Ottawa (ON): NSO; 2018 [cited 2020 July 24]. Available from: https://www.newbornscreening.on.ca/sites/default/files/nso_cchd_protocol_v1.1.pdf
Return to footnote 99 referrer
Narvey M, Wong KK, Fournier A, Canadian Paediatric Society, Fetus and Newborn Committee. Pulse oximetry screening in newborns to enhance detection of critical congenital heart disease. Paediatr Child Health. 2017;22(8):494-8.
Return to footnote 100 referrer
Bagatto M, Scollie SD, Hyde M, Seewald R. Protocol for the provision of amplification within the Ontario infant hearing program. Int J Audiol. 2010;49(1):S70-9.
Return to footnote 101 referrer
Patel H, Feldman M. Universal newborn hearing screening. Paediatr Child Health. 2011;16(5):301-5.
Return to footnote 102 referrer
Eskander A, Papsin BC. Screening infants for hearing impairment in Canada. CMAJ. 2014;186(14):1048-9.
Return to footnote 103 referrer
Speech-Language and Audiology Canada. SAC position paper on universal newborn hearing screening in Canada [Internet]. Ottawa (ON): SAC; 2014 [cited 2020 July 24]. Available from: https://www.sac-oac.ca/sites/default/files/resources/SAC-OAC-UNHS-PP_EN.pdf
Return to footnote 104 referrer
Ottawa Neonatal Pain Interest Group. Newborn pain management: A practical approach. Self-learning module [Internet]. Ottawa (ON): Champlain Maternal Newborn Regional Program; 2015 [cited 2020 July 24]. Available from: http://www.cmnrp.ca/uploads/documents//Newborn_Pain_SLM_2015_02_19_FINAL.pdf
Return to footnote 105 referrer
Shah PS, Herbozo C, Aliwalas LL, Shah VS. Breastfeeding or breast milk for procedural pain in neonates. Cochrane Database Syst Rev. 2012;12:CD004950.
Return to footnote 106 referrer
Johnston C, Campbell-Yeo M, Disher T, Benoit B, Fernandes A, Streiner D, et al. Skin-to-skin care for procedural pain in neonates. Cochrane Database Syst Rev 2017;2017(2):CD008435.
Return to footnote 107 referrer
Harrison D, Bueno M, Yamada J, Adams-Webber T, Stevens B. Analgesic effects of sweet-tasting solutions for infants: Current state of equipoise. Pediatrics. 2010;126(5):894-902.
Return to footnote 108 referrer
Barrington KJ, Batto DG, Finley GA, Wallman C, Canadian Paediatric Society, Fetus and Newborn Committee. Prevention and management of pain in the neonate: An update. Paediatr Child Health. 2007;12(2):137-8.
Return to footnote 109 referrer
Leduc D, Côté A, Woods S, Canadian Paediatric Society. Recommendations for safe sleeping environments for infants and children. Paediatr Child Health. 2004;9(9):659-63.
Return to footnote 110 referrer
Public Health Agency of Canada, Canadian Paediatric Society, Canadian Foundation for the Study of Infant Deaths, Canadian Institutes of Child Health, Health Canada. Joint statement on safe sleep: Preventing sudden infant deaths in Canada [Internet]. Ottawa (ON): PHAC; 2011 [cited 2020 July 24]. Available from: https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/hp-ps/dca-dea/stages-etapes/childhood-enfance_0-2/sids/pdf/jsss-ecss2011-eng.pdf
Return to footnote 111 referrer
Statistics Canada. Table: 13-10-0395-01 Leading causes of death, infants [Internet]. Ottawa (ON): SC; 2018 [cited 2020 July 24]. Available from: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310039501
Return to footnote 112 referrer
American Academy of Pediatrics, Task Force on Sudden Infant Death Syndrome. SIDS and other sleep-related infant deaths: Updated 2016 recommendations for a safe infant sleeping environment. Pediatrics. 2016;138(5):e20162938.
Return to footnote 113 referrer
Perinatal Services BC. Health promotion guideline 1: Safe sleep environment guidelines for infants 0 to 12 months [Internet]. Vancouver (BC): Perinatal Services BC; 2011 [cited 2020 July 24]. Available from: http://www.perinatalservicesbc.ca/Documents/Guidelines-Standards/HealthPromotion/SafeSleepGuideline.pdf
Return to footnote 114 referrer
Registered Nurses' Association of Ontario. Working with families to promote safe sleep for infants 0-12 months of age [Internet]. Toronto (ON): RNAO; 2014 [cited 2020 July 24]. Available from: https://rnao.ca/bpg/guidelines/safe-sleep-practices-infants
Return to footnote 115 referrer
Bloem M. The 2006 WHO child growth standards. BMJ. 2007;334(7596):705-6.
Return to footnote 116 referrer
Wambach K, Riordan J. Breastfeeding and human lactation. 5th ed. Burlington (MA): Jones & Bartlett Learning; 2016.
Return to footnote 117 referrer
World Health Organization. Weight velocity [Internet]. Geneva (CH): WHO; 2011 [cited 2020 July 24]. Available from: https://www.who.int/childgrowth/standards/w_velocity/en/
Return to footnote 118 referrer
Canadian Paediatric Society. About ACoRN [Internet]. Ottawa (ON): CPS; 2019 [cited 2020 July 24]. Available from: https://www.cps.ca/en/acorn
Return to footnote 119 referrer
Stein A, Pearson RM, Goodman SH, Rapa DPhil E, Rahman A, McCallum M, et al. Effects of perinatal mental disorders on the fetus and child. Lancet. 2014;384(9956):1800-19.
Return to footnote 120 referrer
National Institute for Health and Care Excellence. Antenatal and postnatal mental health: clinical management and service guidance [Internet]. London (UK): NICE; 2014 [cited 2020 Jul 24]. Available from: https://www.nice.org.uk/guidance/cg192
Return to footnote 121 referrer
Henshaw C. Mood disturbance in the early puerperium: a review. Arch Womens Ment Health. 2003;6(S2):s33-42.
Return to footnote 122 referrer
Edhborg M. Comparisons of different instruments to measure blues and to predict depressive symptoms 2 months postpartum: a study of new mothers and fathers. Scand J Caring Sci. 2008;22(2):186-95.
Return to footnote 123 referrer
Watanabe M, Wada K, Sakata Y, Aratake Y, Kato N, Ohta H, et al. Maternity blues as predictor of postpartum depression: A prospective cohort study among Japanese women. J Psychosom Obstet Gynaecol. 2008;29(3):206-12.
Return to footnote 124 referrer
Reck C, Stehle E, Reinig K, Mundt C. Maternity blues as a predictor of DSM-IV depression and anxiety disorders in the first three months postpartum. J Affect Disord. 2009;113(1):77-87.
Return to footnote 125 referrer
Doornbos B, Fekkes D, Tanke MAC, de Jonge P, Korf J. Sequential serotonin and noradrenalin associated processes involved in postpartum blues. Prog Neuro-Psychopharmacol Biol Psychiatry. 2008;32(5):1320-5.
Return to footnote 126 referrer
O'Keane V, Lightman S, Patrick K, Marsh M, Papadopoulos AS, Pawlby S, et al. Changes in the maternal hypothalamic-pituitary-adrenal axis during the early puerperium may be related to the postpartum 'blues'. J Neuroendocrinol. 2011;23(11):1149-55.
Return to footnote 127 referrer
M'baïlara K, Swendsen J, Glatigny-Dallay E, Dallay D, Roux D, Sutter AL, et al. Baby blues: characterization and influence of psycho-social factors. Encéphale. 2005;31(3):331.
Return to footnote 128 referrer
March of Dimes. Baby blues after pregnancy [Internet]. Arlington (VA): March of Dimes; 2017 [cited 2020 July 24]. Available from: https://www.marchofdimes.org/pregnancy/baby-blues-after-pregnancy.aspx
Return to footnote 129 referrer
Sacher J, Wilson AA, Houle S, Rusjan P, Hassan S, Bloomfield PM, et al. Elevated brain monoamine oxidase a binding in the early postpartum period. Arch Gen Psychiatry. 2010;67(5):468-74.
Return to footnote 130 referrer
Sanjuan J, Martin-Santos R, Garcia-Esteve L, Carot JM, Guillamat R, Gutierrez-Zotes A, et al. Mood changes after delivery: role of the serotonin transporter gene. Br J Psychiatry. 2008;193(5):383-8.
Return to footnote 131 referrer
Seyfried LS, Marcus SM. Postpartum mood disorders. Int Rev Psychiatry. 2003;15(3):231-42.
Return to footnote 132 referrer
Henshaw C, Foreman D, Cox J. Postnatal blues: A risk factor for postnatal depression. J Psychosom Obstet Gynaecol. 2004;25(3-4):267-72.
Return to footnote 133 referrer
Howard LM, Molyneaux E, Dennis C, Rochat T, Stein A, Milgrom J. Non-psychotic mental disorders in the perinatal period. Lancet. 2014;384(9956):1775-88.
Return to footnote 134 referrer
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5 th ed. Washington (DC): 2013.
Return to footnote 135 referrer
Austin M. Classification of mental health disorders in the perinatal period: future directions for DSM-V and ICD-11. Arch Womens Ment Health. 2010;13(1):41-4.
Return to footnote 136 referrer
Jones I, Cantwell R. The classification of perinatal mood disorders—suggestions for DSMV and ICD11. Arch Womens Ment Health. 2010;13(1):33-6.
Return to footnote 137 referrer
Wisner KL, Wisner KL, Moses-Kolko EL, Moses-Kolko EL, Sit DKY, Sit DKY. Postpartum depression: a disorder in search of a definition. Arch Womens Ment Health. 2010;13(1):37-40.
Return to footnote 138 referrer
Statistics Canada. Maternal mental health in Canada, 2018/2019. [Internet]. Ottawa (ON): SC; 2019 [cited 2020 July 24]. Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/190624/dq190624b-eng.htm
Return to footnote 139 referrer
Sharma V, Mazmanian D. Sleep loss and postpartum psychosis. Bipolar Disord. 2003;5(2):98-105.
Return to footnote 140 referrer
Daoud N, O'Brien K, O'Campo P, Harney S, Harney E, Bebee K, et al. Postpartum depression prevalence and risk factors among Indigenous, non-Indigenous and immigrant women in Canada. Can J Public Health. 2019;110(4):440-52.
Return to footnote 141 referrer
Black KA, MacDonald I, Chambers T, Ospina MB. Postpartum mental health disorders in Indigenous women: A systematic review and meta-analysis. J Obstet Gynaecol Can. 2019;41(10):1470-78.
Return to footnote 142 referrer
Wisner KL, Sit DKY, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry. 2013;70(5):490-8.
Return to footnote 143 referrer
Cox J, Holden J, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. 1987;150(6):782-6.
Return to footnote 144 referrer
Eberhard-Gran M, Eskild A, Tambs K, Opjordsmoen S, Ove Samuelsen S. Review of validation studies of the Edinburgh Postnatal Depression Scale. Acta Psychiatr Scand. 2001;104(4):243-9.
Return to footnote 145 referrer
Brouwers EPM, van Baar AL, Pop VJM. Does the Edinburgh postnatal depression scale measure anxiety? J Psychosom Res. 2001;51(5):659-63.
Return to footnote 146 referrer
Matthey S, Barnett B, Howie P, Kavanagh DJ. Diagnosing postpartum depression in mothers and fathers: whatever happened to anxiety? J Affect Disord. 2003;74(2):139-47.
Return to footnote 147 referrer
Figueiredo B, Conde A. Anxiety and depression in women and men from early pregnancy to 3-months postpartum. Arch Womens Ment Health. 2011;14(3):247-55.
Return to footnote 148 referrer
Dennis C, Coghlan M, Vigod S. Can we identify mothers at-risk for postpartum anxiety in the immediate postpartum period using the State-Trait Anxiety Inventory? J Affect Disord. 2013;150(3):1217-20.
Return to footnote 149 referrer
Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. 2016;39:24-31.
Return to footnote 150 referrer
eMentalHealth.ca. Screening tool: anxiety disorders (2-question screener [GAD-2]) [Internet]. Ottawa (ON): eMentalHealth.ca; 2019 [cited 2020 July 24]. Available from: https://www.ementalhealth.ca/index.php?m=survey&ID=44
Return to footnote 151 referrer
Ross LE, McLean LM. Anxiety disorders during pregnancy and the postpartum period: A systematic review. J Clin Psychiatry. 2006;67(8):1285-98.
Return to footnote 152 referrer
Weisberg RB, Paquette JA. Screening and treatment of anxiety disorders in pregnant and lactating women. Womens Health Issues. 2002;12(1):32-6.
Return to footnote 153 referrer
Uguz F, Akman C, Kaya N, Cilli AS. Postpartum-onset obsessive-compulsive disorder: incidence, clinical features, and related factors. J Clin Psychiatry. 2007;68(1):132-8.
Return to footnote 154 referrer
Zambaldi CF, Cantilino A, Montenegro AC, Paes JA, de Albuquerque TLC, Sougey EB. Postpartum obsessive-compulsive disorder: prevalence and clinical characteristics. Compr Psychiatry. 2009;50(6):503-9.
Return to footnote 155 referrer
Uguz F, Gezginc K, Zeytinci IE, Karatayli S, Askin R, Guler O, et al. Obsessive-compulsive disorder in pregnant women during the third trimester of pregnancy. Compr Psychiatry. 2007;48(5):441-5.
Return to footnote 156 referrer
Speisman BB, Storch EA, Abramowitz JS. Postpartum obsessive‐compulsive disorder. J Obstet Gynecol Neonatal Nurs. 2011;40(6):680-90.
Return to footnote 157 referrer
Grekin R, O'Hara MW. Prevalence and risk factors of postpartum posttraumatic stress disorder: a meta-analysis. Clin Psychol Rev. 2014;34(5):389-401.
Return to footnote 158 referrer
Vigod SN, Seeman MV, Ray JG, Anderson GM, Dennis CL, Grigoriadis S, et al. Temporal trends in general and age-specific fertility rates among women with schizophrenia (1996–2009): A population-based study in Ontario, Canada. Schizophr Res. 2012;139(1):169-75.
Return to footnote 159 referrer
Chaudron LH, Pies RW. The relationship between postpartum psychosis and bipolar disorder: a review. J Clin Psychiatry. 2003;64(11):1284-92.
Return to footnote 160 referrer
Munk-Olsen T, Laursen TM, Pedersen CB, Mors O, Mortensen PB. New parents and mental disorders: a population-based register study. JAMA. 2006;296(21):2582-9.
Return to footnote 161 referrer
Heron, McGuinness, Blackmore ER, Craddock, Jones. Early postpartum symptoms in puerperal psychosis. BJOG. 2008;115(3):348-53.
Return to footnote 162 referrer
Ganjekar S, Desai G, Chandra PS. A comparative study of psychopathology, symptom severity, and short-term outcome of postpartum and nonpostpartum mania. Bipolar Disord. 2013;15(6):713-8.
Return to footnote 163 referrer
Engqvist I, Nilsson K. Experiences of the first days of postpartum psychosis: an interview study with women and next of kin in Sweden. Issues Ment Health Nurs. 2013;34(2):82-9.
Return to footnote 164 referrer
Heron J, Gilbert N, Dolman C, Shah S, Beare I, Dearden S, et al. Information and support needs during recovery from postpartum psychosis. BJOG. 2012;15(3):155-65.
Return to footnote 165 referrer
Spinelli MG. Maternal infanticide associated with mental illness: prevention and the promise of saved lives. Am J Psychiatry. 2004;161(9):1548-57.
Return to footnote 166 referrer
Doucet S, Letourneau N, Blackmore ER. Support needs of mothers who experience postpartum psychosis and their partners. J Obstet Gynecol Neonatal Nurs. 2012;41(2):236-45.
Return to footnote 167 referrer
Robertson E, Jones I, Haque S, Holder R, Craddock N. Risk of puerperal and non-puerperal recurrence of illness following bipolar affective puerperal (post-partum) psychosis. Br J Psychiatry. 2005;186(3):258-9.
Return to footnote 168 referrer
Blackmore ER, Rubinow DR, O'Connor TG, Liu X, Tang W, Craddock N, et al. Reproductive outcomes and risk of subsequent illness in women diagnosed with postpartum psychosis. Bipolar Disord. 2013;15(4):394-404.
Return to footnote 169 referrer
Mackeen AD, Mackeen AD, Packard RE, Packard RE, Ota E, Ota E, et al. Antibiotic regimens for postpartum endometritis. Cochrane Database Syst Rev. 2015(2):CD001067.
Return to footnote 170 referrer
Smith Murray S, Slone McKinney E. Foundations of maternal-newborn & women's health nursing. 7 th ed. Toronto (ON): Elsevier; 2019.
Return to footnote 171 referrer
Lawrence RA, Lawrence RM. Breastfeeding: a guide for the medical professional. 8 th ed. New York (NY): Elsevier; 2015.
Return to footnote 172 referrer
Spencer JP, MD. Management of mastitis in breastfeeding women. Am Fam Physician. 2008;78(6):727-32.
Return to footnote 173 referrer
Bramham K, Nelson-Piercy C, Brown MJ, Chappell LC. Postpartum management of hypertension. BMJ. 2013;346(7897):30-4.
Return to footnote 174 referrer
Magee LA, Pels A, Helewa M, Rey E, von Dadelszen P. Diagnosis, evaluation, and management of the hypertensive disorders of pregnancy: executive summary. J Obstet Gynaecol Can. 2014;36(5):416-38.
Return to footnote 175 referrer
Heart and Stroke Foundation of Canada. Women's unique risk factors [Internet]. Ottawa (ON): Heart and Stroke Foundation of Canada; n.d. [cited 2020 July 24]. Available from: https://www.heartandstroke.ca/heart/risk-and-prevention/womens-unique-risk-factors
Return to footnote 176 referrer
American College of Obstetricians and Gynecologists. Practice bulletin no. 165: Prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynaecol. 2016;128(1):e1-15.
Return to footnote 177 referrer
Harvey M, Pierce M, Walter J, Chou Q, Diamond P, Epp A, et al. Obstetrical anal sphincter injuries (OASIS): prevention, recognition, and repair. J Obstet Gynaecol Can. 2015;37(12):1131-48.
Return to footnote 178 referrer
Royal College of Obstetricians and Gynaecologists. Third- and fourth-degree perineal tears, management (green-top guideline no.29) [Internet]. London (UK): RCOG; 2015 [cited 2020 July 24]. Available from: https://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg29/
Return to footnote 179 referrer
Chalmers B, Omer-Hashi K. Female genital mutilation and obstetric care. Victoria (BC): Trafford Publishing; 2003.
Return to footnote 180 referrer
Sperstad JB, Tennfjord MK, Hilde G, Ellström-Engh M, Bø K. Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. Br J Sports Med. 2016;50(17):1092-96.
Return to footnote 181 referrer
Fernandes da Mota PG, Pascoal AGBA, Carita AIAD, Bø K. Prevalence and risk factors of diastasis recti abdominis from late pregnancy to 6 months postpartum, and relationship with lumbo-pelvic pain. Man Ther. 2015; 2014;20(1):200-5.
Return to footnote 182 referrer
Rath A, Attali P, Dumas J, Goldlust D, Zhang J, Chevrel J. The abdominal linea alba: an anatomo-radiologic and biomechanical study. Surg Radiol Anat. 1996;18(4):281-8.
Return to footnote 183 referrer
Lee DG, Lee LJ, McLaughlin L. Stability, continence and breathing: The role of fascia following pregnancy and delivery. J Bodywork Move Ther. 2008;12(4):333-48.
Return to footnote 184 referrer
Gilleard WL, Brown JMM. Structure and function of the abdominal muscles in primigravid subjects during pregnancy and the immediate postbirth period. Phys Ther. 1996;76(7):750-62.
Return to footnote 185 referrer
Benjamin DR, van de Water ATM, Peiris CL. Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods: a systematic review. Physiotherapy. 2014;100(1):1-8.
Return to footnote 186 referrer
Hauck K, Davey R. Diastasis recti and pregnancy: 'closing the gap' between current treatment practices and clinical evidence [Internet]. Toronto (ON): Toronto Physiotherapy; 2015 [cited 2020 July 24]. Available from: http://torontophysiotherapy.ca/diastasis-recti-and-pregnancy-closing-the-gap-between-current-treatment-practices-and-clinical-evidence/
Return to footnote 187 referrer
Spitznagle TM, Leong FC, Van Dillen LR. Prevalence of diastasis recti abdominis in a urogynecological patient population. J Pelvic Floor Dysfunct. 2007;18(3):321-8.
Return to footnote 188 referrer
Kamel DM, Yousif AM. Neuromuscular electrical stimulation and strength recovery of postnatal diastasis recti abdominis muscles. Ann Rehabil Med. 2017;41(3):465-74.
Return to footnote 189 referrer
Thompson D, Berger H, Feig D, Gagnon R, Kader T, Keely E, et al. Diabetes and pregnancy. Can J Diabetes. 2013;37(1):S168-83.
Return to footnote 190 referrer
Tovar A, Chasan-Taber L, Eggleston E, Oken E. Postpartum screening for diabetes among women with a history of gestational diabetes mellitus. Prev Chronic Dis. 2011;8(6):A124.
Return to footnote 191 referrer
Kim C, Berger DK, Chamany S. Recurrence of gestational diabetes mellitus: a systematic review. Diabetes Care. 2007;30(5):1314-19.
Return to footnote 192 referrer
Keely E. An opportunity not to be missed - how do we improve postpartum screening rates for women with gestational diabetes? Diabetes Metab Res. 2012;28(4):312-6.
Return to footnote 193 referrer
Berger H, Gagnon R, Sermer M, Basso M, Bos H, Brown RN, et al. Diabetes in Pregnancy. J Obstet Gynaecol Can. 2016;38(7):667-79.e1.
Return to footnote 194 referrer
Matias SL, Dewey KG, Quesenberry CP, Gunderson EP. Maternal prepregnancy obesity and insulin treatment during pregnancy are independently associated with delayed lactogenesis in women with recent gestational diabetes mellitus. Am J Clin Nutr. 2014;99(1):115-21.
Return to footnote 195 referrer
Nommsen-Rivers LA, Chantry CJ, Peerson JM, Cohen RJ, Dewey KG. Delayed onset of lactogenesis among first-time mothers is related to maternal obesity and factors associated with ineffective breastfeeding. Am J Clin Nutr. 2010;92(3):574-84.
Return to footnote 196 referrer
Feig DS, Berger H, Donovan L, Godbout A, Kader T, Keely E, et al. Diabetes and pregnancy. Can J Diabetes. 2018;42(3):S255–82.
Return to footnote 197 referrer
Stagnaro-Green A, Abalovich M, Alexander E, Azizi F, Mestman J, Negro R, et al. Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and postpartum. Thyroid. 2011;21(10):1081-1125.
Return to footnote 198 referrer
National Collaborating Centre for Women's and Children's Health. Antenatal care routine care for the healthy pregnant woman [Internet]. London (UK): RCOG Press; 2008 [cited 2020 July 24]. Available from: https://www.nice.org.uk/guidance/cg62/evidence/evidence-tables-from-the-2003-version-pdf-196748322
Return to footnote 199 referrer
Aslan E, Fynes M. Symphysial pelvic dysfunction. Curr Opin Gynecol Obstet. 2007;19(2):133-9.
Return to footnote 200 referrer
Vleeming A, Albert HB, Östgaard HC, Sturesson B, Stuge B, Sahlgrenska akademin, et al. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J. 2008;17(6):794-819.
Return to footnote 201 referrer
Leadbetter RE, Mawer D, Lindow SW. Symphysis pubis dysfunction: a review of the literature. J Matern Fetal Neonatal Med. 2004;16(6):349-54.
Return to footnote 202 referrer
Kanakaris NK, Roberts CS, Giannoudis PV. Pregnancy-related pelvic girdle pain: an update. BMC Med. 2011;9(1):15.
Return to footnote 203 referrer
Wu WH, Meijer OG, Uegaki K, Mens JMA, van Dieën JH, Wuisman PIJM, et al. Pregnancy-related pelvic girdle pain (PPP), I: terminology, clinical presentation, and prevalence. Eur Spine J. 2004;13(7):575-89.
Return to footnote 204 referrer
Jain S, Eedarapalli P, Jamjute P, Sawdy R. Symphysis pubis dysfunction: a practical approach to management. Obstet Gynaecol. 2006;8(3):153-8.
Return to footnote 205 referrer
Pelvic Obstetric and Gynaecological Physiotherapy. Pregnancy-related pelvic girdle pain (PGP) – for health professionals [Internet]. London (UK): Chartered Society of Physiotherapy; 2015 [cited 2020 July 24]. Available from: http://pogp.csp.org.uk/publications/pregnancy-related-pelvic-girdle-pain-pgp-health-professionals
Return to footnote 206 referrer
Khorashadi L, Petscavage JM, Richardson ML. Postpartum symphysis pubis diastasis. Radiol Case Rep. 2011;6(3):542.
Return to footnote 207 referrer
Health Service Executive, Therapy Professions Committee, Institute of Obstetricians and Gynaecologists. Clinical practice guideline: management of pelvic girdle pain in pregnancy and post-partum [Internet]. Dublin (IE): Health Service Executive; 2012 [cited 2020 July 24]. Available from: https://www.hse.ie/eng/services/publications/clinical-strategy-and-programmes/management-of-pelvic-girdle-pain-in-pregnancy-and-post-partum.pdf
Return to footnote 208 referrer
Britnell SJ, Cole JV, Isherwood L, Sran MM, Stan MM, Britnell N, et al. Postural health in women: the role of physiotherapy. J Obstet Gynaecol Can. 2005;27(5):493-510.
Return to footnote 209 referrer
Canadian Institute for Health Information. Quick stats: childbirth indicators by place of residence. [Internet]. Ottawa (ON): CIHI; 2020 [cited 2020 July 24]. Available from: https://apps.cihi.ca/mstrapp/asp/Main.aspx?Server=apmstrextprd_i&project=Quick%20Stats&uid=pce_pub_en&pwd=&evt=2048001&visualizationMode=0&documentID=029DB170438205AEBCC75B8673CCE822
Return to footnote 210 referrer
Nielsen PE, Deering SH, Galan HL. Operative vaginal delivery. In: Gabbe SG, Niebyl JR, Simpson JL, et al. Obstetrics: normal and problem pregnancies. 7th ed. Philadelphia (PA): Elsevier; 2017.
Return to footnote 211 referrer
Meyer S, Hohlfeld P, Achtari C, Russolo A, Grandi P. Birth trauma: short and long term effects of forceps delivery compared with spontaneous delivery on various pelvic floor parameters. BJOG. 2000;107(11):1360-5.
Return to footnote 212 referrer
Briggs J. The Joanna Briggs Institute best practice information sheet: The effectiveness of pelvic floor muscle exercises on urinary incontinence in women following childbirth. Nurs Health Sci. 2011;13(3):378-81.
Return to footnote 213 referrer
Brubaker L. Postpartum urinary incontinence: the problem is clear, but there is no simple solution. BMJ. 2002;324(7348):1227-8.
Return to footnote 214 referrer
Public Health Agency of Canada. Data tables - the maternity experiences survey (MES) 2006-2007 [Internet]. Ottawa (ON): PHAC; 2006 [cited 2020 July 24]. Available from: http://www.phac-aspc.gc.ca/rhs-ssg/pdf/tab-eng.pdf
Return to footnote 215 referrer
Boyle R, Hay-Smith EJC, Cody JD, Mørkved S. Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev. 2012;10:CD007471.
Return to footnote 216 referrer
Magali R, Ross S. Conservative management of urinary incontinence. J Obstet Gynaecol Can. 2018;40(2):E119-25.
Return to footnote 217 referrer
Yip S, Sahota D, Pang M, Chang A. Postpartum urinary retention. Acta Obstet Gynecol Scand. 2004;83(10):881-91.
Return to footnote 218 referrer
Carley ME, Carley JM, Vasdev G, Lesnick TG, Webb MJ, Ramin KD, et al. Factors that are associated with clinically overt postpartum urinary retention after vaginal delivery. Obstet Gynaecol. 2002;187(2):430-3.
Return to footnote 219 referrer
Health Service Executive, Institute of Obstetricians and Gynaecologists. Clinical practice guideline: management of urinary retention in pregnancy, post-partum and after gynaecological surgery [Internet]. Dublin (IE): Health Service Executive; 2018 [cited 2020 July 24]. Available from: https://rcpi-live-cdn.s3.amazonaws.com/wp-content/uploads/2018/06/UR-guidelines-for-clinical-care-pathway-17.05.18.pdf
Return to footnote 220 referrer
Lim JL. Post-partum voiding dysfunction and urinary retention: post-partum voiding dysfunction. Aust N Z J Obstet Gynaecol. 2010;50(6):502-5.
Return to footnote 221 referrer
Groutz A, Levin I, Gold R, Pauzner D, Lessing JB, Gordon D. Protracted postpartum urinary retention: the importance of early diagnosis and timely intervention. Neurourol Urodyn. 2011;30(1):83-6.
Return to footnote 222 referrer
Rizvi RM, Khan ZS, Khan ZS. Diagnosis and management of postpartum urinary retention. Int J Obstet Gynaecol. 2005;91(1):71-2.
Return to footnote 223 referrer
Borello-France D, Burgio KL, Richter HE, Zyczynski H, FitzGerald MP, Whitehead W, et al. Fecal and urinary incontinence in primiparous women. Obstet Gynaecol. 2006;108(4):863-72.
Return to footnote 224 referrer
Eason E, Labrecque M, Marcoux S, Mondor M. Anal incontinence after childbirth. CMAJ. 2002;166(3):326-30.
Return to footnote 225 referrer
Watson J, Hermann S, Johnson B. Developing a policy to support breastfeeding in women who are hospitalized and acutely ill. Nurs Womens Health. 2013;17(3):188-96.
Return to footnote 226 referrer
Roger Hixon Ontario Milk Bank. Evidence for the use of donor milk [Internet]. Toronto (ON): Sinai Health; 2018 [cited 2020 July 24]. Available from: https://www.milkbankontario.ca/research-and-resources/evidence-for-the-use-of-donor-milk/
Return to footnote 227 referrer
Sachs HC, American Academy of Pediatrics, Committee On Drugs. The transfer of drugs and therapeutics into human breast milk: an update on selected topics. Pediatrics. 2013;132(3):e796-809.
Return to footnote 228 referrer
Money D, Allen VM. The prevention of early-onset neonatal group B streptococcal disease. J Obstet Gynaecol Can. 2016;38(12):S326-35.
Return to footnote 229 referrer
Centers for Disease Control and Prevention. Group B strep (GBS): clinical overview [Internet]. Atlanta (GA): CDC; 2020 [cited 2020 July 29]. Available from: https://www.cdc.gov/groupbstrep/clinicians/index.html
Return to footnote 230 referrer
Sgro M, Campbell DM, Sankaran K, Tran D, Yudin M. Early-onset neonatal sepsis and meningitis [Internet]. Ottawa (ON): CPSP; 2012 [cited 2020 July 29]. Available from: https://www.cpsp.cps.ca/surveillance/study-etude/early-onset-neonatal-sepsis-and-meningitis
Return to footnote 231 referrer
American Academy of Pediatrics, American Heart Association. Neonatal resuscitation textbook. 6 th ed. Itasca (IL): American Academy of Pediatrics; 2011.
Thomas SL, Heaton J, Makaryus AN. Physiology, cardiovascular murmurs. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 [cited 2020 July 29]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK525958/
Return to footnote 233 referrer
Mejia E, Dhuper S. Innocent murmur. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 [cited 2020 July 29]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507849/
Return to footnote 234 referrer
Wight N, Marinelli KA, Academy of Breastfeeding Medicine. ABM clinical protocol #1: guidelines for blood glucose monitoring and treatment of hypoglycemia in term and late-preterm neonates, revised 2014. Breastfeed Med. 2014;9(4):173-9.
Return to footnote 235 referrer
Nicholl R. What is the normal range of blood glucose concentrations in healthy term newborns? Arch Dis Child. 2003;88(3):238-9.
Return to footnote 236 referrer
Adamkin DH, Papile L, Baley JE, Bhutani VK, Carlo WA, Kumar P, et al. Postnatal glucose homeostasis in late-preterm and term infants. Pediatrics. 2011;127(3):575-9.
Return to footnote 237 referrer
Narvey MR, Marks SD, Canadian Paediatric Society, Fetus and Newborn Committee. The screening and management of newborns at risk for low blood glucose. Paediatr Child Health. 2019;24(8):536-44.
Return to footnote 238 referrer
Andrade SE, Raebel MA, Brown J, Lane K, Livingston J, Boudreau D, et al. Use of antidepressant medications during pregnancy: a multisite study. Obstet Gynaecol. 2008;198(2):194.e1-5.
Return to footnote 239 referrer
Jefferies AL, Canadian Paediatric Society, Fetus and Newborn Committee. Selective serotonin reuptake inhibitors in pregnancy and infant outcomes. Paediatr Child Health. 2011;16(9):562.
Return to footnote 240 referrer
Hudak ML, Tan RC, American Academy of Pediatrics. Neonatal drug withdrawal. Pediatrics. 2012;129(2):e540-60.
Return to footnote 241 referrer
Lattimore KA, Donn SM, Kaciroti N, Kemper AR, Neal CR, Vazquez DM. Selective serotonin reuptake iInhibitor (SSRI) use during pregnancy and effects on the fetus and newborn: a meta-analysis. J Perinatol. 2005;25(9):595-604.
Return to footnote 242 referrer
Moses-Kolko EL, Bogen D, Perel J, Bregar A, Uhl K, Levin B, et al. Neonatal signs after late in utero exposure to serotonin reuptake inhibitors: literature review and implications for clinical applications. JAMA. 2005;293(19):2372-83.
Return to footnote 243 referrer
Perinatal Services BC. Newborn guideline 13: newborn nursing care pathway [Internet]. Vancouver (BC): PSBC; 2013 [cited 2020 July 29]. Available from: http://www.perinatalservicesbc.ca/Documents/Guidelines-Standards/Newborn/NewbornNursingCarePathway.pdf
Return to footnote 244 referrer
Public Health Agency of Canada. Perinatal health indicators for Canada 2017. Ottawa (ON): PHAC; 2017.
Return to footnote 245 referrer
Organization for Economic Cooperation and Development. Health at a glance 2013: OECD indicators. 7th ed. Washington (DC): Organization for Economic Cooperation & Development; 2013.
Return to footnote 246 referrer
Stavis RL. Small-for-gestational-age (SGA) infant [Internet]. Kenilworth (NJ): Merck Manual Professional Version; 2019 [cited 2020 July 29]. Available from: http://www.merckmanuals.com/en-ca/professional/pediatrics/perinatal-problems/small-for-gestational-age-sga-infant
Return to footnote 247 referrer
Zhang X, PhD, Decker A, MD, Platt RW, PhD, Kramer MS, MD. How big is too big? The perinatal consequences of fetal macrosomia. Obstet Gynaecol. 2008;198(5):517.e1-6.
Return to footnote 248 referrer
Mayo Clinic. Fetal macrosomia [Internet]. Scottsdale (AZ): Mayo Clinic; 2020 [cited 2020 July 29]. Available from: http://www.mayoclinic.org/diseases-conditions/fetal-macrosomia/basics/complications/con-20035423
Return to footnote 249 referrer
KC K, Shakya S, Zhang H. Gestational diabetes mellitus and macrosomia: a literature review. Ann Nutr Metab. 2015;66(2):14-20.
Return to footnote 250 referrer
Martins F, Oppolzer D, Santos C, Barroso M, Gallardo E. Opioid use in pregnant women and neonatal abstinence syndrome - a review of the literature. Toxics. 2019;7(1):9.
Return to footnote 251 referrer
British Columbia Centre on Substance Use, B.C. Ministry of Health, B.C. Ministry of Mental Health and Addictions, Perinatal Services BC. The treatment of opioid use disorder during pregnancy [Internet]. Vancouver (BC): BCCSU; 2018 [cited 2020 July 29.] Available from: http://www.bccsu.ca/wp-content/uploads/2018/06/OUD-Pregnancy.pdf
Return to footnote 252 referrer
Lacaze-Masmonteil T, O'Flaherty P, Canadian Paediatric Society, Fetus and Newborn Committee. Managing infants born to mothers who have used opioids during pregnancy [Internet]. Ottawa (ON): CPS; 2018 [cited 2020 July 29]. Available from: https://cps.ca/en/documents/position/opioids-during-pregnancy
Return to footnote 253 referrer
Wong S, Ordean A, Kahan M, Society of Obstetricians and Gynecologists of Canada. Substance use in pregnancy. Int J Gynaecol Obstet. 2011;114(2):190-202.
Return to footnote 254 referrer
Whyte RK, Hilliard RI, Jefferies AL, Peliowski-Davidovich A, Sorokan ST, Whyte HEA. Safe discharge of the late preterm infant. Paediatr Child Health. 2010;15(10):655-60.
Return to footnote 255 referrer
Boyle EM, Johnson S, Manktelow B, Seaton SE, Draper ES, Smith LK, et al. Neonatal outcomes and delivery of care for infants born late preterm or moderately preterm: a prospective population-based study. Arch Dis Child Fetal Neonatal Ed. 2015;100(6):F479-85.
Return to footnote 256 referrer
Parikh LI, Reddy UM, Männistö T, Mendola P, Sjaarda L, Hinkle S, et al. Neonatal outcomes in early term birth. Obstet Gynaecol. 2014;211(3):265.e1-11.
Return to footnote 257 referrer
Ramphul M, Kennelly M, Burke G, Murphy D. Risk factors and morbidity associated with suboptimal instrument placement at instrumental delivery: observational study nested within the instrumental delivery & ultrasound randomised controlled trial. BJOG. 2015;122(4):558-63.
Return to footnote 258 referrer
Edozien LC. Towards safe practice in instrumental vaginal delivery. Best Pract Res Clin Obstet Gynaecol. 2007;21(4):639-55.
Return to footnote 259 referrer
Demissie K, Rhoads GG, Smulian JC, Balasubramanian BA, Gandhi K, Joseph KS, et al. Operative vaginal delivery and neonatal and infant adverse outcomes: population based retrospective analysis. BMJ. 2004;329(7456):24-6.
Return to footnote 260 referrer
Lemacks J, Fowles K, Mateus A, Thomas K. Insights from parents about caring for a child with birth defects. Int J Environ Res Public Health. 2013;10(8):3465-82.
Return to footnote 261 referrer
Stone MB, Botto LD, Feldkamp ML, Smith KR, Roling L, Yamashiro D, et al. Improving quality of life of children with oral clefts: perspectives of parents. J Craniofac Surg. 2010;21(5):1358-64.
Return to footnote 262 referrer
Kaye, C.I. Reducing cultural barriers to the provision of genetic services in South Texas, final report [Internet]. San Antonio (TX): Maternal and Child Health Library – Georgetown University; 2003 [cited 2020 July 29]. Available from: https://www.mchlibrary.org/MCHBfinalreports/docs/fr00109.pdf
Return to footnote 263 referrer
Shilling V, Morris C, Thompson-Coon J, Ukoumunne O, Rogers M, Logan S. Peer support for parents of children with chronic disabling conditions: a systematic review of quantitative and qualitative studies. Dev Med Child Neurol. 2013;55(7):602-9.
Return to footnote 264 referrer
O'Brien K, Bracht M, Robson K, Ye XY, Mirea L, Cruz M, et al. Evaluation of the family integrated care model of neonatal intensive care: a cluster randomized controlled trial in Canada and Australia. BMC Pediatr. 2015;15(1):210.
Return to footnote 265 referrer
Family Integrated Care. Program development [Internet]. Tampa (FL): FICare; 2016 [cited 2020 July 29]. Available from: http://familyintegratedcare.com/implementing-ficare/program- development/
Return to footnote 266 referrer
Cooper LG, Gooding JS, Gallagher J, Sternesky L, Ledsky R, Berns SD. Impact of a family-centered care initiative on NICU care, staff and families. J Perinatol. 2007;27(S2):S32-7.
Return to footnote 267 referrer
Griffin T, Celenza J. Family-centered care for the newborn: The delivery room and beyond. New York (NY): Springer Publishing Company; 2014.
Return to footnote 268 referrer
O'Brien K, Robson K, Bracht M, Cruz M, Lui K, Alvaro R, et al. Effectiveness of family integrated care in neonatal intensive care units on infant and parent outcomes: a multicentre, multinational, cluster-randomised controlled trial. Lancet Child Adolesc Health. 2018;2(4):245-54.
Return to footnote 269 referrer
Davidson JE, Aslakson RA, Long AC, Puntillo KA, Kross EK, Hart J, et al. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med. 2017;45(1):103-28.
Return to footnote 270 referrer
Craig JW, Glick C, Phillips R, Hall SL, Smith J, Browne J. Recommendations for involving the family in developmental care of the NICU baby. J Perinatol. 2015;35(S1):S5-8.
Return to footnote 271 referrer
Family Integrated Care. About FICare [Internet]. Tampa (FL): FICare; 2017 [cited 2020 July 29]. Available from: http://familyintegratedcare.com/about-ficare/
Return to footnote 272 referrer
Banerjee J. Are single family rooms the future for neonatal units? Lancet Child Adolesc Health. 2019;3(3):130-1.
Return to footnote 273 referrer
Banerjee J, Aloysius A, Platonos K, Deierl A. Family centred care and family delivered care – What are we talking about? J Neonatal Nurs. 2018;24(1):8-12.
Return to footnote 274 referrer
Stevens D, Thompson P, Helseth C, Pottala J. Mounting evidence favoring single-family room neonatal intensive care. J Neonatal Perinatal Med. 2015;8(3):177-8.
Return to footnote 275 referrer
van Veenendaal NR, Heideman WH, Limpens J, van der Lee JH, van Goudoever JB, van Kempen AAMW, et al. Hospitalising preterm infants in single family rooms versus open bay units: a systematic review and meta-analysis. Lancet Child Adolesc Health. 2019;3(3):147-57.
Return to footnote 276 referrer
Harris DD, Shepley MM, White RD, Kolberg KJS, Harrell JW. The impact of single family room design on patients and caregivers: executive summary. J Perinatol. 2006;26:38-48.
Return to footnote 277 referrer
Als H, McAnulty GB. The newborn individualized developmental care and assessment program (NIDCAP) with kangaroo mother care (KMC): comprehensive care for preterm infants. Curr Womens Health Rev. 2011;7(3):288.
Return to footnote 278 referrer
Symington A, Pinelli J. Developmental care for promoting development and preventing morbidity in preterm infants. Cochrane Database Syst Rev. 2006(2):CD001814.
Return to footnote 279 referrer
Trajkovski S, Schmied V, Vickers M, Jackson D. Neonatal nurses' perspectives of family‐centred care: a qualitative study. J Clin Nurs. 2012;21(17‐18):2477-87.
Return to footnote 280 referrer
Ramezani T, Hadian Shirazi Z, Sabet Sarvestani R, Moattari M. Family-centered care in neonatal intensive care unit: a concept analysis. Int J Community Based Nurs Midwifery. 2014;2(4):268-78.
Return to footnote 281 referrer
Kearvell H, Grant J. Getting connected: how nurses can support mother/infant attachment in the neonatal intensive care unit. Aust J Adv Nurs. 2010;27(3):75-82.
Return to footnote 282 referrer
National Institute for Health and Care Excellence. Neonatal specialist care [Internet]. London (UK): NICE; 2010 [cited 2020 Jul 29]. Available from: https://www.nice.org.uk/guidance/qs4
Return to footnote 283 referrer
Association of Women's Health, Obstetric and Neonatal Nursing. Guidelines for professional registered nurse staffing for perinatal units: executive summary. J Obstet Gynecol Neonatal Nurs. 2011;40(1):131-4.
Return to footnote 284 referrer
White RD. Development of care in the NICU. J Perinatol. 2014;34(3):174-5.
Return to footnote 285 referrer
Joshi A, Chyou P-, Tirmizi Z, Gross J. Web camera use in the neonatal intensive care unit: impact on nursing workflow. Clin Med Res. 2016;14(1):1-6.
Return to footnote 286 referrer
Best Start Resource Centre. Prenatal education: key messages for Ontario [Internet]. Toronto (ON): Best Start; 2016 [cited 2020 July 29]. Available from: https://resources.beststart.org/product/e49e-prenatal-education-key-messages-for-ontario-website/
Return to footnote 287 referrer
Irwin LG, Siddiqi A, Hertzman C. Early child development : a powerful equalizer: final report for the World Health Organization's Commission on the Social Determinants of Health [Internet]. Geneva (CH): WHO; 2007 [cited 2020 July 29]. Available from: https://apps.who.int/iris/handle/10665/69729
Return to footnote 288 referrer
BC Women's Hospital & Health Centre, British Columbia Centre of Excellence for Women's Health. A women's health strategy for British Columbia: advance the health of girls and women [Internet]. Vancouver (BC): BCCEWH; 2004 [cited 2020 July 29]. Available from: http://bccewh.bc.ca/wp-content/uploads/2012/05/2004_Advancing-Health-Girls-Women.pdf
Return to footnote 289 referrer
British Columbia Ministry of Health. Recommendations from the maternity care enhancement project [Internet]. Vancouver (BC): British Columbia Ministry of Health; 2004 [cited 2020 July 29]. Available from: https://www.health.gov.bc.ca/library/publications/year/2004/mcep_recommend_dec2004.pdf
Return to footnote 290 referrer
Public Health Agency of Canada. Population health approach: the organizing framework [Internet]. Ottawa (ON): PHAC; 2013 [cited 2020 July 29]. Available from: https://cbpp-pcpe.phac-aspc.gc.ca/population-health-approach-organizing-framework/
Return to footnote 291 referrer
Champlain Maternal Newborn Regional Program. Mapping of the maternal-newborn care spectrum in the Champlain and southeast LHINS: final report and recommendations [Internet]. Ottawa (ON): CMNRP; 2017 [cited 2020 July 31]. Available from: https://instantweb.secure-form2.com/uploads/documents//Mapping_of_Maternal_Newborn_Service_Final_Report_Nov20_2017.pdf
Return to footnote 292 referrer
Best Start Resource Centre. Abuse in pregnancy: information and strategies for the prenatal educator [Internet]. Toronto (ON): Best Start; 2015 [cited 2020 July 31]. Available from: https://resources.beststart.org/wp-content/uploads/2016/01/H04-E.pdf
Return to footnote 293 referrer
Beydoun HA, Al-Sahab B, Beydoun MA, Tamim H. Intimate partner violence as a risk factor for postpartum depression among Canadian women in the maternity experience survey. Ann Epidemiol. 2010;20(8):575-83.
Return to footnote 294 referrer
World Health Organization. Child maltreatment: the health sector responds [Internet]. Geneva (CH): WHO; 2017 [cited 2020 July 31]. Available from: https://www.who.int/violence_injury_prevention/violence/child/Child_maltreatment_infographic_EN.pdf?ua=1
Return to footnote 295 referrer
Sinha M. Family violence in Canada: a statistical profile, 2010 [Internet]. Ottawa (ON): Statistics Canada; 2012 [cited 2020 July 31]. Available from: https://www150.statcan.gc.ca/n1/en/pub/85-002-x/2012001/article/11643-eng.pdf?st=swG0oiwz
Return to footnote 296 referrer
Paolozza C, Packard B, Kulkarni C. A call to action on behalf of maltreated infants and toddlers in Canada [Internet]. Toronto (ON) Infant Mental Health Promotion; 2017 [cited 2020 July 31]. Available from: http://www.imhpromotion.ca/Resources/CalltoAction
Return to footnote 297 referrer
Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study. Am J Prev Med. 1998;14(4):245-58.
Return to footnote 298 referrer
World Health Organization. Responding to intimate partner violence and sexual violence against women: WHO clinical and policy guidelines [Internet]. Geneva (CH): WHO; 2013 [cited 2020 July 31]. Available from: https://www.who.int/reproductivehealth/publications/violence/9789241548595/en/
Return to footnote 299 referrer
VEGA Family Violence Project. VEGA family violence education resources [Internet]. Hamilton (ON): McMaster University; 2019 [cited 2020 July 31]. Available from: https://vegaproject.mcmaster.ca/
Return to footnote 300 referrer
World Health Organization. Health care for women subjected to intimate partner violence or sexual violence: a clinical handbook [Internet]. Geneva (CH): WHO; 2014 [cited 2020 July 31]. Available from: https://www.who.int/reproductivehealth/publications/violence/vaw-clinical-handbook/en/
Return to footnote 301 referrer
Wilson RD. Pre-conception folic acid and multivitamin supplementation for the primary and secondary prevention of neural tube defects and other folic acid-sensitive congenital anomalies. J Obstet Gynaecol Can. 2015;37(6):534-49.
Return to footnote 302 referrer
Tarasuk V, Mitchell A, Dachner N. Household food insecurity in Canada, 2014 [Internet]. Toronto (ON): University of Toronto; 2016 [cited 2020 July 31]. Available from: https://proof.utoronto.ca/wp-content/uploads/2016/04/Household-Food-Insecurity-in-Canada-2014.pdf
Return to footnote 303 referrer
Dietitians of Canada. Addressing household food insecurity in Canada - position statement and recommendations. Can J Diet Pract Res. 2016;77(3):159.
Return to footnote 304 referrer
O'Connor DL, Blake J, Bell R, Bowen A, Callum J, Fenton S, et al. Canadian consensus on female nutrition: adolescence, reproduction, menopause, and beyond. J Obstet Gynaecol Can. 2016;38(6):508-554.e18.
Return to footnote 305 referrer
Incollingo Rodriguez AC, Dunkel Schetter C, Tomiyama AJ. Weight stigma among pregnant and postpartum women: A new context of stigmatization. Stigma Health. 5(2):209-16.
Return to footnote 306 referrer
Yim IS, Tanner Stapleton LR, Guardino CM, Hahn-Holbrook J, Dunkel Schetter C. Biological and psychosocial predictors of postpartum depression: systematic review and call for integration. Annu Rev Clin Psychol. 2015;11(1):99-137.
Return to footnote 307 referrer
Nusbaum MRH, Gamble G, Skinner B, Heiman J. The high prevalence of sexual concerns among women seeking routine gynecological care. J Fam Pract. 2000;49(3):229-32.
Return to footnote 308 referrer
Basson R, Leiblum S, Brotto L, Derogatis L, Fourcroy J, Fugl-Meyer K, et al. Definitions of women's sexual dysfunction reconsidered: advocating expansion and revision. J Psychosom Obstet Gynaecol. 2003;24(4):221-9.
Return to footnote 309 referrer
Von Sydow K, Ullmeyer M, Happ N. Sexual activity during pregnancy and after childbirth: results from the sexual preferences questionnaire. J Psychosom Obstet Gynaecol. 2001;22(1):29-40.
Return to footnote 310 referrer
von Sydow K. Sexuality during pregnancy and after childbirth: a metacontent analysis of 59 studies. J Psychosom Res. 1999;47(1):27-49.
Return to footnote 311 referrer
Hicks TL, Goodall SF, Quattrone EM, Lydon-Rochelle MT. Postpartum sexual functioning and method of delivery: summary of the evidence. J Midwifery Womens Health. 2004;49(5):430-6.
Return to footnote 312 referrer
Buhling KJ, Schmidt S, Robinson JN, Klapp C, Siebert G, Dudenhausen JW. Rate of dyspareunia after delivery in primiparae according to mode of delivery. Eur J Obstet Gynecol Reprod Biol. 2006;124(1):42-6.
Return to footnote 313 referrer
Connolly A, Thorp J, Pahel L. Effects of pregnancy and childbirth on postpartum sexual function: a longitudinal prospective study. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(4):263-7.
Return to footnote 314 referrer
Barrett G, Peacock J, Victor CR, Isaac. Cesarean section and postnatal sexual health. Birth. 2005;32(4):306-11.
Return to footnote 315 referrer
Black A, Francoeur D, Rowe T. Canadian contraception consensus. J Obstet Gynaecol. Can 2004 April 2004;26(4):347-87.
Return to footnote 316 referrer
Society of Obstetricians and Gynaecologists of Canada. Postpartum – contraception [Internet]. Ottawa (ON): SOGC; 2020 [cited 2020 July 31]. Available from: https://www.pregnancyinfo.ca/postpartum/postpartum/contraception/
Return to footnote 317 referrer
World Alliance for Breastfeeding Action. LAM – The lactational amenorrhea method [Internet]. Penang (MY): WABA; 2017 [cited 2020 July 31]. Available from: http://www.waba.org.my/resources/lam/
Return to footnote 318 referrer
Guttmann A, Shulman R, Manuel D. Improving accountability for children's health: immunization registries and public reporting of coverage in Canada. Paediatr Child Health. 2011;16(1):16-8.
Return to footnote 319 referrer
Public Health Agency of Canada. Message from the Chief Public Health Officer of Canada: national immunization awareness week - April 23 to 30, 2016 [Internet]. Ottawa (ON): PHAC; 2016 [cited 2020 July 31]. Available from: https://www.canada.ca/en/public-health/news/2016/04/message-from-the-chief-public-health-officer-of-canada-national-immunization-awareness-week-april-23-to-30-2016.html
Return to footnote 320 referrer
Public Health Agency of Canada. Vaccine coverage in Canadian children: highlights from the 2013 childhood national immunization coverage survey (cNICS) [Internet]. Ottawa (ON): PHAC; 2016 [cited 2020 July 31]. Available from: https://www.canada.ca/en/public-health/services/publications/healthy-living/vaccine-coverage-canadian-children-highlights-2013-childhood-national-immunization-coverage-survey.html?_ga=1.10659505.462930771.1474382704
Return to footnote 321 referrer
Public Health Agency of Canada. Guidelines for measles outbreak in Canada [Internet]. Ottawa (ON): PHAC; 2013 [cited 2020 July 31]. Available from: https://www.canada.ca/en/public-health/services/reports-publications/canada-communicable-disease-report-ccdr/monthly-issue/2013-39/guidelines-prevention-control-measles-outbreaks-canada.html
Return to footnote 322 referrer
Wilson SE, Deeks SL, Seo CY, Lim GH, Fediurek J, Crowcroft NS. Trends in medical and nonmedical immunization exemptions to measles-containing vaccine in Ontario: an annual cross-sectional assessment of students from school years 2002/03 to 2012/13. CMAJ 2015;3(3):E317-23.
Return to footnote 323 referrer
Busby C, Jacobs A, Muthukumaran R. In need of a booster: how to improve childhood vaccination coverage in Canada [Internet]. Toronto (ON): C.D. Howe Institute; 2017 [cited 2020 July 31]. Available from: https://www.cdhowe.org/sites/default/files/attachments/research_papers/mixed/Commentary_477.pdf
Return to footnote 324 referrer
MacDonald NE, Desai S, Gerstein B. Working with vaccine-hesitant parents: an update. Paediatr Child Health. 2018;23(8):561.
Return to footnote 325 referrer
De Vries R, Wiegers TA, Smulders B, Teijlingen Ev. The Dutch obstetrical system: vanguard of the future in maternity care. In: Davis-Floyd R, Barclay L, Daviss, BA, Tritten J. Birth models that work. Berkeley (CA): University of California Press; 2019.
Return to footnote 326 referrer
Expatica. Having a baby in France [Internet]. Haarlem (NL): Expatica; 2020 [cited 2020 July 31]. Available from: https://www.expatica.com/fr/healthcare/womens-health/having-a-baby-in-france-107664/
Return to footnote 327 referrer
Reproductive Care Program of Nova Scotia. Healthy babies, healthy families: postpartum & postnatal guidelines [Internet]. Halifax (NS): Nova Scotia Department of Health; 2012 [cited 2020 July 31]. Available from: https://novascotia.ca/dhw/publications/Public-Health-Education/Postpartum%20Guidelines.pdf
Return to footnote 328 referrer
Monarch. About us [Internet]. Ottawa (ON): Monarch Centres – Maternal and Newborn Health; 2015 [cited 2020 July 31]. Available from: http://www.monarchcentre.ca/us/
Return to footnote 329 referrer
Children's Health Policy Centre. Nurse-family partnership is being tested in Canada [Internet]. Vancouver (BC): Simon Fraser University; 2020 [cited 2020 July 31]. Available from: https://childhealthpolicy.ca/nurse-family-partnership/
Return to footnote 330 referrer
Nurse-Family Partnership Canada. Nurse-family partnership Canada [Internet]. Hamilton (ON): McMaster University; 2015 [cited 2020 July 31]. Available from: https://nfp.mcmaster.ca
Return to footnote 331 referrer
Public Health Agency of Canada. Canada prenatal nutrition program (CPNP) [Internet]. Ottawa (ON): PHAC; 2020 [cited 2020 July 31]. Available from: https://www.canada.ca/en/public-health/services/health-promotion/childhood-adolescence/programs-initiatives/canada-prenatal-nutrition-program-cpnp.html
Return to footnote 332 referrer
Public Health Agency of Canada. Community action program for children (CAPC) [Internet]. Ottawa (ON): PHAC; 2020 [cited 2020 July 31]. Available from: https://www.canada.ca/en/public-health/services/health-promotion/childhood-adolescence/programs-initiatives/community-action-program-children-capc.html
Return to footnote 333 referrer
Association of American Medical Colleges. Implementing curricular and institutional climate changes to improve health care for individuals who are LGBT, gender nonconforming, or born with DSD [Internet]. Washington (DC): AAMA; 2014 [cited 2020 June 24]. Available from: https://store.aamc.org/implementing-curricular-and-institutional-climate-changes-to-improve-health-care-for-individuals-who-are-lgbt-gender-nonconforming-or-born-with-dsd-a-resource-for-medical-educators.html
Return to footnote 334 referrer
Page details
- Research article
- Open access
- Published: 06 January 2020
Knowledge on postnatal care among postpartum mothers during discharge in maternity hospitals in Asmara: a cross-sectional study
- Ghirmay Ghebreigziabher Beraki ORCID: orcid.org/0000-0003-3933-0835 1 ,
- Eyasu H. Tesfamariam 2 ,
- Amanuel Gebremichael 1 ,
- Berhanemeskel Yohannes 1 ,
- Kessete Haile 1 ,
- Shewit Tewelde 1 &
- Simret Goitom 1
BMC Pregnancy and Childbirth volume 20 , Article number: 17 ( 2020 ) Cite this article
42k Accesses
12 Citations
Metrics details
The early postnatal period is a dangerous time for both mother and baby where morbidity and mortality are highly prevalent if proper care is not done. Post natal care (PNC) knowledge has significant role in reducing such complications. In this study, the knowledge of postpartum mothers on PNC and its determinants were determined.
A cross-sectional quantitative study was conducted in postpartum mothers (PpM) who attended all maternal delivery services in Asmara. Data was collected by a structured questionnaire. All ( n = 250) PpM who gave birth in December, 2017 were included in the study. Independent samples t-test and one way ANOVA were used to compare the scores in knowledge across categories of background characteristics using SPSS. Bonferroni post-hoc test was performed for variables that were found to be significant while using ANOVA tool. P -values less than 0.05 were considered as significant.
The percentage of PpM who cited vaginal bleeding, as a maternal danger sign, and fever, as a baby danger sign, were 83.2 and 58.8%, respectively. The majority (96%) of PpM responded the correct answer on where to go if they note any danger signs. In addition, more than nine tenth of PpM correctly identified injectable contraceptives (92.7%) and oral contraceptive (91.5%). The percentages of knowledge in recognizing the necessary nutrients ranged from 87.6% for carbohydrates to 46% for minerals. The percentages of correct knowledge regarding first baby bath, frequency of breast feeding, umbilical care, duration of exclusive breast feeding, need and purpose of vaccine were 40.1, 81.9, 77.4, 94.8, and 99.2% respectively. The mean PNC knowledge score was 24.89/60. The score of knowledge on postnatal care was found to significantly differ across the categories of residence ( p < 0.001) and ethnicity ( p = 0.015). An increasing trend of knowledge score was observed with increase in age group ( p < 0.001), educational level ( p = 0.021), gravida ( p < 0.001) and para ( p < 0.001).
Considerable gaps in knowledge regarding postnatal care among postpartum mothers were evident. Special attention should be laid on rural residents, single/living together, junior/below in educational level, primigravida/para, non-Tigrigna ethnicity, and 17 to 25 years old mothers.
Peer Review reports
Post-natal care refers to issues pertaining to the mother and the baby from birth up to 6 weeks [ 1 ]. The goal of care during the early postnatal period is to promote the physical well-being of both mother and baby, as well as support the developing relationship between the baby and his or her parents and family. In addition, it can also support the development of infant feeding skills and strengthen the mother’s knowledge and confidence in her and her baby’s health and well-being. Accordingly, postnatal care knowledge enables mothers to develop parenting skills to fulfill their mothering role within their particular family [ 2 ].
Lack of appropriate postnatal care sometimes may result in death or disability of the mother and/or newborn [ 3 ]. Worldwide, nearly 600,000 mothers between the ages of 15–49 years die every year due to complications arising from pregnancy and childbirth. Hence, maternal death occurs almost every minute of every year, out of which 99% are in the developing countries [ 3 ]. Around two thirds of maternal and newborn deaths occur in the early postpartum period in developing countries and most of them in sub-Saharan Africa [ 1 , 4 ]. Almost half of postnatal maternal deaths occur within the first 24 h and 66% occur during the first week [ 1 , 5 ]. In 2013, 2.8 million newborns died in their first month of life, from which 1 million died on the first day [ 5 ].
There has been great emphasis on skilled attendant delivery and efforts have been made to improve PNC guidelines globally and nationally [ 1 ]. In sub-Saharan Africa, 48% of women give birth with the assistance of skilled personnel [ 5 ]. A review of sub-Saharan Africa demographic and health survey showed that only 13% of women who delivered at home received postnatal care within 2 days of birth [ 5 ]. The majority of health care providers across sub-Saharan Africa, including Eritrea, continue to advise mothers to come back to the facility for a first check-up after 6 weeks [ 6 ]. Despite these services and advice, maternal and neonatal mortality and morbidity in Eritrea were extremely high [ 7 ] . According to a WHO report, infant mortality rate was 36 deaths per 1000 live births and maternal mortality ratio was 501 per 100,000 live births in 2015 [ 7 , 8 ]. In Eritrea, only 34% of the mothers who give birth were served by trained health workers [ 9 ]. Consequently, only 2% of women who had home deliveries receive postnatal care during the first 2 days of post-partum, and another 5 and 7% of such women had postnatal care within 5 to 41 days post-partum [ 10 ]. Hence, providing the needed services and advice might not always necessarily lead to achievement of the required goals.
Maternal and child health is one of the basic needs of a society for it is the cornerstone on which a health community and nation are built. Hence, the ministry of health of Eritrea has postnatal care program with sequence of activities that begins with clean delivery practice, followed by clean umblical cord care, thermal care, special care of low birth weight or preterm birth, early and exclusive breastfeeding, as well as immunization programs. However, postnatal care health education given to postpartum mothers in the maternity health facilities of Eritrea is not based on standard guidelines. On the other hand, while discharging the postpartum mothers from the hospital, list of common postnatal danger signs are given in a piece of paper to inform them that they have to approach a nearby health facility upon their appearance.
Postpartum mothers can pass the critical postpartum period successfully if they have knowledge regarding postnatal care [ 11 ]. A study conducted in Malawi on assessment of the knowledge and practice of postpartum mothers regarding postnatal care showed that almost all the participants were knowledgeable about some aspect of postnatal care [ 12 ]. However, other studies have shown women’s insufficient knowledge on postnatal care [ 13 , 14 ]. As far as the researchers’ knowledge is concerned, no published resource regarding maternal level of knowledge on postnatal care upon discharge in Eritrea exists. Therefore, this study is designed to determine maternal knowledge regarding PNC and to find out the socio-demographic determinants of knowledge scores on postnatal care among postpartum mothers.
Study design and period
Cross-sectional study design with quantitative approach was used to determine the knowledge of postnatal care among postpartum mothers during discharge in maternity hospitals in Asmara. The study was conducted in December, 2017.
Study area and population
The study was conducted in the health facilities which provide delivery service in Asmara. Asmara is the capital city of Eritrea, a country in the horn of Africa. This capital city is located 2325 m above sea level with a total area of 44.97km 2 . According to 2017 Asmara municipality report, it has a population size of 416,367. Maternity hospitals in the city are Orotta National Referral Maternity Hospital, Sembel Hospital, Edaga Hamus Community Hospital, and Betmekae Community Hospital. Postpartum mothers who delivered in these four hospitals during the study period constituted the study population.
Participants
Complete enumeration of the postpartum mothers was undertaken to determine the knowledge of postpartum mothers on postnatal care. This is because all subjects during the specified period of time can be recruited resulting to more accuracy, than that of samples. Hence, all health facilities (4 Hospitals) that render maternity services as well as all eligible postpartum mothers ( N = 334) who have given birth during the study period in the study area were considered but only 250 were finally included in the study.
The dependent variable in the study was the knowledge of postnatal care among mothers who had given birth. The selected determinants were age, marital status, religion, educational level, and occupation.
Data collection tool and variable measurement
A questionnaire was developed with reference to a guideline prepared by WHO on post-natal care of the mother and new born [ 1 ] and previous similar studies conducted in Kenya [ 15 ] and Tanzania [ 16 ]. After compiling the questionnaire, content validity was assessed using panel of experts from Ministry of Health and Asmara College of Health Sciences. On the other hand, the internal consistency of the tool was computed and found to be within the acceptable range (Richard’s Kurdson = 0.75). Then, the questionnaire was translated from English to Tigrigna, a language most familiar to Eritreans, by experienced researchers, linguists, and midwife experts.
The questionnaire was pre-tested among 30 postpartum mothers in Orotta National Referral Maternity Hospital 1 month before the study period. The interview was done face- to- face by five degree midwife nurses who can speak and understand the language. Pre-designed questions that were not easily understood by the interviewee were simplified after pre-testing the questionnaire. Furthermore, re-arrangement of the questions were made.
The modified questionnaire had two main parts, namely, socio-demographic characteristics and questions that assess knowledge on postnatal care. There were in total 17 questions (with 60 items each having one score) that were used to determine the knowledge on postnatal care encompassing two main components: maternal care, and baby care. Maternal care component consisted of concerns on maternal danger signs (15 items), infection prevention (9 items), bladder care (1 item), sexual activity starting time (1 item), proper nutrition (6 items), delay of menstruation by exclusive breast feeding (1 item), and contraceptive methods (4 items). On the other hand, the baby care component consisted of mechanism of keeping the baby warm (2 items), time of first new born baby bath (1 item), umbilical care (1 item), initiation of breast feeding (1 item), frequency of breast feeding per day (1 item), exclusive breast feeding (1 item), needs and purposes of vaccination (2 items), and baby danger signs (14 items). Every item was scored by assigning one of the following options: “correct” (score = 1), and “wrong” (score = 0). An overall score was obtained by adding the correct responses totaling to 60. The scores indicate that with an increase in score, there is an increase of knowledge regarding postnatal care.
Data entry and analysis
After verification of the collected questionnaires by the researchers, the data was entered into CSPro (Census and Survey processing system) version 7.0 software package. The entered data was then exported to Statistical Package for Social Sciences (SPSS, version 22.0) for analysis. Frequency (percentage), mean (SD), or median (IQR) were used to describe the data, as appropriate. Normality of the knowledge score was assessed using Kolmogorov-Smirnov test. Independent samples t-test (variables with two categories) and one way ANOVA (variables with more than 2 categories) were used to find out the difference in the level of knowledge of post-natal across demographic variables. Bonferroni post hoc test was performed for the significant ANOVA results. P -values less than 0.05 were considered as significant.
Operational definition
Post-natal care refers to issues pertaining to the mother and the baby from birth up to 6 weeks [ 1 ].
Postpartum mothers are those mothers who have given birth in the health facility.
Data collectors were able to approach 334 postpartum mothers in the four hospitals during the study period. However, 27 delivered by caesarean section and 307 by spontaneous vaginal delivery (SVD). In addition, 30 subjects were excluded because they cannot speak Tigrigna (native language), 13 had still birth, and 14 withdrew from the study to arrive at 250 subjects included in the analysis (Fig. 1 ).
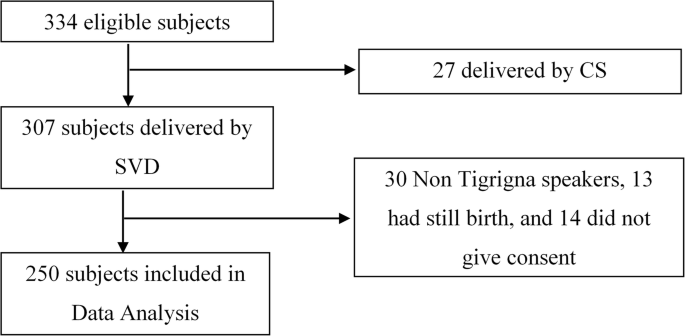
Study participants that were eligible and finally included in the analyses
Background characteristics of the postpartum mothers
An overview of the socio- demographic characteristics of 250 postpartum mothers during the study period on postnatal care is shown in Table 1 .
Obstetrical and gynecological history of the mothers revealed that, 28.4, 23.2, 22.8, 8.4, and 17.2% were gravida one, two, three, four, and five and above respectively (Table 2 ). On the other hand, 33.2% of respondents were primi para, 24.4% were para two, 18.8% were para three, 8.4% were para four and 15.2% were para five and above. Only 37(14.8%) of respondents had history of abortion.
Knowledge on maternal care
The percentage distribution of postpartum mothers on maternal danger signs are shown in Fig. 2 . The three most recognized maternal danger signs were heavy vaginal bleeding (83.2%), severe head ache (38.4%), and lower abdominal pain (32.0%).
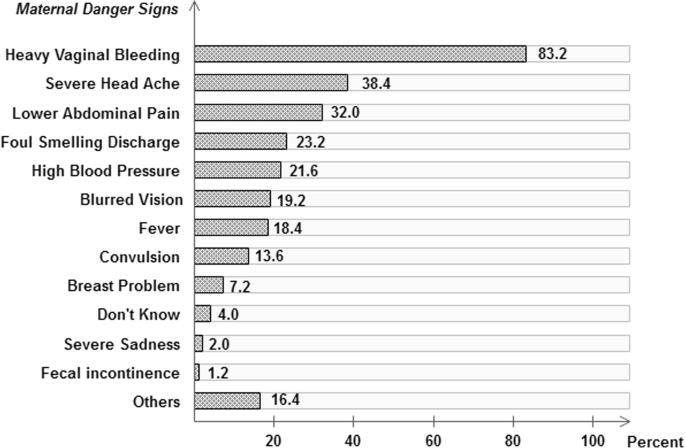
Knowledge of postnatal mothers on maternal danger signs. Others = vomiting, unconsciousness or edema
Almost all (96.0%) of the respondents responded correctly on where to go if they note any danger signs (Table 3 ). Emptying the bladder every 2 hours, which is the correct response for frequency of urination, was mentioned only by 35 (21.6%) of the postpartum mothers. The majority (74.1%) of the respondents mentioned “if I felt to urinate”. The minimum time for starting sexual intercourse was correctly responded by 114 (45.6%). Six different nutrients which are needed to be taken during postpartum were presented to the postpartum mothers for identification. More than 80 % of the postpartum mothers were able to identify food items rich in carbohydrates (87.6%). Moreover, 81.6% replied high fluid intake. Food rich in proteins (75.2%), vitamins (67.6%), fats (47.2%), and minerals (45.6%) were also mentioned. The percentages of women who responded delay in menstrual period as a result of giving exclusive breast feeding for 3 months, 6 months, 1 year, 2 years, and more than 2 years were 12.0, 26.4, 22.8, 17.6 and 21.2 respectively. More than nine tenth of postpartum mothers correctly identified injectable contraceptives (92.7%) and oral contraceptive (91.5%). The remaining had mentioned IUD (53.6%), LAM (16.9%) and other contraceptives (46.8%) such as condom, Norplant or calendar method.
Nine different infection prevention methods were presented to the postnatal mothers for identification (Table 4 ). Wash perineum with warm water and some salt (70.0%) and general body hygiene (69.6%) were highly known infection prevention methods. The remaining seven infection prevention methods were known by less than half of the postpartum mothers. Among the least known infection prevention methods were hand washing after changing pads (10.8%), hand washing after perineal hygiene (10.4%), and hand washing before perineal hygiene (6.8%).
Knowledge on baby care
Table 5 shows the percentage distribution of mothers by their knowledge on baby care. Knowledge on keeping the baby warm by wrapping the baby with cloth was almost universal (99.6%). Few (6.8%) also mentioned skin to skin contact. Correct response on the time at which first bath can be given for a new born baby was obtained from 67(26.8%) of the study participants. More than three fourths (77.4%) of the women responded umbilical care should be simply keeping clean and dry. Most of the respondents (88.40%) mentioned the correct answer on initiation of breast feeding after delivery which is within 30 min. Almost three fourths (74.0%) of the women correctly responded to the frequency need of breast feeding per day (eight per day); however, 10.4% said ‘if the baby cries’. The majority (94.8%) of respondents correctly answered that duration of exclusive breast feeding needs to be for 6 months. Almost all respondents (99.2%) correctly knew the needs of vaccine for a newborn baby. With regards to the purpose of vaccine, most of the respondents (94.8%) mentioned ‘to prevent disease’ and 13 (5.2%) did not know.
More than half of the respondents mentioned fever (58.8%), severe vomiting (53.2%), and difficulty in breathing (50.8%) as baby danger signs (Table 6 ). Almost one third of the women were able to identify the inability to breast feed (32.8%) and irritability (33.2%). Less than one fourth of the respondents cited umbilical problems (14.0%), abdominal distention (9.2%), convulsion (8.4%), lethargy (7.6%), yellowness of eyes (7.6%), eye problem (6.8%), yellowness of palms (2.8%), and yellowness of sole (1.6%). However, 19 (7.6%) of the respondents mentioned “I don’t know” and 101 (40.4%) responded vomiting/unconsciousness/ edema.
Comparison of knowledge scores
The results showed that the mean knowledge score was 24.89/60 (SD = 5.66). Independent sample t-test has revealed that the categories in residence ( p < 0.001) and ethnicity ( p = 0.015) had shown significant difference in score of knowledge on postnatal care among postpartum mothers (Table 7 ). However, occupation ( p = 0.210), religion ( p = 0.476), number of abortion ( p = 0.783) have not shown significant difference in score of knowledge on postnatal care among postpartum mothers.
Result from one way ANOVA (Table 8 ), revealed that there was significant difference in the average score of knowledge regarding post natal care among the postpartum mothers across different age groups ( p < 0.001), marital status ( p = 0.045), educational level ( p = 0.014), gravidity ( p < 0.001) and parity ( p < 0.001). An increasing trend of knowledge score was observed with increase in age group ( p = 0.001), educational level ( p = 0.021), gravidity ( p < 0.001) and parity ( p < 0.001).
Bonferroni post-hoc comparison showed that the postnatal knowledge score among mothers aged 17–25 was significantly less than 26–30, and 31–42 years old. Moreover, significantly higher knowledge score was observed among married and divorced as compared to single and living together. Postpartum mothers who are junior or below were also found to have significantly lower postnatal knowledge score as compared to mothers who are secondary and higher level. No significant difference in knowledge score was observed among mothers who were gravidity two, three, four, and five or above, however, mothers of gravidity one had significantly less knowledge score than mothers of the aforementioned gravidity. Similar results with that of the gravidity were observed for parity.
There are maternal and child health programs to safeguard maternal and child health in Eritrea. Nonetheless, maternal and neonatal mortality ratio still remain as high as 501/100,000 and 36/1000 live births, respectively, in the country [ 8 ]. Studies regarding utilization of maternal health services such as antenatal care and skilled delivery at birth are not infrequent; however, there still exists paucity of studies on knowledge regarding postnatal care in the country. One of the fundamental activities that needs to be instigated for the improvement of maternal and neonatal health is postnatal care because the majority of maternal and newborn death happen during this period [ 1 ]. Among others, one dimension of initiating postpartum care constitutes enhancing the knowledge of the mothers in order to enable them to properly handle themselves and the neonates in times of difficulty [ 17 ].
In this study, vaginal bleeding (83.2%) was the most frequently mentioned danger sign during the postpartum period. This finding is similar to a research conducted in Ethiopia (89.2%) [ 18 ] but lower than another study done in Nepal (98.47%) [ 3 ]. When compared with the study conducted in Ethiopia, a similar result observed is foul-smelling vaginal discharge (23.3%) as a danger sign [ 18 ]. However, in the Ethiopian study, relatively higher percentages of postnatal mothers identified severe headache (38.4% Vs 23.1%), blurred vision (19.2% Vs 8.9%), convulsion (13.6% Vs 7.9%) and lower abdominal pain (32.0% Vs 2.9%) as danger signs as compared to this study [ 18 ]. This could be due to the long standing public health campaigns given in Eritrea that bleeding either during pregnancy or post-partum period puts the mother’s health at danger.
In this study, the most identified infection prevention methods were washing perineum with warm water and some salt (70.0%) and changing pads frequently (36.4%). These findings are lower than those yielded in the study done in Nepal, in which 91.33% of PpM had prior knowledge of washing perineum with warm water and 83.16% changing pads frequently [ 3 ]. This discrepancy could be due to differences in the availability of health facilities and maternal training in the two study populations.
Around half (45.6%) of the postpartum mothers were aware about the appropriate time for restarting sexual intercourse in this study. However, it is difficult to say whether the postpartum mothers’ knowledge on this issue has been obtained through proper and methodical mechanisms, such as trainings and educational interventions, or from tradition. However, it is worth remembering that the scientific and traditional reason of commencing sexual intercourse after 6 weeks has the same ground. Lochia stays up to 6 weeks postpartum putting the mother at risk of postpartum infection and the pain as well as discomfort associated with the childbirth. Besides, the majority (87.6%) of participants in this study were Christians, and specifically belonged to the Orthodox Christian religion, where women are traditionally obliged to abstain from sexual intercourse for a minimum of 40 days because they are considered as polluted (tainted) after childbirth.
Worldwide, unwanted pregnancy is a major cause of death in children less than 5 years of age and a death of pregnant women attempting abortion (650 per100,000 pregnant women) each year [ 11 , 19 ]. Hence, a reliable contraceptive method is needed for mothers to avoid unwanted pregnancy as early as possible because menstruation period usually restarts at 3 to 9 weeks [ 11 ]. In the current study, knowledge of PpM on contraceptive methods shows that injectable contraceptives (92.7%) and oral contraceptives (91.5%) were highly mentioned. These findings are higher than the study done in Nepal that indicated injectable or Depo-Provera (78.0%) followed by oral contraceptive pills (74.0%) as the most common methods [ 20 ]. Therefore, it seems that maternal training and consultation about contraceptive methods in Eritrea is properly addressed and should be maintained.
In the present study, regarding knowledge of postpartum mothers on keeping baby warm after delivery, almost all participants (99.6%) had a higher knowledge when compared to a study conducted in Nepal which showed that 82% had knowledge on wrapping the baby with warm clothes. However, in this study, lower level of knowledge (6.8%) was scored on keeping baby warm by skin to skin contact than the study done in Nepal (58%) [ 21 ] .
Almost one-fourth of the PpM knew the correct answer for ‘when to give a bath to a newly born baby’ which is similar to a study conducted in India (30%) [ 22 ]. Around three-fourths of the postpartum mothers in the current study responded that umbilical cord is taken care of by simply keeping the umbilicus clean and dry. However, the study in Nepal showed that 59% were knowledgeable about keeping the umbilicus clean and dry [ 21 ]. The culture-driven beliefs and practices have also led 14.7% of the postpartum mothers in this study to indicate that butter is to be applied for umbilical care.
Health education provision by health workers at the health facilities and through the mass media could be the possible reason behind the correct knowledge (88.4%) of postpartum mothers regarding initiation of breastfeeding within 30 min. However, in a study done in Nepal, the percentage of mothers who mentioned that breastfeeding needs to be initiated within 1 hour was 48% [ 21 ]. Fever, as a new born danger sign, was identified by only 58.8% of the postpartum mothers in this study. This can be said to be relatively lower than the findings in Ethiopia (76.6%) [ 18 ] and Kenya (74.9%) [ 15 ]. Moreover, the difficulty of breathing as a baby danger sign was mentioned by almost half (50.8%) of the postpartum mothers. The same danger sign, was known by 46.6% of the participants in Kenyan study [ 15 ], whereas the current study finding was higher than that of Ethiopian study (19.7%) [ 14 ].
Results regarding new-born danger signs on umbilical cord problem (14, 5.4, 35%), convulsion (8.4, 19.3, 15%), and eye problem (6.8, 16.7, 21%) were not similar in this study, Ethiopia, and Nepal respectively [ 14 , 21 ]. Yellow palm as baby danger sign was the most highly unidentified (97.2%) by the postpartum mothers in this study, which is similar to the findings in Ghana (93.6%) [ 23 ]. However, inconsistent results on jaundice as baby danger sign were obtained in a study done in Nepal (21%) [ 21 ].
Comparison of the knowledge scores by categories of residence has revealed that urban residents had significantly greater knowledge score than the rural residents. The main reason for the difference could be the regularity in health education in urban places. Another possible reason could be the easy access to transport in urban places to go to the place where health education is offered. The lower level of knowledge among mothers who were in the age group 17 to 25, or primipara could be due to practical lessons that multipara mothers gain each time birth occurs.
Limitations of the study
The use of a cross sectional design in this study did not allow for causal relationships to be established, thus the reasons why postpartum mothers reported certain maternal and baby care more so than others is not known.
The average knowledge score on PNC of the postpartum mothers was low for it was below half of the overall score. Moreover, significant association between the mothers’ knowledge and their age group, residence, educational background, and parity was observed. Therefore, special attention should be given to mothers living in rural areas, junior or below in educational level, single or living together, primigravida/primipara, ethnic groups other than Tigrigna, and those between 17 to 25 years of age to improve PNC knowledge.
Availability of data and materials
Data set is available in electronic form which can be accessed upon a reasonable request from the corresponding author.
Abbreviations
Analysis Of Variance
Cesarean Section
Interquartile range
Post Natal Care
Postpartum Mothers
Standard Deviation
Statistical Package for Social Sciences
Spontaneous vaginal delivery
World Health Organization
World Health Organization. WHO recommendations on postnatal care of the mother and newborn. Geneva: World Health Organization; 2014.
FCM, Early Postpartum Care of the Mother and Infant and Transition to the Community.
Timilsina S, Dhakal R. Knowledge on postnatal care among postnatal mothers. Saudi J Med Pharm Pci. 2015;1:87–92.
Google Scholar
Shahraki AD, et al. World health report: make every mother and child count. J Med Sci. 2005;7(8):1066–74.
WHO. Postnatal care for mothers and newborns. Geneva: Highlights from the World Health Organization 2013 guidelines. RHR/15.05; 2015.
Warren C, et al. Postnatal care opportunities for Africa newborn. Oxford: Oxford University; 2005.
Alkema L, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN maternal mortality estimation inter-agency group. Lancet. 2016;387(10017):462–74.
Article Google Scholar
World Health Organization. Trends in Maternal Mortality: 1990 to 2015. Geneva: World Health Organization; 2015.
NSO. Eritrea Population and Health Survey 2010. Asmara: National statistics Offce and Fafo Institute for Appled; 2010.
Araya W, et al. Overview of maternal mortality in Eritrea, sub-Saharan Africa. Afr J Midwifery Womens Health. 2012;6(4):171–5.
Mirzaee K, Taghi Shakeri M. Maternal knowledge on postpartum care in healthcare centers of Mashhad, Iran in 2013. J Midwifery Reprod Health. 2015;3(4):456–64.
Sarkar J, Konwar G, Das LK. Assessment of knowledge and practice regarding postnatal exercises among mothers admitted in postnatal ward in Gauhati medical college and hospital. Obstet Gynaecol Barpeta. 2014;1(1):52–6.
Mohamadirizi S, Bahrami B, Moradi F. Comparison of the effect of electronic education and pamphlet on the knowledge of women about their post partum hygiene. J Nurs Educ. 2015;3(4):29–36.
Feyisso M, Addisu Y. Prabhanja danger signs of neonatal and postnatal illness and health seeking. J Curr Res. 2016;8(01):25466–71.
Kibaru EG, Otara AM. Knowledge of neonatal danger signs among mothers attending well baby clinic in Nakuru Central District, Kenya: cross sectional descriptive study. BMC Res Notes. 2016;9(1):481.
Mwilike B, et al. Knowledge of danger signs during pregnancy and subsequent healthcare seeking actions among women in urban Tanzania: a cross-sectional study. BMC Pregnancy Childbirth. 2018;18(1):4.
Fahey JO, Shenassa E. Understanding and meeting the needs of women in the postpartum period: the perinatal maternal health promotion model. J Midwifery Womens Health. 2013;58(6):613–21.
Bililign N, Mulatu T. Knowledge of obstetric danger signs and associated factors among reproductive age women in Raya kobo district of Ethiopia: a community based cross-sectional study. BMC Pregnancy Childbirth. 2017;17(1):70.
Zamani F, Rajabi Z. Unwanted pregnancy in rural women of Najafabad. KAUMS J (FEYZ). 2005;9(1):56–61.
Tuladhar H, Marahatta R. Awareness and practice of family planning methods in women attending gyne OPD at Nepal medical college teaching hospital. Nepal Med Coll J. 2008;10(3):184–91.
CAS PubMed Google Scholar
Shrestha T, Bhattarai SG, Silwal K. Knowledge and practice of postnatal mother in newborn care. J Nepal Med Assoc. 2013;52(190):372–7.
Rama R, Gopalakrishnan S, Udayshankar P. Assessment of knowledge regarding new-born care among mothers in Kancheepuram district, Tamil Nadu. Int J Commun Med Public Health. 2017;1(1):58–63.
Kuganab-Lem R, Yidana A. Exploring women knowledge of newborn danger signs: a case of mothers with under five children. Public Health Res. 2014;4(5):195–202.
Download references
Acknowledgments
We thank the staffs at the study areas for their assistance and collaboration. We would like also to express our heartfelt appreciation to the mothers who have participated in this study.
No funds were available.
Author information
Authors and affiliations.
Department of Nursing, Orotta College of Medicine and Health Sciences, Asmara, Eritrea
Ghirmay Ghebreigziabher Beraki, Amanuel Gebremichael, Berhanemeskel Yohannes, Kessete Haile, Shewit Tewelde & Simret Goitom
Department of Statistics, Biostatistics and Epidemiology Unit, College of Science, Eritrea Institute of Technology, Mai-Nefhi, Eritrea
Eyasu H. Tesfamariam
You can also search for this author in PubMed Google Scholar
Contributions
Each author contributed substantially to manuscript. GGB conceived, designed, wrote, analyzed and interpreted the manuscript. AG, BY, KH, ST, and SG collected the data and analyzed and wrote the first draft of the paper. EHT designed, analyzed and critically revised the manuscript for important intellectual content the final paper. All authors have read the manuscript for publication. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Ghirmay Ghebreigziabher Beraki .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from Asmara College of Health Sciences with a ref. No.: 019/09/17 and Eritrean Ministry of Health research and ethics committee with a ref. No.: 002/10/17. The participants’ rights were protected by ensuring voluntary participation and supported by written consent; after explaining the purpose, nature, potential benefits and risks of the study and data collection techniques. The anonymity and confidentiality of the participants were assured and treated as strictly confidential. Furthermore, they were given a full right to drop from participating in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Beraki, G.G., Tesfamariam, E.H., Gebremichael, A. et al. Knowledge on postnatal care among postpartum mothers during discharge in maternity hospitals in Asmara: a cross-sectional study. BMC Pregnancy Childbirth 20 , 17 (2020). https://doi.org/10.1186/s12884-019-2694-8
Download citation
Received : 21 August 2019
Accepted : 23 December 2019
Published : 06 January 2020
DOI : https://doi.org/10.1186/s12884-019-2694-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Postpartum mothers
- Postnatal care
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Research article
- Open access
- Published: 29 August 2018
Early postnatal home visits: a qualitative study of barriers and facilitators to achieving high coverage
- Yared Amare 1 ,
- Pauline Scheelbeek 2 ,
- Joanna Schellenberg 2 ,
- Della Berhanu 2 &
- Zelee Hill 3
BMC Public Health volume 18 , Article number: 1074 ( 2018 ) Cite this article
4878 Accesses
13 Citations
1 Altmetric
Metrics details
Timely interventions in the postnatal period are important for reducing newborn mortality, and early home visits to provide postnatal care are recommended. There has been limited success in achieving timely visits, and a better understanding of the realities of programmes is needed if improvements are to be made.
We explored barriers and facilitators to timely postnatal visits through 20 qualitative interviews and 16 focus group discussions with families and Health Extension Workers in four Ethiopian sites.
All sites reported some inaccessible areas that did not receive visits, but, Health Extension Workers in the sites with more difficult terrain were reported to make more visits that those in the more accessible areas. This suggests that information and work issues can be more important than moderate physical issues. The sites where visits were common had functioning mechanisms for alerting workers to a birth; these were not related to postnatal visits but to families informing Health Extension Workers of labour so they could call an ambulance. In the other sites, families did not know they should alert workers about a delivery, and other alert mechanisms were not functioning well. Competing activities reducing Health Extension Worker availability for visits, but in some areas workers were more organized in their division of their work and this facilitated visits. The main difference between the areas where visits were reported as common or uncommon was the general activity level of the Health Extension Worker. In the sites where workers were active and connected to the community visits occurred more often.
Conclusions
If timely postnatal home visits are to occur, CHWs need realistic catchment areas that reflect their workload. Inaccessible areas may need their own CHW. Good notification systems are essential, families will notify CHWs if they have a clear reasons to do so, and more work is needed on how to ensure notification systems function. Work ethic was a clear influencer on whether home visits occur, studies to date have focused on understanding the motivation of CHWs as a group, more studies on understanding motivation at an individual level are needed.
Peer Review reports
Approximately 2.9 million neonates die every year, which accounts for 44% of deaths among children under five years of age. 73% of these deaths are in the first week of life, and 36% on the first day [ 1 , 2 ]. This highlights the importance of timely intervention in this vulnerable period [ 2 ]. Several life saving newborn behaviours can be promoted, and interventions delivered, through early postnatal care (PNC). These include an assessment of the baby and treatment or referral, and counselling on breastfeeding, thermal care, hygiene, cord care and on danger signs [ 3 , 4 ].
Evidence shows that home visits by community health workers (CHWs) can be an effective means of delivering postnatal care in high mortality settings, and can reduce mortality [ 5 , 6 ], and this strategy has been adopted by 59 of the 75 countries in the Countdown to 2015 report [ 7 ]. Observational data suggest that these visits need to occur within 2 days of delivery to be effective [ 8 ]. The World Health Organization recommends that those who deliver at home should receive a home visit within 24 h of delivery, and those who deliver in a facility should receive PNC in the facility for the first 24 h and home visits from day three [ 3 ].
There have been mixed results in achieving timely visits. Data from sub-Saharan Africa show modest coverage of postnatal care home visits by CHWs, even in study and pilot program settings. In Malawi only 11% of women received a PNC visit within 3 days of delivery, in Tanzania only 15% within 2 days, in Uganda 26% received a visit on day 1, and in Ghana 38% received a visit on day 1 or 2 (figures calculated from authors data) [ 6 , 9 , 10 , 11 , 12 ]. Data from government programmes show even lower coverage levels [ 7 ]. Given the timing of newborn deaths and the importance of early visits, the need for research in this area has been acknowledged [ 13 ]. We identified only three quantitative studies exploring factors affecting the coverage of postnatal care home visits. A meta-analysis of quantitative data from Bangladesh, Malawi and Nepal found that early visits were more likely if a mother had been visited in pregnancy, if they had notified the CHW about the birth, and if the birth had been at home. In Ethiopia attending ANC, having more than two family meetings in pregnancy with a CHW, delivering with a CHW or skilled attendant, and having the CHW’s phone number were associated with receiving early home visits [ 14 ]. No association with maternal socio-demographic characteristics were found in any of the studies [ 10 , 11 , 14 ]. A program review that conducted qualitative interviews with government policy makers and technical specialists identified the need for a functioning primary health care system, a feasible PNC visit schedule, community demand, a functioning system to notify CHWs of a birth, and a cadre of CHWs who are qualified, motivated, have adequate time, access and transport [ 7 ]. We identified no qualitative studies at community level. Such research could provide evidence on why visits may, or may not, occur based on the experiences of the providers and beneficiaries. This paper reports the findings of a study, conducted in Ethiopia, on factors affecting early postnatal home visits by CHWs - Health Extension Workers. This is particularly timely as a Community Based Newborn Care program is currently being rolled out across the country, which includes early postnatal contacts to identify and manage neonatal sepsis at community level, and to provide counselling to families on newborn care [ 15 ].
Program description
The Health Extension Program was introduced in 2003, and has provided one year of training to over 30,000 female Health Extension Workers (HEW). Two salaried workers, educated to at least grade 10, are selected by local councils to serve an area of around 5000 people. They are stationed in health posts and are supported by a network of community volunteers, called the Health Development Army (HDA). HEWs provide health promotion, and disease prevention and treatment, both in the community and at the Health Post [ 16 , 17 , 18 ]. In 2009 a program to equip HEWs with the skills to provide essential newborn care was introduced, which included early post natal visits [ 19 ], and Community Based Newborn Care (CBNC) was added in 2014 including the identification and treatment of sepsis at community level.
Study setting selection and characteristics
The study was conducted in the Amhara and Southern Nations, Nationalities and Peoples (SNNP) regions of Ethiopia. The study was conducted in areas where the Health Extension Program, including CBNC activities, are supported by The Last Ten Kilometers programme (L10 K), a project implemented by JSI Research & Training Institute, Inc. In addition to routine HEW activities, L10 K has implemented a Community Based Data for Decision Making platform that includes tracking pregnant women, recording their service needs and linking them with the health system, and Family Conversations to promote key maternal and newborn health messages [ 20 , 21 , 22 , 23 ].
We were interested in understanding barriers and facilitators to early postnatal care within a reasonably functioning system, and L10 K provided us with a list of woreda (districts) and kebeles (lowest administrative units) that they considered had a functioning HEW and HDA system. From this list we selected two typical woreda in each region, and one kebele in each woreda that was reasonably accessible to the data collection team. We refer to the selected kebele s as kebele “A-D” to maintain anonymity. Table 1 shows the characteristics of the selected kebeles , all of which had a predominantly subsistence farming based economy. There were no reports of the use of the private sector by any study participants and we did not identify any private providers of PNC in the study areas.
Data collection
Data were collected from end of March, 2015 to May, 2015. Ethical approval was gained from the research ethics committees of the London School of Hygiene and Tropical Medicine, and from the Ministry of Science and Technology in Ethiopia. Written informed consent was obtained from all respondents. Data were collected using pre-tested semi structured guides developed by the authors. Data were collected as part of a wider study on the mechanisms of behaviour change related to key maternal and newborn care practices.
Data were collected from recent mothers, grandmothers, fathers, HEWs and HDA members using narrative and in-depth interviews, friendship pair interviews and focus group discussions. Collecting data from several respondent groups, and using a range of methods, ensured we captured a range of views and allowed for data triangulation. Sample sizes, respondent groups, the rationale for using each method, and the content related to early PNC visits are shown in Table 2 . Sample sizes were based on prior experience of when saturation was likely to be reached. The possibility of conducting additional interviews and FGDs was built into the data collection plan in case saturation was not reached as anticipated.
The recent mothers and grandmothers were identified with the assistance of HEWs and HDAs and through snowball sampling. They were eligible for inclusion if they, or their daughter/daughter in law, received at least one home visit by an HEW or HDA in the ante or postnatal period. Recent mothers were purposively selected to ensure a range of ages, educational levels, parities, sex of newborn and socio-economic status that reflected the variation within the study site. For example, less than 14% of women in the study regions had secondary school education [ 24 ], and our purposive sampling focused on women with no or primary education. Place of delivery was also set as a selection criteria but it proved difficult to get many respondents who delivered at home. Fathers were recruited through the local authorities or through the HEWs and HDAs. All HDAs in a kebele were invited for the HDA FGDs. As there were only 2 HEWs per kebele , HEWs from neighbouring health posts were invited to the HEW FGDs. Selected respondents were approached in their home or place of work by the interviewers who explained the study, answered questions and took consent. Three participants refused: one wanted to attend a funeral, and the other two were too busy with their household chores to be able to participate.
Data were collected by four trained interviewers in the local language, with translators used in SNNPR. Interviews lasted from 1 to 2 h and took place in respondents’ houses. FGDs consisted of 3–7 participants and lasted from 1.5 to 2.5 h. They were conducted in neutral locations such as community centres. Interviews and FGDs were audio-recorded and fully transcribed in English within a week of data collection. During data collection, interviewers received regular feedback from senior researchers on their transcripts, interview techniques and to discuss emerging themes. The research team met twice during data collection to ‘pre-analyse’ the data in-order to document emerging themes and identify areas that needed to be explored in subsequent interviews and focus groups and to determine if saturation had been reached.
Data analysis
We conducted a thematic analysis, this consisted of multiple readings of the postnatal care sections of the transcripts to ensure familiarity with the data, to get an understanding of the data as a whole, to begin to identify recurring ideas, and core, a-typical or notable ideas, − these were captured in reflective notes. General themes were derived deductively from the research aims, these were: Timing and content of PNC visits, reactions to PNC visits, and factors influencing the occurrence of visits. Analysis for the timing of, content and reaction to PNC was semantic/descriptive, while coding for factors influencing the occurrence of visits included examining the data for latent constructs. Interviews and focus groups were coded within the broad themes using NVIVO. Coding consisted of reading each transcript and identifying the underlying meaning of each segment of text. For each segment we considered what the segment was about, what message it was giving, what stuck out, and how it was different or similar to others segments, each segment was then given one or more code related to its underlying meaning. Codes that contained similar concepts were sorted and placed into themes. Themes and codes were refined and adjusted by looking for patterns, links and contradictions within themes. Data credibility was checked by triangulating data between respondent groups and between data collection methods. Data analysis was done by two of the senior researchers who discussed their coding regularly to enhance conceptual thinking and increased coding rigor.
There was considerable variability in the reported occurrence and timing of post-natal care (PNC) visits by HEW among the four study kebele . Respondents from all respondent groups consistently reported that HEWs in kebele A and B in Amhara visit most mothers within 3 days of giving birth. But the replacement of two longstanding HEWs by temporary workers in kebele B was reported to have led to a recent decline in visits. Visits were reported as occurring late or not at all in kebele C in SNNPR, and were said to be largely non-existent in kebele D in SNNPR. Reflecting their reportedly frequent occurrence, PNC visits in the Amhara kebeles were described as ‘ordinary’, while in kebele D respondents had ‘never heard’ of this type of visit.
Through our inductive coding three main interlinked themes related to why early PNC visit may or may not occur emerged. These were physical issues related to accessibility and transport issues; information issues related to whether the HEW knew about the delivery; and work issues related to HEW availability, HEW performance and organization. We found no pattern in relation to PNC visits and maternal education level, with nearly all of the mothers interviewed having no or primary education levels.
Physical issues
The main physical barriers to early PNC visits were related to accessibility (distance, spread of villages and topography) and to transport. In all study areas, there were households that were classed as inaccessible by all participants due to time or terrain issues. For example, in kebele A, there were some areas that were accessible only by ladders or only in the dry season, and these were difficult for the HEWs to visit:
‘Some of the places are quite mountainous, and other places can only be accessed using a ladder to descend a ravine….There are places that we can’t access in the wet season…. Those that are nearer are not problematic. We get them within 24 hours’ [ kebele A, Amhara, HEW – FGD].
Generally a flat topography and clustered settlements were seen to facilitate visits and a hilly terrain and scattered settlements were seen as a barrier. A flat terrain meant that households were generally accessible by transportation, which was facilitated by the few HEWs that had bicycles: ‘The topography of this kebele is flat like …. no ups and downs It is accessible for cars and walking’ [ kebele D, SNNPR, Fathers – FGD].
Although extreme distances and terrains were limiting factors for PNC visits, moderate difficulties were not a limiting factor. Kebele A and B had the most difficult terrain overall, but these kebele are where community members reported that early PNC visits were most common. In contrast kebele D was generally flat and accessible but PNC visits were reported by community members as not occurring at all suggesting that information and work issues can be more important barriers than moderate physical difficulties.
Information issues
Whether the HEWs’ knew a birth had occurred was a key theme in whether early PNC visits occurred. The main sub-themes were whether there was a functioning alert mechanism; and minor sub themes were place of delivery, migration in pregnancy and whether the pregnancy carried any stigma.
In the Amhara kebeles (A and B), where visits were reported as being common, mothers reported that HEWs knew they had delivered because they were involved in the delivery or in calling the ambulance. Women in these kebeles reported that they were told to inform the HEW when they went into labor, and few women had the ambulance number themselves: ‘ I directly went to their office [health post] when I felt labor pain, and it is the HEWs who called for Ambulance services’ [ kebele A, Amhara, mother-narrative]. In the difficult to access areas of these kebeles , HEWs reported that they relied on the HDAs informing them of the delivery, which was hampered by accessibility issues as HDAs went in person or sent a messenger to inform an HEW of a delivery:
‘The problem is that we do not get the feedback through the HDAs on time. They have to go a lot of distance and they sometimes send the feedback through students…….because of that we visit them after 7 days. So that is our major problem’ [ kebele A Amhara, HEW-FGD].
In the SNNP kebeles (C and D), where PNC visits were reported as occurring late or not at all, women were given the ambulance number directly, often by the HDA. The HEWs thus relied on the HDA leaders informing them that a woman had given birth, and this did not always occur. In particular, HDAs in kebele D (where PNC visits were rare) reported that they did not always tell the HEWs about a delivery ‘The problem may be with us [HDA].….for example there was a mother that had delivered; I did go and visit her but I have not come and tell the HEW about it’ [ kebele D, SNNPR, HDA – FGD]. This lack of provision of information was not linked to a lack of HDA activity, which was high in these kebele . Instead, there were some reports that the HDAs were tasked by the HEWs to conduct their visits and did not see any benefit of informing them of a delivery.
Other means of identifying delivered women were using the expected date of delivery, word of mouth and being informed by the family. Using the expected date of delivery was reported as problematic as the date were not accurate, and word of mouth was only useful where HEWs were very active in the community and made regular visits. In kebele A, in Amhara, and kebele C, in SNNPR, HEWs reported that the women themselves were meant to inform the HEW of the delivery, but mothers did not know that they should inform the HEW, and this mechanism was not functioning.
At the time of the study, few women in the study Kebles reported delivering at home, with major efforts from HEWs and HDAs to ensure all women delivered in a facility. Delivering at home was reported as shameful, with threats of sanctions and a fear that the HEW and HDA would be angry. Respondents from the mother, father and HEW/HDA FGDs all reported that HEWs would not know about women who delivered at home ‘If a woman gives birth at home, the HEWs won’t hear about it. Nobody tells them that she has given birth’ [ kebele A, Amhara, Mother – FGD]. In the few cases we found where the HEWs knew about a home delivery, the women felt that they were denied PNC visits as a sanction for not delivering at a facility or not attending ANC, and this was reiterated in a mothers in the FGDs: ‘ If she [mother] refused and decided to stay at home, they [HEW] will never visit her and she just sit at her house alone….they won’t be at her side [kebele A, Amhara, Mother- FGD]. In general attending ANC was a proactive decision by the family, while the families’ roles in receiving PNC visits was passive, with no active care seeking decisions in relation to the home visits. We found no pattern or link between attending ANC and receiving a PNC visit.
Other minor themes related to HEWs being unaware of deliveries, that were reported in the HEW/HDA FGDs, were that some first time mothers travel to their own mother in another kebele to deliver, and that unmarried ‘teenagers’ keep their pregnancies and deliveries secret due to the stigma attached to them.
Work issues
Two main sub themes related to work issues that affected whether timely PNC visits were made were: HEW availability and HEW work ethic and organization. Mothers, HEWs and HDAs reported workload and HEW availability as barriers to making timely PNC visits. Issues included being unavailable for visits as they were escorting women for delivery, multiple women delivering in different locations at the same time, staff absences, and participation in training workshops, meetings and health campaigns: ‘There are only two HEWs. They have lots of activities, which they are expected to perform. Therefore, they cannot cover all mothers in the three days after delivery’ [ kebele C, SNNPR, Mother – FGD]. Some HEWs were more organized in terms of dividing up the community and having a clear plan for visiting communities, and these plans facilitated early visits.
Differences in HEW work ethic was also identified as a reason for no or late PNC visits, and the main differences between the kebele with reported high and low levels of early PNC visits was the general level of activity of the HEWs. In kebeles with low PNC visits HEWs were reported as only coming to the community for vaccinations, being rarely at the health post, or rarely leaving the health post: ‘They [HEWs] spend the whole day here [at health post] but no one come to here…..they didn’t go inside the village’ [ kebele D, SNNPR, Father - FGD]. Temporary HEWs were reported as having particular issues with poor links with the community and with the HDA. This translated into few PNC visits being made: ‘Such staff [temporary] have a feeling that they will not be there in the kebele for long and show some sort of reluctance. They will not take their job … they believe that another person will take over from them very soon’ [ kebele A, Amhara, HEW – FGD]. In kebeles with low PNC coverage the HEWs sometimes relied on strong HDA teams to conduct activities, or were reported as only being interested in ensuring facility deliveries occurred.
In contrast, in those kebeles with reported high PNC coverage, community members described a general high level of HEW activity and a sense of connectedness between the community and the HEW:
‘ They themselves live with us. They are with us when the baby is delivered. They visit us every day. They do not do only visiting within three days. They call for Ambulance; they escort us to the health facility and assist us in delivery’ [ kebele B, Amhara, Mother - FGD].
Home visits by community health workers to provide postnatal care have the potential to reduce newborn mortality [ 5 , 6 ], but observational data suggest that these need to occur within 24 h to be effective [ 8 ]. Despite the importance of PNC visits, achieving early visits in sub Saharan African settings has proved difficult [ 6 , 9 , 10 , 11 , 25 ], and there has been little research on why early visits are not achieved. We found that visits were affected by three inter-linked issues: physical issues (accessibility and transport), information issues (whether the HEW knows about the delivery), and work issues (HEW availability and performance).
Accessibility as a barrier to CHW performance has been found in several settings [ 26 ], and there were areas in all the study sites that were inaccessible due to topography or distance constraints. We found that moderate accessibility issues were not barriers to early visits if HEWs were active, organized and well connected to the community. Care should be taken when demarcating work areas to exclude areas that are unreachable; such areas may require their own CHW for timely visits to occur. The demarcation of small and realistic catchment areas was hypothesized as a reason why Village Health Workers (VHW) in a study in Bangladesh achieved a coverage of early home visits of 87% [ 13 ].
Knowing that a delivery has occurred was essential for HEWs making a timely PNC visit, and no or late notification of a delivery has been identified as a barrier to early home visits in other settings [ 8 , 10 , 13 ]. In the study areas formal notification strategies existed through HDAs informing HEWs of a delivery, although this did not always occur despite the existence of enhanced tracking of pregnant women through L10Ks’ Community Based Data for Decision Making platform. Timely notification by HDAs was hindered by distance, and HDAs did not report using mobile phones for notification. Providing mobile phones or air time could improve notification rates, with an association between having the HEWs phone number and receiving an early PNC visit found in a previous Ethiopian study [ 14 ]. Evidence suggests that using mobile phones to increase communication is highly valued by CHWs because it reduces travel time and enhances efficiency [ 27 ], however, this may be difficult where mobile phone coverage levels are low.
In two of the study kebeles families notified the HEWs directly when they went into labour, and HEWs played an active role in calling an ambulance or assisting with the delivery. This demonstrates that when families are aware of the need to notify a HEW, and have a reason to do so, then they are able and willing to do this. Our study suggests that family led notification, especially if done in labor, may result in earlier PNC visits than HDA led notification. Family led notification is likely to be enhanced by HEWs making pregnancy visits, especially if family members are included [ 10 , 14 ], as this may improve links between the HEW and the family, and helps ensure that families know their role in notification. Facilities did not play a role in the notification process in the study kebeles . As rates of facility delivery increase facilities could play an important role in notification, particularly for newborns identified as high risk who may benefit most from early visits. The passive role that families currently play in PNC home visits may explain why we saw no pattern in visits by education levels, mirroring the lack of association between socio demographic characteristics and PNC visits found in other studies [ 10 , 11 , 14 ].
Issues with HEW availability were also reported as affecting PNC coverage, with competing tasks meaning that HEWs were not always available for timely visits. Such factors are largely out of control of the HEWs, and care needs to be taken to ensure that CHW tasks are feasible and take into account travel time. There was some evidence that HEWs and HDAs were focusing on facility deliveries to the detriment of their other activities.
The greatest difference between kebeles with high and low PNC coverage was the general activity level of the HEW. This affected notification issues and was more important than moderate physical barriers. In some kebeles , HEWs were reported as rarely coming to the community or relying on active HDAs to perform tasks, whilst in others they were reported as making frequent visits and were clearly well connected to the community. There was a particular problem with temporary workers. The role of motivation in performance is well recognized and numerous studies have reported on general motivators of CHWs. Few studies have explored variability in motivation across areas, nor the role of contextual issues, although these appear to be important [ 26 ]. We identified only one study that aims to rigorously evaluate methods of improving CHW motivation: the results of this study are yet to be reported and more research is needed [ 28 ].
We found little evidence of socio-cultural barriers from the community side for early visits, except that home delivery may be a barrier for notifying HEWs for fear for sanctions, and that some first time mothers travel to their home community for delivery. The use of sanctions for those who deliver at home may lead to vulnerable families not receiving vital services. There is much attention now being paid to the disrespect and abuse of women in facilities [ 29 , 30 ]: there is also the potential for this to occur during home visits.
During this study we took several steps to maximize data quality and data transferability such as the use of multiple study sites, methods and respondent groups; the use of methods that aimed to overcome social desirability bias; purposive sampling to saturation; regular meetings and feedback during data collection to enhance reflective thinking; triangulation of data and team analysis. Despite this there is the potential for reporting and recall bias. Data were collected from small geographic areas that were accessible to the study teams and had reasonably functioning HEW systems, the findings may not apply to other areas with significantly different contextual issues, however the study findings suggest several issues that could be explored and considered when exploring issues related to PNC coverage in other settings. Studies in other settings in Ethiopia would further enhance transferability.
If timely postnatal home visits are to occur, programs need to ensure that CHWs have realistic catchment areas that reflect their workload. Inaccessible areas may need their own CHW. Good notification systems are essential, families will notify CHWs if they have a clear reasons to do so, and more work is needed on how to ensure other potential notification systems function. Work ethic was a clear influencer on whether home visits occur, studies to date have tended to explore the motivation of CHWs as a group rather than exploring differences between CHWs, more studies on understanding motivation at an individual level are needed.
Darmstadt GL, Kinney MV, Chopra M, Cousens S, Kak L, Paul VK, et al. Who has been caring for the baby? Lancet. 2014;384(9938):174–88.
Article PubMed Google Scholar
Lawn JE, Blencowe H, Oza S, You D, Lee AC, Waiswa P, et al. Every newborn: progress, priorities, and potential beyond survival. Lancet. 2014;384(9938):189–205.
World Health Organization. WHO recommendations on postnatal care of the mother and newborn. Geneva: World Health Organization; 2013. Report No.: 978 92 4 150664 9
Google Scholar
World Health Organization and UNICEF. Home visits for the newborn child: a strategy to improve survival. Geneva: World Health Organization and UNICEF; 2009.
Gogia S, Sachdev HS. Home visits by community health workers to prevent neonatal deaths in developing countries: a systematic review. Bull World Health Organ. 2010;88(9):658–666B.
Article PubMed PubMed Central Google Scholar
Kirkwood BR, Manu A, ten Asbroek AH, Soremekun S, Weobong B, Gyan T, et al. Effect of the Newhints home-visits intervention on neonatal mortality rate and care practices in Ghana: a cluster randomised controlled trial. Lancet. 2013;381(9884):2184–92.
McPherson R, Hodgins S. Postnatal home visitation: lessons from country programs operating at scale. J Glob Health. 2018;8(1):010422.
Baqui AH, Ahmed S, El Arifeen S, Darmstadt GL, Rosecrans AM, Mannan I, et al. Effect of timing of first postnatal care home visit on neonatal mortality in Bangladesh: a observational cohort study. BMJ. 2009;339:b2826.
Waiswa P, Pariyo G, Kallander K, Akuze J, Namazzi G, Ekirapa-Kiracho E, et al. Effect of the Uganda newborn study on care-seeking and care practices: a cluster-randomised controlled trial. Glob Health Action. 2015;8:24584.
Sitrin D, Guenther T, Murray J, Pilgrim N, Rubayet S, Ligowe R, et al. Reaching mothers and babies with early postnatal home visits: the implementation realities of achieving high coverage in large-scale programs. PLoS One. 2013;8(7):e68930.
Article PubMed PubMed Central CAS Google Scholar
Callaghan-Koru JA, Nonyane BA, Guenther T, Sitrin D, Ligowe R, Chimbalanga E, et al. Contribution of community-based newborn health promotion to reducing inequities in healthy newborn care practices and knowledge: evidence of improvement from a three-district pilot program in Malawi. BMC Public Health. 2013;13:1052.
Hanson C, Manzi F, Mkumbo E, Shirima K, Penfold S, Hill Z, et al. Effectiveness of a home-based counselling strategy on neonatal care and survival: a cluster-randomised trial in six districts of rural southern Tanzania. PLoS Med. 2015;12(9):e1001881.
Shah R, Munos MK, Winch PJ, Mullany LC, Mannan I, Rahman SM, et al. Community-based health workers achieve high coverage in neonatal intervention trials: a case study from Sylhet. Bangladesh J Health Popul Nutr. 2010;28(6):610–8.
PubMed Google Scholar
Tesfaye S, Barry D, Gobezayehu AG, Frew AH, Stover KE, Tessema H, et al. Improving coverage of postnatal care in rural Ethiopia using a community-based, collaborative quality improvement approach. J Midwifery Womens Health. 2014;59(Suppl 1):S55–64.
The Last Ten Kilometers. Community based newborn care. In: Kilometers TLT, editor. News from the last ten kilometers. Addis Ababa: The Last Ten Kilometers; 2014.
Banteyerga H. Ethiopia's health extension program: improving health through community involvement. MEDICC Rev. 2011;13(3):46–9.
Koblinsky M, Tain F, Gaym A, Karim A, Carnell M, Tesfaye S. Responding to the maternal health care challenge: The Ethiopian Health Extension Program. Ethiop J Health Dev. 2010;24(Special Issue 1):105–9.
Legesse H, Degefie T, Hiluf M, Sime K, Tesfaye C, Abebe H, et al. National scale-up of integrated community case management in rural Ethiopia: implementation and early lessons learned. Ethiop Med J. 2014;52(Suppl 3):15–26.
Karim AM, Admassu K, Schellenberg J, Alemu H, Getachew N, Ameha A, et al. Effect of ethiopia’s health extension program on maternal and newborn health care practices in 101 rural districts: a dose-response study. PLoS One. 2013;8(6):e65160.
The Last Ten Kilometers. Improving maternal and newborn health care practices. The role of community based data for decision making in: kilometers TLT, editor. News from the last ten kilometers. The Last Ten Kilometers: Addis Ababa; 2013.
Betemariam B, Karim A, Getachew N. Evidence based scaling-up an innovative community-based maternal and newborn health strategy in Ethiopia. In: 141st American Public Health Assocition annual meeting. Boston, USA; 2013.
Darmstadt GL, Marchant T, Claeson M, Brown W, Morris S, Donnay F, et al. A strategy for reducing maternal and newborn deaths by 2015 and beyond. BMC Pregnancy Childbirth. 2013;13:216.
Karim A. Effectiveness evaluation of a large-scale community-based program: Lessons from Ethiopia. Annals of Global Health. 2015;81(1):192.
Article Google Scholar
Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland: CSA and ICF. p. 2016.
Penfold S, Manzi F, Mkumbo E, Temu S, Jaribu J, Shamba DD, et al. Effect of home-based counselling on newborn care practices in southern Tanzania one year after implementation: a cluster-randomised controlled trial. BMC Pediatr. 2014;14:187.
Kok MC, Kane SS, Tulloch O, Ormel H, Theobald S, Dieleman M, et al. How does context influence performance of community health workers in low- and middle-income countries? Evidence from the Literature Health Res Policy Syst. 2015;13:13.
Thondoo M, Strachan DL, Nakirunda M, Ndima S, Muiambo A, Kallander K, et al. Potential roles of Mhealth for community health workers: formative research with end users in Uganda and Mozambique. JMIR Mhealth Uhealth. 2015;3(3):e76.
Kallander K, Strachan D, Soremekun S, Hill Z, Lingam R, Tibenderana J, et al. Evaluating the effect of innovative motivation and supervision approaches on community health worker performance and retention in Uganda and Mozambique: study protocol for a randomised controlled trial. Trials. 2015;16:157.
Bohren MA, Vogel JP, Hunter EC, Lutsiv O, Makh SK, Souza JP, et al. The Mistreatment of Women during Childbirth in Health Facilities Globally: A Mixed-Methods Systematic Review. PLoS Med 2015;12(6):e1001847; discussion e1001847.
Freedman LP, Kruk ME. Disrespect and abuse of women in childbirth: challenging the global quality and accountability agendas. Lancet. 2014;384(9948):e42–4.
Download references
The study was funded by the Bill and Melinda Gates foundation as part of the IDEAS study.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available due to issues of confidentiality and privacy. Although respondents’ names are not included in transcripts they do include place names and any names mentioned by respondents, for example, names of Health Extension Workers.
Author information
Authors and affiliations.
Consultancy for Social Development, PO Box 70196, Addis Ababa, Ethiopia
Yared Amare
London School of Hygiene and Tropical Medicine, Keppel Street, London, WC1E 7HT, UK
Pauline Scheelbeek, Joanna Schellenberg & Della Berhanu
University College London, 30 Guilford Street, London, WC1N 1EH, UK
You can also search for this author in PubMed Google Scholar
Contributions
ZH and JS conceived the study; ZH, YA and PA designed the study and the data collection tools. YA, PA and DB were responsible for the acquisition of data. ZH, PS and YA were responsible for analysing and interpreting the data. ZH and YA prepared the first draft of the paper and all authors commented on the paper and approved the final version.
Corresponding author
Correspondence to Zelee Hill .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was obtained from the Institutional Review Boards of the London School of Hygiene and Tropical Medicine and the Ministry of Science and Technology in Ethiopia. Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Amare, Y., Scheelbeek, P., Schellenberg, J. et al. Early postnatal home visits: a qualitative study of barriers and facilitators to achieving high coverage. BMC Public Health 18 , 1074 (2018). https://doi.org/10.1186/s12889-018-5922-7
Download citation
Received : 29 August 2017
Accepted : 01 August 2018
Published : 29 August 2018
DOI : https://doi.org/10.1186/s12889-018-5922-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Community health worker
- Qualitative
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]

- Copy/Paste Link Link Copied
What is prenatal care and why is it important?
Having a healthy pregnancy is one of the best ways to promote a healthy birth. Getting early and regular prenatal care improves the chances of a healthy pregnancy. This care can begin even before pregnancy with a pre-pregnancy care visit to a health care provider.
Pre-Pregnancy Care
A pre-pregnancy care visit can help women take steps toward a healthy pregnancy before they even get pregnant. Women can help to promote a healthy pregnancy and birth of a healthy baby by taking the following steps before they become pregnant: 1
- Develop a plan for their reproductive life.
- Increase their daily intake of folic acid (one of the B vitamins) to at least 400 micrograms. 2
- Make sure their immunizations are up to date.
- Control diabetes and other medical conditions.
- Avoid smoking, drinking alcohol, and using drugs.
- Attain a healthy weight.
- Learn about their family health history and that of their partner.
- Seek help for depression, anxiety, or other mental health issues.
Prenatal Care
Women who suspect they may be pregnant should schedule a visit to their health care provider to begin prenatal care. Prenatal visits to a health care provider usually include a physical exam, weight checks, and providing a urine sample. Depending on the stage of the pregnancy, health care providers may also do blood tests and imaging tests, such as ultrasound exams. These visits also include discussions about the mother's health, the fetus's health, and any questions about the pregnancy. 3
Pre-Pregnancy and prenatal care can help prevent complications and inform women about important steps they can take to protect their infant and ensure a healthy pregnancy. With regular prenatal care women can:
- Reduce the risk of pregnancy complications. Following a healthy, safe diet; getting regular exercise as advised by a health care provider; and avoiding exposure to potentially harmful substances such as lead and radiation can help reduce the risk for problems during pregnancy and promote fetal health and development. 4 Controlling existing conditions, such as high blood pressure and diabetes, is important to prevent serious complications and their effects. 5
- Reduce the fetus's and infant's risk for complications. Tobacco smoke and alcohol use during pregnancy have been shown to increase the risk for Sudden Infant Death Syndrome . 6 Alcohol use also increases the risk for fetal alcohol spectrum disorders, which can cause a variety of problems such as abnormal facial features, having a small head, poor coordination, poor memory, intellectual disability, and problems with the heart, kidneys, or bones. 7 According to one recent study supported by the NIH, these and other long-term problems can occur even with low levels of prenatal alcohol exposure. 8 In addition, taking 400 micrograms of folic acid daily reduces the risk for neural tube defects by 70%. 2 , 9 Most prenatal vitamins contain the recommended 400 micrograms of folic acid as well as other vitamins that pregnant women and their developing fetus need. 1 , 10 Folic acid has been added to foods like cereals, breads, pasta, and other grain-based foods. Although a related form (called folate) is present in orange juice and leafy, green vegetables (such as kale and spinach), folate is not absorbed as well as folic acid.
- Help ensure the medications women take are safe. Women should not take certain medications , including some acne treatments 11 and dietary and herbal supplements, 12 during pregnancy because they can harm the fetus.
Learn more about prenatal and pre-pregnancy care .
- Centers for Disease Control and Prevention. (2015). Preconception health and health care. Retrieved May 20, 2016, from http://www.cdc.gov/preconception/planning.html
- Centers for Disease Control and Prevention. (2011). Fetal alcohol spectrum disorders. Retrieved August 1, 2012, from http://www.cdc.gov/Features/FASD
- Eckstrand, K. L., Ding, Z., Dodge, N. C., Cowan, R. L., Jacobson, J. L., Jacobson, S. W., et al. (2012). Persistent dose-dependent changes in brain structure in young adults with low-to-moderate alcohol exposure in utero. Alcoholism: Clinical and Experimental Research, 36 (11), 1892–1902. PMID: 22594302
- Centers for Disease Control and Prevention. (2016). Folic acid. Data and statistics. Retrieved December 12, 2016, from https://www.cdc.gov/ncbddd/folicacid/data.html
- NIH Office of Dietary Supplements. (2016). Folate. Dietary supplement fact sheet. Retrieved May 20, 2016, from http://ods.od.nih.gov/factsheets/Folate-HealthProfessional
- Office on Women's Health. (2012). Prenatal care fact sheet. Retrieved May 20, 2016, from http://www.womenshealth.gov/publications/our-publications/fact-sheet/prenatal-care.html
Courses on Sexual and Reproductive Health and Research 2021 Geneva Foundation for Medical Education and Research
- Weekly schedule
- Participants
- Course files
- Assignments
- Course evaluation report
- General information
- Application form
- Course guide
- Assignment guide
- Web statistics
- End of course meeting
Antenatal, intrapartum and postnatal care
Training course in adolescent sexual and reproductive health 2021 for WHO Eastern Mediterranean Region
February 8, 2021 - Geneva
Assignment (25 marks in total)
Answer the following questions using the clues provided to review the selected aspects of the relevant documents.
Global reading – 1
United Nations Population Fund (UNFPA). Not on pause: Responding to the sexual and reproductive health needs of adolescents in the context of the COVID-19 CRISIS - Technical Brief. UNFPA; 2020 Jun.
Question 1 (5 marks)
1.1 Identify three actions that could be taken to ensure that adolescents have access to antenatal care, intrapartum care and postnatal care in the context of disruptions to service provisions due to COVID-19.
Clue: Refer to page 10 of “Not on pause: Responding to the SRH needs of adolescents in the context of the COVID-19 crisis”. (3 marks)
1.2 Were there disruptions to maternal health services in your country due to COVID-19? If so, what were the consequences. Please back up your answers with references, where possible.
Clue: Refer to “Not on pause: Responding to the SRH needs of adolescents in the context of the COVID-19 crisis” and provide references and relevant data sources. (2 marks)
Global reading – 2
Bohren MA, Mehrtash H, Fawole B, et al. How women are treated during facility-based childbirth in four countries: a cross-sectional study with labour observations and community-based surveys. The Lancet. 2019 Nov 9;394(10210):1750-63.
Question 2 (5 marks)
2.1 What were the two primary determinants of mistreatment during childbirth in the four-country study reported in the article titled: “How women are treated during facility-based childbirth in four countries: a cross-sectional study with labour observations and community-based surveys”?
Clue: Refer to the summary of the article, page 1750. (2 marks)
2.2 Why do you believe that girls/young women and those with less education were more affected by mistreatment?
Clue: Provide references and relevant used data sources. (3 marks)
Global reading – 3
WHO. Companion of choice during labour and childbirth for improved quality of care – Evidence-to-action brief. World Health Organization; 2020.
Question 3 (5 marks)
3.1 What are the proven clinical benefits of labour companionship?
Clue: Refer to page 2 of the document titled: “Companion of choice during labour and childbirth for improved quality of care”. (3 marks)
3.2. What were the three principal findings of the research study in three public tertiary hospitals in Egypt, Lebanon and the Syrian Arab Republic on labour companionship in each of these contexts?
Clue: Refer to page 5 of the document titled: “Companion of choice during labour and childbirth for improved quality of care”. (2 marks)
Regional reading – 1
Mahaini R. Improving maternal health to achieve the Millennium Development Goals in the Eastern Mediterranean Region: a youth lens. East Mediterr Health J. 2008;14 Suppl:S97-106.
Question 4 (5 marks)
4.1 Identify three ‘delays’ that contribute to high maternal and infant mortality in the Eastern Mediterranean region.
Clue: Refer to page 101, Situation analysis of youth reproductive health in the region, “Improving maternal health to achieve the Millennium Development Goals in the Eastern Mediterranean Region: a youth lens” (Mahaini, 2008). (3 marks)
4.2 Identify two priorities for improving maternal healthcare - with a focus on adolescents - in your country.
Clue: Refer to “Improving maternal health to achieve the Millennium Development Goals in the Eastern Mediterranean Region: a youth lens” (Mahaini, 2008). (2 marks)
Regional reading – 2
Moridi M, Shokravi FA, Ahmadi F. The paradox of acceptance: A content analysis of Iranian married female adolescent in confronting pregnancy. PLOS ONE. 2019 May 10;14(5):e0216649.
Question 5 (5 marks)
5.1 Based on the study’s findings, identify two reasons that young Iranian women accepted a pregnancy even if they were not ready for it?
Clue: Refer to page 7-8, Passive acceptance of pregnancy, “The paradox of acceptance: A content analysis of Iranian married female adolescent in confronting pregnancy” (Moridi, Shokravi and Ahmadi, 2019). (2 marks)
5.2. Based on the study’s findings, identify two causes for the frustration and regret the young pregnant Iranian women who were studied felt.
Clue: Refer to page 9-10, Frustration and regret, “The paradox of acceptance: A content analysis of Iranian married female adolescent in confronting pregnancy” (Moridi, Shokravi and Ahmadi, 2019). (2 marks)
5.3 Name one thought that came to your mind when you read this study. (1 mark)

- Review Assignment
- Announcements
- About the Course
- Explore Courses
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care : Result Published!!
- Log in to your account and navigate to the "Download E-certificate" section.
- Next to "Download E-certificate," you'll find another tab labeled "Share your experience." Click on it.
- Answer the provided questions about your experience.
- Optionally, you can add your picture or skip this step.
- An AI-assisted post will be generated for you. You can share this post on your social media platforms.
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care : Final Feedback Form !!!
Dear students, We are glad that you have attended the NPTEL online certification course. We hope you found the NPTEL Online course useful and have started using NPTEL extensively. In this regard, we would like to have feedback from you regarding our course and whether there are any improvements, you would like to suggest. We are enclosing an online feedback form and would request you to spare some of your valuable time to input your observations. Your esteemed input will help us in serving you better. The link to give your feedback is: https://docs.google.com/forms/d/1qnJXV7T5yROopwC4D_rYiXb6YP98hAHyVkzXo2M8GEY/viewform We thank you for your valuable time and feedback. Thanks & Regards, -NPTEL Team
April 2024 NPTEL Exams - Hall Tickets Released!
.jpg)
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Assignment-9,10,11& 12. Solution Released
Dear Participants,
The Assignment- 9,10,11& 12. of Week- 9,10,11& 12. Solution for the course An Overview on Maternal Health Antenatal,Intranatal and Postnatal Care has been released in the portal. Please go through the solution and in case of any doubt post your queries in the forum.
Solution 9 : Link: https://drive.google.com/file/d/1lQburXGfVdz4OvNYvBQfBdcJISzlJ_A1/view?usp=sharing Solution 10 : Link: https://drive.google.com/file/d/1F2UUrfySeE7RATKhkZnwBKYzi2Y0JHKQ/view?usp=sharing Solution 11 : Link: https://drive.google.com/file/d/1XPlxsCDbhiZft2Wg4GvI6olt7bu_0dJj/view?usp=sharing Solution 12 : Link: https://drive.google.com/file/d/1VCbhv4IdmnMzXT2JVAnxPF66oFyXj5qG/view?usp=sharing
Happy Learning!
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care : Live Interactive session - 3
Dear Learner,
The Course Instructor of "An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care"
(IIT Kharagpur), will be available in a live session on YouTube on the date and time mentioned below. You will have the opportunity to interact with the faculty and ask questions by posting in the YouTube live chat box.
Date: 18 /04 /2024
Time: 4 :00 Hrs.
Link for YouTube live session : https://youtube.com/live/AC7_7t7upSk?feature=share
Feel free to submit your queries ahead of the live session by clicking on the provided link. The faculty will address your questions during the live session : https://docs.google.com/spreadsheets/d/1StRTjxn_gwNXysCs49hGZGSA2NpM-op3TWt1nJMUWpE/edit?resourcekey#gid=1354436855
**We would also like to hear from you after the session, therefore we request you to please share your thoughts in the forum. Learners are encouraged to visit bit.ly/NPTELLIVE for updates regarding live sessions.
-NPTEL Team
Exam Format - April, 2024!!
Dear Candidate, ****This is applicable only for the exam registered candidates**** Type of exam will be available in the list: Click Here You will have to appear at the allotted exam center and produce your Hall ticket and Government Photo Identification Card (Example: Driving License, Passport, PAN card, Voter ID, Aadhaar-ID with your Name, date of birth, photograph and signature) for verification and take the exam in person. You can find the final allotted exam center details in the hall ticket. The hall ticket is yet to be released. We will notify the same through email and SMS. Type of exam: Computer based exam (Please check in the above list corresponding to your course name) The questions will be on the computer and the answers will have to be entered on the computer; type of questions may include multiple choice questions, fill in the blanks, essay-type answers, etc. Type of exam: Paper and pen Exam (Please check in the above list corresponding to your course name) The questions will be on the computer. You will have to write your answers on sheets of paper and submit the answer sheets. Papers will be sent to the faculty for evaluation. On-Screen Calculator Demo Link: Kindly use the below link to get an idea of how the On-screen calculator will work during the exam. https://tcsion.com/ OnlineAssessment/ ScientificCalculator/ Calculator.html NOTE: Physical calculators are not allowed inside the exam hall. Thank you! -NPTEL Team
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Week 12 videos are live now!!
Dear Learners,
The lecture videos for Week 12 for the course An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care is made available early for viewing to get an idea about the content but the actual start date remains unchanged.
The lectures can be accessed using the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=119&lesson=121
The other lectures of this week are accessible from the navigation bar to the left. Please remember to login into the website to view contents (if you aren't logged in already).
Please use the discussion forums if you have any questions on this module.
--NPTEL Team
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Week 12 assignment is live now!!
Dear Learners,
The assignment 12 for Week 12 for the course An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care is made available early for viewing to get an idea about the assignments but the actual start date of the course remains unchanged.
Assignment 12 can be accessed using the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=119&assessment=120
The other Assignment 12 is accessible from the navigation bar to the left under Week 12 . Please remember to login into the website to view contents (if you aren't logged in already).
The assignment has to be submitted on or before Wednesday, 2024-04-17 , 23:59 IST.
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Week 11 videos are live now!!
The lecture videos for Week 11 for the course An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care is made available early for viewing to get an idea about the content but the actual start date remains unchanged.
The lectures can be accessed using the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=111&lesson=112
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Week 11 assignment is live now!!
The assignment 11 for Week 11 for the course An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care is made available early for viewing to get an idea about the assignments but the actual start date of the course remains unchanged.
Assignment 11 can be accessed using the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=111&assessment=118
The other Assignment 1 is accessible from the navigation bar to the left under Week 1. Please remember to login into the website to view contents (if you aren't logged in already).
The assignment has to be submitted on or before Wednesday, 2024-04-10 , 23:59 IST.
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Week 10 assignment is live now!!
The assignment 10 for Week 10 for the course An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care is made available early for viewing to get an idea about the assignments but the actual start date of the course remains unchanged.
Assignment 10 can be accessed using the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=102&assessment=103
The assignment has to be submitted on or before Wednesday, 2024-04-03 , 23:59 IST.
Important Notice:No CHANGE in NPTEL Exam Schedule for April 2024
Dear Student,
We wanted to take a moment to address an important matter regarding the upcoming election dates and their potential impact on your exam schedule.
- None of the election dates clash with scheduled exam dates. If we schedule additional dates, we will ensure they again do not clash with elections in your state.
- Hence this is to confirm that there will be no changes to the exam dates and they are the same as previously scheduled. We may have exams in some cities on April 19 and April 26 depending on seat availability on scheduled dates. But again this will be done ensuring we don't conduct exams on election dates in your state.
- Your academic progress and success remain our top priority, and we are committed to maintaining the integrity of the examination process.
- We have more than 6 lakh learners registered for April exams and logistics has been a huge challenge. We understand that some of you may need to travel to your native cities to participate in the voting process. Please remember that you selected your exam cities during registration, and it is crucial that you return to these cities to take your exams as scheduled. Since hall ticket and center allocation is under process, exam cities selected by you during exam registration cannot be changed now.
Hence we kindly request that you make the necessary arrangements to ensure you can both exercise your right to vote and fulfill your academic obligations.
Warm Regards,
NPTEL Team.
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care : Live Interactive session - 2
Date: 27 /03/2024
Time: 3 :00 Hrs.
Link for YouTube live session : https://youtube.com/live/IhbNmIPH0ns?feature=share
Feel free to submit your queries ahead of the live session by clicking on the provided link. The faculty will address your questions during the live session : https://docs.google.com/spreadsheets/d/1pnFQh_YQIY1l7dhHsM9vdo3vPtxzZ2w7-Ai9kBaekF0/edit?resourcekey#gid=130423141
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Week 10 videos are live now!!
The lecture videos for Week 10 for the course An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care is made available early for viewing to get an idea about the content but the actual start date remains unchanged.
The lectures can be accessed using the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=102&lesson=109
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Assignment- 8. Solution Released
The Assignment- 8 of Week- 8 Solution for the course An Overview on Maternal Health Antenatal,Intranatal and Postnatal Care has been released in the portal. Please go through the solution and in case of any doubt post your queries in the forum.
Solution 8 : Link: https://drive.google.com/file/d/1srTFUVmmLuM6m9fFC7adczQGqwWFl1qg/view?usp=sharing
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Week 9 content is live now!!
Dear Students
The lecture videos for Week 9 have been uploaded for the course An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care . The lectures can be accessed using the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=91&lesson=93
Assignment 9 for Week 9 is also released and can be accessed from the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=91&assessment=92
The assignment has to be submitted on or before Wednesday, 2024-03-27 , 23:59 IST.
As we have done so far, please use the discussion forums if you have any questions on this module.
Note : Please check the due date of the assignments in the announcement and assignment page if you see any mismatch write to us immediately.
Thanks and Regards,
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Assignment-5,6 & 7. Solution Released
The Assignment- 5,6 & 7 of Week- 5,6 & 7 Solution for the course An Overview on Maternal Health Antenatal,Intranatal and Postnatal Care has been released in the portal. Please go through the solution and in case of any doubt post your queries in the forum.
Solution 5 : Link: https://drive.google.com/file/d/1tjtYwqUoaKiktdoY5sOkvVSv--8nTB6N/view?usp=sharing Solution 6 : Link: https://drive.google.com/file/d/19v7xsoOUToNOFqS4O8gA93HzTGXJAUAK/view?usp=sharing Solution 7 : Link: https://drive.google.com/file/d/1P3OO7EAbAC_OZRW3vzu-KXhUmR6TvOaw/view?usp=sharing
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care : Live Interactive session - 1
Date: 13 /03/2024
Link for YouTube live session : https://youtube.com/live/3AxNpNaSAUY?feature=share
Feel free to submit your queries ahead of the live session by clicking on the provided link. The faculty will address your questions during the live session : https://docs.google.com/spreadsheets/d/1JAUO4Mu5MzFwhDrM_Nj8V_43vw3KSfqFHKaKypbPCBk/edit?resourcekey#gid=502418258
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Week 8 videos are live now!!
The lecture videos for Week 8 for the course An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care is made available early for viewing to get an idea about the content but the actual start date remains unchanged.
The lectures can be accessed using the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=79&lesson=80
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Week 8 assignment is live now!!
The assignment 8 for Week 8 for the course An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care is made available early for viewing to get an idea about the assignments but the actual start date of the course remains unchanged.
Assignment 1 can be accessed using the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=79&assessment=83
The other Assignment 8 is accessible from the navigation bar to the left under Week 8 . Please remember to login into the website to view contents (if you aren't logged in already).
The assignment has to be submitted on or before Wednesday, 2024-03-20 , 23:59 IST.
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Week 7 content is live now!!
The lecture videos for Week 7 have been uploaded for the course An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care . The lectures can be accessed using the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=70&lesson=72
Assignment 7 for Week 7 is also released and can be accessed from the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=70&assessment=71
The assignment has to be submitted on or before Wednesday, 2024-03-13 , 23:59 IST.
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Week 6 content is live now!!
The lecture videos for Week 6 have been uploaded for the course An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care . The lectures can be accessed using the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=62&lesson=64
Assignment 6 for Week 6 is also released and can be accessed from the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=62&assessment=63
The assignment has to be submitted on or before Wednesday, 2024-03-06 , 23:59 IST.
NPTEL: Exam Registration date is extended for 12 week courses of Jan 2024!
- No further extension will be provided.
- This extension is only applicable for 12-week courses.
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Assignment- 4. Solution Released
The Assignment- 4 of Week- 4 Solution for the course An Overview on Maternal Health Antenatal,Intranatal and Postnatal Care has been released in the portal. Please go through the solution and in case of any doubt post your queries in the forum.
Solution 4 : Link: https://drive.google.com/file/d/11ICAlaFTOBQQVfVc_TzOyvYryYMHkJGH/view?usp=sharing
Reminder: NPTEL: Exam Registration is date is extended for Jan 2024 courses!
Dear Learner, The exam registration for the Jan 2024 NPTEL course certification exam is extended till February 23, 2024 - 05.00 P.M . CLICK HERE to register for the exam Choose from the Cities where exam will be conducted: Exam Cities Click here to view Timeline and Guideline : Guideline For further details on registration process please refer the previous announcement in the course page. -NPTEL Team
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Week 5 content is live now!!
The lecture videos for Week 5 have been uploaded for the course An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care . The lectures can be accessed using the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=53&lesson=55
Assignment 5 for Week 5 is also released and can be accessed from the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=53&assessment=54
The assignment has to be submitted on or before Wednesday, 2024-02-28 , 23:59 IST.
Dear Learner, The exam registration for the Jan 2024 NPTEL course certification exam is extended till February 20, 2024 - 05.00 P.M . CLICK HERE to register for the exam Choose from the Cities where exam will be conducted: Exam Cities Click here to view Timeline and Guideline : Guideline For further details on registration process please refer the previous announcement in the course page. -NPTEL Team
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Assignment-1,2 & 3. Solution Released
The Assignment- 1,2 &3 of Week- 1,2 &3 Solution for the course An Overview on Maternal Health Antenatal,Intranatal and Postnatal Care has been released in the portal. Please go through the solution and in case of any doubt post your queries in the forum.
Solution 1 : Link: https://drive.google.com/file/d/11yEO3qR1KudtlkDr_L_AXforiPWIlk97/view?usp=sharing Solution 2 : Link: https://drive.google.com/file/d/11yEO3qR1KudtlkDr_L_AXforiPWIlk97/view?usp=sharing Solution 3 : Link: https://drive.google.com/file/d/11yEO3qR1KudtlkDr_L_AXforiPWIlk97/view?usp=sharing
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Week 4 content is live now!!
The lecture videos for Week 4 have been uploaded for the course An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care . The lectures can be accessed using the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=43&lesson=45
Assignment 4 for Week 4 is also released and can be accessed from the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=43&assessment=44
The assignment has to be submitted on or before Wednesday, 2024-02-21 , 23:59 IST.
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Week 3 content is live now!!
The lecture videos for Week 3 have been uploaded for the course An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care . The lectures can be accessed using the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=36&lesson=38
Assignment 3 for Week 3 is also released and can be accessed from the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=36&assessment=37
The assignment has to be submitted on or before Wednesday, 2024-02-14 , 23:59 IST.
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Week 2 content is live now!!
The lecture videos for Week 2 have been uploaded for the course An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care . The lectures can be accessed using the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=29&lesson=35
Assignment 2 for Week 2 is also released and can be accessed from the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=29&assessment=30
The assignment has to be submitted on or before Wednesday, 2024-02-07 , 23:59 IST.
Reminder: NPTEL: Exam Registration is open now for Jan 2024 courses!
Dear Learner,
Here is the much-awaited announcement on registering for the Jan 2024 NPTEL course certification exam.
1. The registration for the certification exam is open only to those learners who have enrolled in the course.
2. If you want to register for the exam for this course, login here using the same email id which you had used to enroll to the course in Swayam portal. Please note that Assignments submitted through the exam registered email id ALONE will be taken into consideration towards final consolidated score & certification.
3 . Date of exam: Apr 28, 2024
CLICK HERE to register for the exam.
Choose from the Cities where exam will be conducted: Exam Cities
4. Exam fees:
If you register for the exam and pay before Feb 12, 2024 - 5:00 PM, Exam fees will be Rs. 1000/- per exam .
5. 50% fee waiver for the following categories:
Students belonging to the SC/ST category: please select Yes for the SC/ST option and upload the correct Community certificate.
Students belonging to the PwD category with more than 40% disability: please select Yes for the option and upload the relevant Disability certificate.
6. Last date for exam registration: Feb 16, 2024 - 5:00 PM (Friday).
7. Between Feb 12, 2024 - 5:00 PM & Feb 16, 2024 - 5:00 PM late fee will be applicable.
8. Mode of payment: Online payment - debit card/credit card/net banking/UPI.
9. HALL TICKET:
The hall ticket will be available for download tentatively by 2 weeks prior to the exam date. We will confirm the same through an announcement once it is published.
10. FOR CANDIDATES WHO WOULD LIKE TO WRITE MORE THAN 1 COURSE EXAM:- you can add or delete courses and pay separately – till the date when the exam form closes. Same day of exam – you can write exams for 2 courses in the 2 sessions. Same exam center will be allocated for both the sessions.
11. Data changes:
Last date for data changes: Feb 16, 2024 - 5:00 PM :
We will charge an additional fee of Rs. 200 to make any changes related to name, DOB, photo, signature, SC/ST and PWD certificates after the last date of data changes.
The following 6 fields can be changed (until the form closes) ONLY when there are NO courses in the course cart. And you will be able to edit those fields only if you: -
REMOVE unpaid courses from the cart And/or - CANCEL paid courses
1. Do you come under the SC/ST category? *
2. SC/ST Proof
3. Are you a person with disabilities? *
4. Are you a person with disabilities above 40%?
5. Disabilities Proof
6. What is your role?
Note: Once you remove or cancel a course, you will be able to edit these fields immediately.
But, for cancelled courses, refund of fees will be initiated only after 2 weeks.
12. LAST DATE FOR CANCELLING EXAMS and getting a refund: Feb 16, 2024 - 5:00 PM
13. Click here to view Timeline and Guideline : Guideline
Domain Certification
Domain Certification helps learners to gain expertise in a specific Area/Domain. This can be helpful for learners who wish to work in a particular area as part of their job or research or for those appearing for some competitive exam or becoming job ready or specialising in an area of study.
Every domain will comprise Core courses and Elective courses. Once a learner completes the requisite courses as per the mentioned criteria, you will receive a Domain Certificate showcasing your scores and the domain of expertise. Kindly refer to the following link for the list of courses available under each domain: https://nptel.ac.in/domains
Outside India Candidates
Candidates who are residing outside India may also fill the exam form and pay the fees. Mode of exam and other details will be communicated to you separately.
Thanks & Regards,
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Week 1 content is live now!!
The lecture videos for Week 1 have been uploaded for the course An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care . The lectures can be accessed using the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=20&lesson=24
Assignment 1 for Week 1 is also released and can be accessed from the following link: https://onlinecourses.nptel.ac.in/noc24_ge34/unit?unit=20&assessment=23
An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care - Assignment-0-RELEASED
We welcome you all to this course. The assignment 0 for the course An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care has been released. This assignment is based on a prerequisite of the course. Kindly note that marks obtained in this assignment will not be considered for the final assessment. You can find the assignment under Week 0 unit on the left-hand side of your screen. You can submit the assignment multiple times. All the best !!
NPTEL: Exam Registration is open now for Jan 2024 courses!
An overview on maternal health antenatal, intranatal and postnatal care: welcome to nptel online course - jan 2024.
- Every week, about 2.5 to 4 hours of videos containing content by the Course instructor will be released along with an assignment based on this. Please watch the lectures, follow the course regularly and submit all assessments and assignments before the due date. Your regular participation is vital for learning and doing well in the course. This will be done week on week through the duration of the course.
- Please do the assignments yourself and even if you take help, kindly try to learn from it. These assignments will help you prepare for the final exams. Plagiarism and violating the Honor Code will be taken very seriously if detected during the submission of assignments.
- The announcement group - will only have messages from course instructors and teaching assistants - regarding the lessons, assignments, exam registration, hall tickets, etc.
- The discussion forum (Ask a question tab on the portal) - is for everyone to ask questions and interact. Anyone who knows the answers can reply to anyone's post and the course instructor/TA will also respond to your queries.
- Please make maximum use of this feature as this will help you learn much better.
- If you have any questions regarding the exam, registration, hall tickets, results, queries related to the technical content in the lectures, any doubts in the assignments, etc can be posted in the forum section
- The course is free to enroll and learn from. But if you want a certificate, you have to register and write the proctored exam conducted by us in person at any of the designated exam centres.
- The exam is optional for a fee of Rs 1000/- (Rupees one thousand only).
- Date and Time of Exams: April 28, 2024 Morning session 9am to 12 noon; Afternoon Session 2 pm to 5 pm.
- Registration URL: Announcements will be made when the registration form is open for registrations.
- The online registration form has to be filled and the certification exam fee needs to be paid. More details will be made available when the exam registration form is published. If there are any changes, it will be mentioned then.
- Please check the form for more details on the cities where the exams will be held, the conditions you agree to when you fill the form etc.
- Once again, thanks for your interest in our online courses and certification. Happy learning.
A project of

In association with


COMMENTS
The days and weeks following childbirth—the postnatal period—are a critical phase in the lives of mothers and newborn babies. Most maternal and infant deaths occur in the first month after birth: almost half of postnatal maternal deaths occur within the first 24 hours,1 and 66% occur during the first week.2 In 2013, 2.8 million newborns ...
In this session we review the key information to be communicated to women who have just given birth and their partners and/or families. This covers general care of both the mother and the baby as well as danger signs in the postnatal period. Special mention is made for supporting women with depression.This topic is used to practise the skills of facilitating family and group support and ...
Background. Postnatal Care (PNC) is one of the care packages that make up the continuum of care for mothers and babies globally [1, 2].A significant number of maternal deaths still occur during the postnatal period and an estimated 2.8 million babies die in the first month of life (neonatal death) [3, 4].Neonatal deaths account for up to 52% of all deaths in children under-5 years of age [].
WHO Recommendations on Postnatal Care of the Mother and Newborn. Geneva: World Health Organization; 2013 Oct. WHO Recommendations on Postnatal Care of the Mother and Newborn. ... Konefal Gallagher M. Assignment to a hospital-based breastfeeding clinic and exclusive breastfeeding among immigrant Hispanic mothers: a randomized, controlled trial.
The guidelines focus on postnatal care of mothers and newborns in resource-limited settings in low- and middle-income countries. The critical maternal health outcome considered was maternal morbidity (including haemorrhage, infections, anaemia and depression). The two critical neonatal outcomes were neonatal mortality and morbidity.
The postpartum period—the 12 weeks following the birth of a child—is an important time for your health. As you recover from childbirth and learn to care for your baby, your postpartum check-ups will help make sure you are. healing physically, mentally, and emotionally. feeling good about your health and your baby's care.
Optimal care during the antenatal and postnatal phases of the life cycle is a potentially positive determinant of health elsewhere in the continuum. A successful transition from the antenatal to the postnatal period requires early detection, optimal management, and prevention of disease; health promotion; birth preparedness; and complication readiness. Women, their babies, and families need ...
person-centred care at every contact, in accordance with a human rights-based approach. The WHO postnatal care model places the woman- newborn dyad at the centre of care (Fig. 1). The foundation of this postnatal care model is a minimum of four postnatal care contacts. In particular, the GDG considered the first two weeks after birth to be a key
WHO recommendations on maternal and newborn care for a positive postnatal experience: executive summary. 28 March 2022 | Executive summary. Download (243.9 kB) Overview . The recommendations in this guideline are intended to inform the development of relevant national and subnational health policies, clinical protocols and programmatic guides ...
1.Labor,Obstetric 2.Delivery,Obstetric 3.Prenatal care 4.Perinatal care — methods 5.Postnatal care - methods 6.Pregnancy complications - diagnosis 7.Pregnancy complications - therapy 8.Manuals I.World Health Organization. ISBN 92 4 159084 X (NLM classification: WQ 175)
Unit 2: Postpartum Assessment and Care 22 Postpartum and Newborn Care: A Self-study Manual PRIME 1999 First-time mothers and their babies Figure 6: Sometimes the pelvic opening of a young mother is not large enough for her baby. Illustration source: Klein S, p. 238. Why first-time mothers are physically at risk Many first-time mothers are young.
3.3 Care of the Newborn. During the early postpartum period, care of the newborn usually involves celebrating and rejoicing with the family and respecting and supporting their needs. The care is based on nurturing the developing mother-baby-family relationship and caring for mother and baby as a unit.
The early postnatal period is a dangerous time for both mother and baby where morbidity and mortality are highly prevalent if proper care is not done. Post natal care (PNC) knowledge has significant role in reducing such complications. In this study, the knowledge of postpartum mothers on PNC and its determinants were determined. A cross-sectional quantitative study was conducted in postpartum ...
Timely interventions in the postnatal period are important for reducing newborn mortality, and early home visits to provide postnatal care are recommended. There has been limited success in achieving timely visits, and a better understanding of the realities of programmes is needed if improvements are to be made. We explored barriers and facilitators to timely postnatal visits through 20 ...
Abstract. High quality postnatal care is key for the health and wellbeing of women after childbirth and. their newborns. In 2022, the World Health Organization (WHO) published global recommen ...
Getting early and regular prenatal care improves the chances of a healthy pregnancy. This care can begin even before pregnancy with a pre-pregnancy care visit to a health care provider. Having a healthy pregnancy is one of the best ways to promote a healthy birth. Getting early and regular prenatal care improves the chances of a healthy pregnancy.
Lecture4:Postnatal Care Lecture5:Post- Partum Contraception. Week 12: ... YOU WILL BE ELIGIBLE FOR A CERTIFICATE ONLY IF AVERAGE ASSIGNMENT SCORE >=10/25 AND EXAM SCORE >= 30/75. If one of the 2 criteria is not met, you will not get the certificate even if the Final score >= 40/100.
4 Postnatal Care, with a Focus on Home Visitation 3. Community health workers are not all the same. Community health workers (CHWs) are often discussed as if they are a homogenous group or in terms of a single characteristic, such as whether they are paid or unpaid. However, there were important differences across the trials, including selection
Put your thumb and first finger opposite each other on your areola (coloured area surrounding your nipple) in the shape of a 'C'. 5. Gently squeeze your thumb and finger together repeating in a rhythmic action. 6. When the flow stops move your finger and thumb to another position and repeat steps 4-6 7.
Module 3. Antenatal, intrapartum and postnatal care. Assignment. Training course in adolescent sexual and reproductive health 2021 for WHO Eastern Mediterranean Region. February 8, 2021 - Geneva. Assignment (25 marks in total) Answer the following questions using the clues provided to review the selected aspects of the relevant documents.
The decreasing length of postnatal stay might be an important obstacle to conducting individual postnatal consultations with all women who want them. From 1999-2016, the mean length of postnatal stays in Norway decreased from 4.5 to 3.2 days for first-time mothers and from 3.9 to 2.4 days for multiparous mothers [43]. The findings of the ...
This video provide knowledge about how to make health talk on postnatal care in a simple and easy waycheck playlist for more informative videoshttps://youtub...
The assignment 10 for Week 10 for the course An Overview on Maternal Health Antenatal, Intranatal and Postnatal Care is made available early for viewing to get an idea about the assignments but the actual start date of the course remains unchanged. Assignment 10 can be accessed using the following link: https://onlinecourses.nptel.ac.in/noc24 ...